yogabook / movement physiology / pulse deficit
Contents
- 1 Circulation and vascular system
- 2 cardiac output, CO
- 2.1 Maximum oxygen uptake VO2max
- 2.2 Veins: Veins and arteries
- 2.3 Capillaries
- 2.4 Capillarisation / Capillarisation
- 2.5 Vascularisation / vascularisation
- 2.6 Hypervascularisation
- 2.7 Collaterals, anastomoses
- 2.8 Vein valves
- 2.9 Blood volumes in the systems
- 2.10 Windkessel function
- 2.11 Interstitium
- 2.12 Arteries
- 2.13 Veins
- 3 Heart
- 3.1 Pulse, heart rate
- 3.2 Pulse deficit
- 3.3 Heart rate recovery / heart rate recovery HRR
- 3.4 Pulse Wave Velocity
- 3.5 Cardiac output
- 3.6 Structure of the heart
- 3.7 Stimulus formation and conduction
- 3.8 Cardiac action: the phases
- 3.9 Wall layers of the heart
- 3.10 Coronaries
- 3.11 ECG
- 3.12 Mediastinum
- 3.13 Trachea
- 3.14 Lung
- 3.15 abdominal breathing
- 3.16 chest breathing
- 3.17 Breathing volumes
- 3.18 Respiratory muscles
Circulation and vascular system
The circulatory system is a system driven by the heart to circulate the fluid blood so that its various functions can maintain the body:
– Transporting O2 and nutrients
– Removing CO2 and metabolic and waste products
– Closure of leakages
– Immune functions
– Transport of hormones to control the body
– Heat distribution
There are two circulatory systems:
small circulation
This leads from the heart to the lungs and back and serves primarily to enrich the blood with oxygen (with simultaneous release of CO2), but also secondarily for thrombolysis and hormone activation and a
large circulation
This serves to supply the body with O2 and all other substances and cells that can be transported by the blood. Due to the size of the large circulatory system and the higher pressure required, the associated left ventricle is equipped with stronger muscles. The pressure in the large circulation must be sufficiently high to passively press most of the required substances into the corresponding regions by diffusion. The lower pressure in the lungs, on the other hand, facilitates gas diffusion (O2/CO2). The nutrients collected from the digestive organs via the venous portal vein are transported via the liver into the venous system and thus into the entire body. Waste products produced during metabolism are transported to the liver for detoxification or to the kidneys for excretion.
In all circulatory systems, the vessels leading away from the heart are called arteries, all others (those leading to the heart and not connected to the heart) are called veins. The cross-section of the arterial vessels decreases from the heart towards the periphery; they eventually merge into the smaller arterioles and finally into myriads of parallel capillaries, which in turn unite to form venules and later veins, the cross-section of which increases towards the heart. The capillaries are only large enough for individual erythrocytes to pass through, which drastically improves their ability to release oxygen and absorb CO2 compared to larger cross-sections.
Coronaries
The two arteries Arteria coronaria sinistra (LCA) and Arteria coronaria dextra (RCA), which supply the heart muscle with their branches (rami), are called coronary arteries or coronaries. Arteriosclerosis of the coronaries is known as coronary sclerosis and causes coronary heart disease (CHD) with the possible consequences angina pectoris and heart attack.
TPR (total peripheral resistance)
The resistance of the vascular system to cardiac force depends mostly on the TPR (total peripheral resistance) of the capillaries and arterioles. The TPR depends on neurological and hormonal factors, the pH value and the NO concentration. The exact composition of the TPR is:
– large and medium arteries: 19%
– smaller arteries and arterioles: 47% (regulable resistance vessels)
– capillaries: 27 %
– Venules: 4 %
– Medium and large veins: 3 %
The total resistance that the heart experiences with the is also referred to as afterload.
cardiac output, CO
In physiology, the minute is typically used as the unit of time, so that the term cardiac output (HMV) is used. This is the volume that the heart ejects in one minute. It must be assumed that physiologically (in healthy people without shunts (see e.g. on doccheck.com) and septal defects (see also e.g. on doccheck.com), the ejection of the right heart corresponds exactly to that of the left heart in the short term, as any deviation from this would mean an accumulation of blood in a circuit (pulmonary circulation or large circulation) and would no longer be compatible with life above a certain level. With a heart rate of 60 bpm and a stroke volume of 50 ml, a deviation of just 1 ml per cardiac action would correspond to an accumulation of 3 litres of blood in one of the circulatory systems. The pulmonary circulation could not absorb such a quantity of blood, and in the large circulation this would correspond to an extreme pooling of blood in the periphery, as is known from anaphylactic shock, for example. The second hour at the latest would certainly not be survivable.
In a right-to-left shunt, the cardiac output is greater than the pulmonary output, in a left-to-right shunt it is smaller.
At rest, the average cardiac output is 4.5 – 5 litres, which can be increased by a factor of 4 during exercise.
If the cardiac output is multiplied by the arterial-venous oxygen difference, the result is the VO2max per minute, whereby a healthy lung is generally not the limiting factor, but internal respiration and metabolism are decisive in determining how much of the inhaled oxygen is utilised.
Maximum oxygen uptake VO2max
VO2max refers to a person’s maximum oxygen uptake. In training physiology, it is usually not the absolute VO2max that is used, but rather the VO2max relative to body weight. This value depends primarily on the ejection capacity (cardiac output) of the heart and only secondarily – except in pathological cases – on the lungs or internal respiration. VO2max indicates an upper limit for a person’s endurance performance; how far this can be achieved depends on many other factors, many of which can be improved through endurance training. Among other things, this training attempts to bring the anaerobic threshold closer to the performance corresponding to VO2max. VO2max decreases by around 10% with every decade of life from the age of 40, so that in old age it can fall below the frailty line of 18 (men) or 16 (women). Untrained people typically have values of 35 ml/min/kg (women) or 40 ml/min/kg (men) by middle age (men). Competitive athletes achieve values of up to 80 ml/min/kg through training and weight optimisation. VO2max is determined quite accurately in a non-invasive stress test using special equipment, but there are several ways to obtain good estimates:
- Fick’s principle: VO2max = HMV * (arterial oxygen content CaO2 – venous oxygen content CvO2). This measurement is invasive and the most accurate.
- Uth–Sørensen–Overgaard–Pedersen estimate: VO2max = 15,3 * HXmax / resting heart rate. This estimate requires a correct measurement of the resting heart rate (RHR). There are many false positive factors for this measurement.
- Cooper-Test: VO2max = (v * 12m – 505m) / 44,7m = (s-505) / 44,7
- Rockport Walk Test (1-mile walk test): VO2max=132.853 − (0.1695×weight {kg}) − (0.3877×age) + (6.315×gender [m:1, f:0]) −(3.2649×time {min}) − (0.1565×HR {bpm})
The following tables can be calculated from the formula for the Cooper test:
The following tables show the maximum oxygen uptake VO2max determined by the Cooper Institute in deciles, as it can be achieved by both sexes of different ages on a treadmill or ergometer. The decline with age results solely from the decrease in HRmax.
Running/Treadmill – Men:
| Alter | 10 % | 20 % | 30 % | 40 % | 50 % | 60 % | 70 % | 80 % | 90 % |
|---|---|---|---|---|---|---|---|---|---|
| 20…29 | 34,6 | 37,8 | 41,0 | 42,6 | 44,2 | 47,4 | 49,0 | 52,1 | 55,1 |
| 30…39 | 33,0 | 36,2 | 39,4 | 41,0 | 42,6 | 44,2 | 47,4 | 50,6 | 52,1 |
| 40…49 | 31,4 | 34,6 | 36,2 | 39,4 | 41,0 | 44,2 | 45,8 | 49,0 | 50,6 |
| 50…59 | 29,9 | 31,4 | 34,6 | 36,2 | 37,8 | 39,4 | 41,0 | 44,2 | 49,0 |
| over 60 | 26,7 | 28,3 | 31,4 | 33,0 | 34,6 | 36,2 | 37,8 | 41,0 | 44,2 |
Running/Treadmill – Women:
| Alter | 10 % | 20 % | 30 % | 40 % | 50 % | 60 % | 70 % | 80 % | 90 % |
|---|---|---|---|---|---|---|---|---|---|
| 20…29 | 29,4 | 31,6 | 33,8 | 35,5 | 37,4 | 39,5 | 41,1 | 44,0 | 47,0 |
| 30…39 | 27,4 | 29,9 | 32,3 | 31,8 | 35,2 | 36,7 | 38,8 | 41,0 | 44,7 |
| 40…49 | 25,6 | 28,0 | 29,7 | 31,6 | 33,3 | 35,1 | 36,7 | 38,9 | 42,4 |
| 50…59 | 23,7 | 25,5 | 27,3 | 28,7 | 30,2 | 31,4 | 32,9 | 35,2 | 38,1 |
| over 60 | 21,7 | 23,7 | 24,9 | 26,6 | 27,5 | 29,1 | 30,2 | 32,3 | 34,6 |
Cycling – Men
| Alter | 10 % | 20 % | 30 % | 40 % | 50 % | 60 % | 70 % | 80 % | 90 % |
|---|---|---|---|---|---|---|---|---|---|
| 20…29 | 32,9 | 35,91 | 38,95 | 40,5 | 41,9 | 45,0 | 46,55 | 49,5 | 52,3 |
| 30…39 | 31,3 | 34,4 | 37,4 | 38,9 | 40,5 | 41,9 | 46,0 | 48,1 | 49,5 |
| 40…49 | 29,8 | 32,9 | 34,4 | 37,4 | 40,5 | 41,9 | 43,5 | 46,6 | 48,1 |
| 50…59 | 28,4 | 29,8 | 32,9 | 34,4 | 35,9 | 37,4 | 41,9 | 41,9 | 46,6 |
| over 60 | 25,4 | 26,9 | 29,8 | 31,3 | 32,9 | 34,4 | 35,9 | 41,9 | 41,9 |
Cycling – Women
| Alter | 10 % | 20 % | 30 % | 40 % | 50 % | 60 % | 70 % | 80 % | 90 % |
|---|---|---|---|---|---|---|---|---|---|
| 20…29 | 26,9 | 31,3 | 31,3 | 34,4 | 35,9 | 37,4 | 38,9 | 42,0 | 46,6 |
| 30…39 | 25,4 | 28,4 | 31,3 | 31,3 | 32,9 | 34,4 | 37,4 | 38,9 | 43,5 |
| 40…49 | 23,8 | 26,9 | 28,4 | 31,3 | 31,3 | 32,9 | 34,4 | 37,4 | 40,5 |
| 50…59 | 20,8 | 23,8 | 25,4 | 26,9 | 28,4 | 29,8 | 31,3 | 32,9 | 35,9 |
| over 60 | 19,3 | 20,8 | 22,3 | 23,8 | 25,4 | 26,9 | 29,8 | 31,3 | 32,9 |
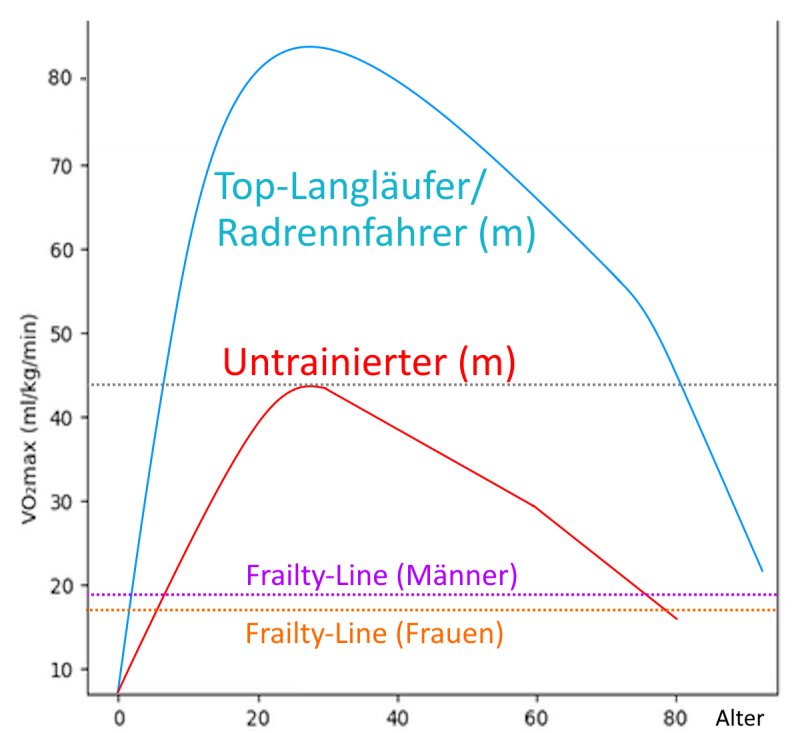
Further data: VO2max usually peaks at around 25 years of age. After that, it declines by approx. 0.5 – 1 ml/kg/min without training, and somewhat more steeply from around 75 years of age. The blue curve in the following model graph shows an elite athlete, where the maximum is over 85 (cyclist) or over 90 (runner). Well-trained amateur athletes with good genetic disposition achieve values of up to 70. The red curve shows a typical progression for sedentary life, no exercise to moderate exercise. The decline in both curves is due to falling HRmax, decreasing stroke volume SVmax, sarcopenia and decreasing diffusion capacity a-vO2-Diff. The data suggests that a former elite long-distance runner aged 70 still has approximately the same VO2max as a completely untrained person of the same age and, at his peak, had almost twice the VO2max of an untrained person of the same age. VO2max is approximately 10-15% lower in women than in men. With an adequate training programme, predominantly sedentary non-athletes can increase their VO2max by 15-20% within 6 months.
Veins: Veins and arteries
The veins are also known as veins, the arteries as arteries, as the blood beat or pulse caused by the contraction of the heart can be clearly felt in them; In contrast, there is no stroke in the venous system and the pressure is on average lower, but above all strongly gravity-dependent, in anatomically zero, i.e. greatest in the feet and lower legs. Pressure and flow velocity in the arterial system are around 120/80 mmHg (millimetres of mercury column, measured at heart level without the influence of hydrostatic blood pressure! These values correspond to 160 or 106 mbar or hPa pressure in addition to the ambient pressure) and are constant and equally higher than in the venous system.
Of course, the position-dependent hydrostatic blood pressure, approx. 100 mbar / m, must be added to the arterial or venous blood pressure measured at heart level. The venous pressure normally only becomes positive below the heart in an upright position. In the headstand, the zero point of venous pressure lies in the femoral veins. The hydrostatic indifference point, i.e. the clear fixed point for all changes in the body’s position, is around 5-10 cm below the diaphragm.
Because of the pressure, the arteries are equipped with a thicker contractile muscle layer for pressure regulation, which is particularly pronounced in the area further away from the heart: it allows vasoconstriction (vasoconstriction) or vasodilation (vasodilation).
The blood pressure drops towards the periphery as the vessels become smaller, i.e. the vascular resistance increases:
Aorta and large arteries: 100 mmHg, arterial branches 40 mmHg, capillaries 25 mmHg, venules 20 mmHg. In the pulmonary circulation, the pressures are much lower: pulmonary artery 14 mmHg, pulmonary veins 7 mmHg.
Capillaries
In the capillaries, an exchange of fluids, nutrients, electrolytes, hormones, gases and other substances between blood and tissue takes place in both directions, which is why, like the veins, they are only equipped with a thin vessel wall (endothelium only) that is permeable (selectively permeable) to low-molecular substances. Due to the size of the pores in the membrane of the capillaries, cells and, for the most part, proteins remain in the blood, while O2, fluid and small molecules are squeezed out to the interstitium (intercellular space), which is under lower pressure. In the course of the capillary passage, the blood pressure continues to drop. The lower blood pressure and the now higher colloid osmotic pressure (ability of proteins to bind water) then favours the venous leg to absorb fluid with substances to be transported away. The amount of fluid absorbed by the venous limb is usually smaller than the amount released by the arterial limb, the rest is then transported away with the lymph. If the blood contains too little protein, for example due to malnutrition, MAS or protein loss via the kidneys, oedema results due to the low colloid osmotic pressure, as too much fluid remains in the tissues. The same applies if the permeability of the membrane is pathologically increased and proteins leak into the tissue. Of course, oedema can also be caused by inadequate venous return transport, for example due to insufficient venous valves.
In three organs (liver, spleen, bone marrow) the capillaries are dilated to sinosoids with discontinuous endothelium. The venules can regulate the vascular tension via a thin muscle layer and thus form a blood reservoir; the veins have very little musculature. The second disposal of the capillary area by the lymph transports hydrophobic substances (proteins and lipids from the digestive organs) and cells, which flows very slowly towards the right heart. Like veins, lymphatic vessels have valves.
The lymph transports only 1/10 of the fluid produced in the tissues (2-4 litres / d compared to 7000 – 8000 litres of blood), it returns to the venous blood via the ductus thoracicus (thoracic duct) in the left venous angle (confluence of the subclavian vein and internal jugular vein to form the brachiocephalic vein) shortly before the right heart. The lymph has an important function in the immune system because it transports pathogens to the lymph nodes, where special T and B lymphocytes react to the pathogens, multiply and migrate from there into the blood. Despite the low flow volume and speed, the lymph must not be neglected: if lymph ducts are blocked or lymph nodes are resected, this results in lymphoedema.
Capillarisation / Capillarisation
Capillarisation is the term used to describe the permeation of muscles with tiny capillary vessels that supply them with blood. The degree of capillarisation is not a fixed, genetically determined quantity, but is increased by regular endurance sports or repeated, more intensive isometric contraction. Capillarisation is an important aspect of vascularisation. Depending on the author, capillarisation also refers to the process of forming new capillaries.
Vascularisation / vascularisation
Vascularisation is the term used to describe the permeation of muscles with small supplying vessels. The degree of vascularisation is not a fixed, genetically determined quantity, but is increased by regular endurance sports or repeated, more intensive isometric contractions, which stimulate angiogenesis in order to better supply the muscle with oxygen in real time. In the area of capillaries, this is also referred to as capillarisation. The term vascularisation is not only used for muscles, but also for other organs. Depending on the car, vascularisation also refers to the process of the formation of new small vessels. Hypervascularisation, on the other hand, usually refers to a pathological proliferation of small vessels, for example in the context of inflammations, injuries or degenerative events; it is also referred to as neovascularisation.
Hypervascularisation
Hypervascularisation usually refers to a pathological proliferation of small vessels, for example in the context of inflammation, injuries or degenerative events, i.e. increased vascularisation for pathological reasons; it is also referred to as neovascularisation. Hypervascularisation reflects an increased metabolic requirement of the tissue, which can be caused by wound healing, chronic inflammation or malignant tumours.
Collaterals, anastomoses
Neighbouring blood vessels with the same target area are referred to as collaterals, between which there are connections almost everywhere in the body (anastomoses), which can enable further supply in the event of a vessel becoming blocked, e.g. due to thrombosis. Arteries without anastomoses are called end arteries. Overlocations (occlusions) of end arteries therefore lead to ischaemia or infarction. If the anastomosis of an artery is too small to take over the complete supply, this is referred to as a functional end artery.
Vein valves
While the arterial circulation is driven by the heart, the venous return flow works quite differently: the veins contain many valve-like venous valves, which are folds in the lining of the vein that prevent blood from flowing back into the periphery. With its usually two (rarely one or three) sails, it forms a non-return valve for the blood against the intended direction of flow. In this way, they are similar to the bicuspid valve (bicuspid leaflet valve). The section of the vein between the valves is called the sinus valvulae and is more elastic than the area near the valve, which is why it tends to bulge (varicosis: varicose veins).
Venous valves are found in the veins of the extremities to guarantee the direction of flow, both in the deep veins and in the superficial veins and the perforating veins that connect them. The blood flow is guaranteed by the „muscle pump“, i.e. the repeated pressure of muscles on the sinus valvulae. Venous valves have been known since 1547 (first described by Giovanni Battista Canano).
In the legs in particular, the muscles press the blood from one segment to the other with their alternating tension, thus overcoming gravity, so that the blood finally arrives in the right heart, this is particularly successful during leg-related activities. In the trunk, without venous valves, the differences in pressure caused by breathing contribute to transport. The venous valves are therefore essential for the return flow.
Because of the venous valves, infusion or injection needles in the extremities are always placed in the course of the blood flow and not against it. Large vascular trunks such as the vena cava, the portal vein, the umbilical vein, cerebral and pulmonary veins as well as parenchymal veins do not have venous valves. In the abdomen, with its significantly shorter distance compared to the leg, the return transport occurs mainly through pressure changes caused by abdominal breathing and the resulting alternating intra-abdominal pressure. Venous valves are important not only because of the risk of varicosis, but above all because of the risk of coagulation of the blood due to the stasis factor from the Virchow triad, i.e. blood flow that is too slow. In the lymphatic vessels of the extremities there is an analogue, the valvulae lymphaticae (lymphatic valves).
Venous and arterial blood differ in their colour: the arterial blood is lighter red. However, the bluish appearance of the veins is more due to the fact that the long-wave red light penetrates further into the veins and is absorbed more.
Blood volumes in the systems
Only about 20% of the blood is travelling in the arteries, postmortem (due to cardiac arrest) only about 2% due to the drop in pressure and lower elasticity, so the heart maintains the arteriovenous pressure difference throughout life. Without cardiac activity, a uniform pressure of around 6-7 mmHg is established everywhere in the supine position. Differences in blood volume due to blood loss or transfusion are primarily absorbed by the venous low-pressure system and have little effect on the arterial high-pressure system on a smaller scale.
Windkessel function
Arteries close to the heart have a windpipe function: they are quite elastic and thus stabilise the blood flow by largely absorbing blood pressure peaks. This not only serves to stabilise the blood pressure and thus reduce pathogenic effects in the vessels, but also saves energy because the otherwise intermittently higher speed would cost more energy due to the vascular resistance. Arteriosclerosis can partially or completely eliminate this function, which causes higher systolic blood pressure with corresponding consequential damage. Arteries further away from the heart are equipped with more muscle so that they can regulate blood pressure by narrowing or widening. The aorta (main artery) has a diameter of approx. 3 cm.
The pressure wave of the blood reaches approx. 6m/s in young adults and doubles in the course of life due to the decreasing wind chamber function and decreasing elasticity of the arteries, whereby the volume flow decreases due to the lower energy efficiency.
In the body, those organs whose activity is currently needed are supplied with more blood, the cardiac output (HRV) would not be sufficient for a simultaneous maximum blood flow to all organs. The „switching off“ of organs keeps the TPR and thus the RR sufficiently high and relieves the heart. This means, for example, that simultaneous digestion and high-performance sport are mutually exclusive. There are some special features for the regulation of RR and TPR and other purposes:
– blocking arteries that normally close and open in certain situations (e.g. in the penis),
– arteriovenous anastomoses: bypasses of organs,
– throttling veins, e.g. for the delayed release of nutrients from the intestine into the blood.
– Mechanisms for restricting blood flow in the event of injury
– Mechanisms for increasing blood flow in the event of inflammation
control signals for blood flow are neural, hormonal and local chemical, whereby the latter can override the first two. In the medulla oblongata, information from circulatory sensors is analysed: arterial blood pressure, pulse rate, filling pressure of the low pressure system, pH value, carbon dioxide and oxygen partial pressure of the blood. Symphaticus and Parasympathetic regulate chronotropy (change in heart rate) and inotropy (change in contraction force) as well as vascular tone.
The aortic arch and the division of the common carotid artery (carotid sinus) contain pressoreceptors that report the adjacent arterial pressure to the medulla oblongata so that it can adjust the pressure if necessary.
Interstitium
The interstitium is the space between the cells in the body’s tissues. The interstitial fluid is formed from blood that is squeezed through the pores of the membranes of the blood vessels (by blood pressure) and is therefore very similar to arterial blood in its composition, only blood cells and large molecules such as the proteins albumins and globulins are missing in the interstitial fluid, as the membrane pores are too small to allow them to pass through. The serum pressed into the tissue and altered there by the metabolic processes of the cells is reabsorbed into the bloodstream in the venous limb due to the increased osmotic pressure of the venous blood (colloid osmotic pressure is increased: high protein, low fluid).
Arteries
Arteries consist of 3 layers (from the inside to the outside):
1. Intima lies on the inside, is bare and smooth for the lowest possible resistance
2. Media or Muscularis contains ring-shaped and obliquely arranged muscle tissue, which enables a cross-sectional change of the vessel: the sympathetic nervous system causes vasoconstriction, the parasympathetic system causes vasodilation, contains even the smallest vessels to supply the muscles
3. Adventitia or Serosa made of elastic and fibrous connective tissue; it nourishes and controls the entire artery with vasa vasorum (the vessels of the vessels) and nerves (nervi vasorum).
Hormones help determine the diameter of the arteries:
Adrenaline and noradrenaline cause vasoconstriction except in the coronaries, there vasodilation
angiotensin II causes vasoconstriction (strongest vasoconstrictor of all)
Serotonin causes vasodilation in the abdominal area and vasoconstriction in the brain area (too much of it probably leads to migraine)
The blood vessels contain alpha-receptors, the heart vessels beta-receptors (this is why so-called beta-blockers are given for hormonal hypertension, so that the vasoconstrictor adrenaline, which increases blood pressure, cannot act there).
starting behind the aortic valve:
– coronary arteries :
– – A. coronaria dexter ,
– – A. coronaria sinister , which divides into the
– – – ramus circumflexus
– – – RIVA ramus interventricularis anterior
– aorta ascendens -> arcus aortae , from which it departs:
– – truncus brachiocephalicus supplies the right arm, the right brain and the right
half of the head, divides into:
– – – A. subclavia dexter -> A. axillaris -> A. brachialis ->
– – – – A. ulnaris
– – – – A. radialis the two flow together in the arcus palmaris (of which there are two: arcus palmaris
profundus, which lies deep in the hand and arcus palmaris superficialis, which lies further
palmar). From this
– – – – – Aa. digitalis the finger arteries
– – – A. carotis communis dexter merges into
– – – – A. carotis interna dexter supplies the right hemisphere of the brain
– – – – A. carotis externa dexter. carotis externa dexter supplies the right half of the face and skull
– – – A. carotis communis sinister merges into
– – – A. carotis interna sinister supplies the left half of the brain
– – – – A. carotis externa sinister supplies the left half of the face and skull
– – A. carotis communis sinister analogous to the right, lies partly in the mediastinum
– – A. subclavia sinister
– .. merges into the descending aorta, from which the
– – intercostal intercostal arteries (12 each on the right and left)
– .. passes into the abdominal cavity to the abdominal aorta, from which descend:
– – Lienal artery to the spleen (caudally)
– – Gastric artery to the stomach (to the left)
– – Hepatic artery to the liver (to the right)
– . divides in the bifurcatio aortae into
– – A. iliaca communis dexter
– – A. iliaca communis sinister both of which merge into
– – A. iliaca interna supplies the small pelvis
– – – A. iliaca externa supplies the leg and
– – – … merges into A. femoralis
– – – … merges into A. poplitea at the knee. poplitea divides after the knee into
– – – – A. peronea
– – – – A. tibialis anterior
– – – A. tibialis posterior this and the tibial artery anterior flow together in the forefoot into the
– – – – arcuate artery, from which the metatarsal arteries then branch off
Veins
Veins are blood vessels that do not transport blood away from the heart. In addition to the vessels that transport blood to the heart, these are also two vessels whose blood does not flow directly to the heart:
– the portal vein v.portae of the abdominal organs, which transports the blood of most abdominal organs to the liver and
– the portal vein v.portae of the brain between the hypothalamus and anterior pituitary gland.
Two large veins flow into the heart:
v. cava sup. , into which flows
– v. jugularis from the head
– v. subclavia , receives blood from the
– – v. axillaris , merges into
– – v. brachialis , lies ulnar, well suited for blood collection and infusion, into which flows
– – – v. radialis, deep-lying
– – – v. ulnaris, deep-lying
– – v. brachialis receives:
– – – v. basilica , superficial
– – v. axillaris receives:
– – v. cephalica , superficial, radial, well suited for blood sampling and infusion
v. cava inf. , into which it opens
– 2 v. renales (kidney)
– 3 v. hepaticae (liver)
– v. iliaca interna
– v. iliaca externa , arises from
– v. femoralis , arises from
– v. poplitea , arises from
– v. saphena parva , lies laterally, into which two lower leg veins flow
– the v. saphena magna, into which 2 further lower leg veins flow, flows into the v. femoralis
The organs spleen, pancreas, stomach, large intestine, small intestine have no direct venous connection to the v. cava inf. but are venously connected via the v. portae to the liver, which in turn is connected via 3 veins to the v. cava. inf.
Heart
The heart, cardia (Greek) cor (Latin) is a hollow muscular organ that pumps blood through the body with rhythmic contractions and thus ensures the supply of all organs.
Lies in the mediastinum, protrudes slightly to the right over the spine (pain may therefore also be felt on the right) and is the size of a fist, weighing approx. 200-350 g: man 280 – 340 g, woman: 230 – 280 g. In the course of life, the heart mass slowly increases, but the supplying vessels do not grow to the same extent, which is why 500 g is already considered pathological: critical heart weight (hypertrophy), as the supply of the myocardium, which has become so large, is no longer guaranteed by the vessels. Such severe hypertrophy cannot occur through sport. Younger people form approx. 1% new heart cells per year, older people only 0.5%.
The heart lies at a slight angle (the right side tilts downwards, the lower side forwards) on the diaphragm, to which it is fused at the bottom; in slim people it is more upright. The thymus and the pectoral bone lie in front of the heart. The heart lies in the area of the 2nd – 5th rib. At the top, the heart extends approx. 2 cm beyond the edge of the sternum.
The heart functions like a 2-way pump with valves that ensure that the blood only flows in one defined direction. It is turned to the left so that the larger part of the left heart, which pumps into the large circulation, is at the back. This is why posterior myocardial infarctions (left heart attacks) are also considered more critical.
Pulse, heart rate
With pulse the e.g. data-dl-uid=“441″>palpation or technical sensors in the peripheral blood flow, Examples are the radial pulse on the radial-palmar side of the forearm before the wrist or the carotid pulse of the carotid artery ventral-medial of the sternocleidomastoid. If the pulse in a time interval is lower than the heart rate, there is a pulse deficit.
A resting pulse of 60-80 beats per minute is considered normal, less than 60 beats per minute is called a bradycardia, more than 100 is called a tachycardia, more than 250 is called fluttering, and more than 350 is called fibrillation. If one ventricle (usually both) is in fibrillation, no hemodynamically useful action is possible. If one atrium (usually both) is in flutter or fibrillation, the AV node can filter out useful impulses.
By way of comparison: the heart rate (HR) of the blue whale is 6/min, that of the Etrucan shrew 1000/min. In larger animals, the HR is usually lower than in smaller ones, with the exception of the giraffe (170/min). The giraffe’s blood pressure is also very high at 300/250, because there is a 2-metre difference in height between the heart and the brain; the blood pressures of horses (114/90) and cats (125/75) are very similar to those of humans, while other animals often have significantly different pressures: rooster (191/154), hen (162/133), spiny dogfish (32/16), frog 27, sparrow (180/140). The hearts of mammals are all structured the same and amount to about 0.6% of the body mass; the stroke volume increases linearly with it. A 100-tonne blue whale has a 600-kg heart with a stroke volume of 350 litres, which is about the body volume of four 85-kg adults.
Pulse deficit
A pulse deficit indicates the number by which a peripheral pulse (e.g. the radial pulse) is reduced compared to the heartbeats, i.e. the difference between heart rate and pulse. Physiologically, there is no pulse deficit. A pulse deficit can occur with
- Severe hypotension, e.g. in shock
- Severe hypertension
- Arterial circulatory disorders, e.g. in the context of PAD
- Arterial thromboses
- Arrhythmias in which hemodynamically ineffective heart contractions occur, e.g. extrasystoles, absolute arrhythmia or atrial fibrillation
- Aortic dissection
- Carotid sinus pressure bandage
A pulse deficit can be divided into complete and incomplete,
Complete is when a ventricular contraction does not pump any blood.
Typically, a pulse deficit decreases when the head is lowered to heart level, as when lying down, and increases again when the head is raised. Furthermore, the pulse deficit often decreases as blood pressure rises. Even minor physical activity significantly reduces the pulse deficit, and light exertion such as climbing stairs often causes it to disappear. A pulse deficit can be a sign of heart failure. In 50% of patients with pulse deficits, there are no symptoms; in the other half, palpitations, reduced performance or even presyncopes are noticed.
Because extrasystoles can also trigger a pulse deficit, their causes, some of which are harmless, must also be considered as indirect causes. Supraventricular extrasystoles (SVES, atrial extrasystoles), which occur in the atrium (atrial SVES) or in the AV node (nodal SVES), are usually asymptomatic because they affect hemodynamics less than ventricular extrasystoles (VES). They only occasionally cause heart stumbling or palpitations. In rare cases, dizziness may also occur,
anxiety, nervousness or fainting. They are often found incidentally on the ECG and do not require treatment in otherwise healthy people. Ventricular extrasystoles (VES) can always look the same on the ECG (monomorphic) and are not always pathological, or they often appear differently (polymorphic) and indicate myocardial damage. If a regular heartbeat is followed by only one extrasystole, this is referred to as a bigeminal beat, a trigeminal beat is followed by two extrasystoles and more than two are referred to as volleys. If the extrasystole is too close in time (within the refractory period) to a regular cardiac action, the latter cannot be hemodynamically effective and a compensatory pause occurs. This has no pathological value, but can be perceived as a heart stumble.
Sport is one of the harmless causes of extrasystoles, which also occur in healthy people. They can occur during exercise because the relative lack of oxygen favors potential fluctuations in the heart muscle cells, i.e. affects the electrochemistry of the heart. Due to the adrenergic situation and depending on its extent, dromotropy (excitation conduction) and bathmotropy (excitability) are promoted, the latter above all favoring extrasystoles. This is harmless in otherwise heart-healthy people. Extrasystoles can also occur after sport, because the increasingly active vagus nerve has an increasing influence on the heart when the sympathetic nervous system is simultaneously declining. In addition to sport, stress can also promote extrasystoles in various ways due to the increased excitation of the body, which applies to both dystress and eustress. This is particularly pronounced in the case of cardiac neuroses.
Pregnancy can also promote extrasystoles, especially at the beginning and towards the end. This indicates that thyroid values, electrolytes and cardiac activity should be monitored by ECG. Toxins such as nicotine and caffeine, but also alcohol (consumption and withdrawal) can also lead to extrasystoles. Among the electrolytes, potassium, magnesium (deficiency) and calcium imbalances are particularly conducive to extrasystoles.
Heart rate recovery / heart rate recovery HRR
The recovery heart rate is usually defined as the drop in the heart rate (for the sake of simplicity, a peripheral heart rate) after a certain time following exercise; the post-exercise heart rate is the remaining heart rate, i.e. the training heart rate minus the recovery heart rate. Typical values are 1 (HRR1), 2 (HRR2), 3, 5, 10 minutes. It has been shown that HHR1 correlates with VO2_peak and Pmax, HHR5 is an even better predictor of maximum performance. HHR5 also correlates more strongly than HHR1 or HHR3 with weekly training time. In principle, the recovery heart rate increases with a better level of training in terms of endurance performance. For example, a 1-minute recovery heart rate of only 20 is considered a sign of a low level of fitness, while a heart rate of 30 or more is considered good fitness. However, other parameters are also included in the recovery heart rate, such as the duration, intensity and type of exercise, current health restrictions and the type of recovery.
The initial rapid decline is mainly due to the resumption of vagal tone and the decrease in sympathetic activation. The subsequent slower decline depends on several factors, such as the continued decrease in sympathetic nervous system activation, further decline in catecholamine levels, supply situation and temperature. The faster initial decline in trained individuals is mainly due to the more pronounced increase in vagal tone, which is already higher at rest.
The recovery heart rate indicates the rapid regulatory phase of the ability to regenerate. Over time, the heart rate drops exponentially after exercise. Athletes who complete a high volume of endurance training at not too high an intensity can experience the effect of parasympathetic overtraining, where the recovery heart rate is excessive even though this does not correspond to the oxygen requirement. This is often seen as a protective reaction of the body. Another parameter that can also lead to a high drop in heart rate that does not correspond to the fitness level is fatigue.
According to a Dutch study, the 10-second recovery heart rate correlates better with the risk of death than longer time intervals, which applies not only to the consequences of CHD as a cause of death, but also in general. Measurements were also taken at 20s, 30s, 40s and 50s. In a study involving 126,356 participants, Serge Harb of the Cleveland Clinic used treadmill data on recovery heart rate, exercise capacity, heart rate response (chronotropic reserve) and metabolic rate (metabolic equivalent, MET) to calculate a value called A-BEST (Age Based on Exercise Stress Testing), which is intended to reflect a person’s physiological age. MET and chronotropic reserve correlate reciprocally with the risk of mortality. Particularly poor recovery heart rates were associated with higher mortality risks. A-BEST is particularly well suited as a predictor of mortality or life expectancy.
Pulse Wave Velocity
Pulse Wave Velocity (PWV) The measurement of pulse wave velocity is a non-invasive way of determining the stiffness of the arteries, which helps to assess cardiovascular risk. It is measured at two (ideally widely separated) points on a continuous vascular path, usually an extremity, e.g. upper arm (brachial artery) and in front of the wrist (radial artery). The most important disease that increases the pulse wave velocity is arteriosclerosis (atherosclerosis); increases in the pulse wave velocity are also seen in the following cases:
- Adipositas
- Arterielle Hypertonie
- Chronische Niereninsuffizienz
- Diabetes mellitus
- Hypercholesterinämie
- Hyperurikämie (Gicht)
- Koronare Herzkrankheit (KHK)
- starker Nikotinabusus
The pulse wave velocity must not be confused with the lower flow velocity. In a young, healthy aorta, the pulse wave velocity in its area is approx. 4-6 m/s due to the elasticity (wind kettle function) and the larger lumen, and then approx. 8-12 m/s in the periphery, e.g. in the radial artery. The pulse wave velocity is increased in an aorta with arteriosclerotic changes; the elasticity of the aorta also decreases with increasing biological age and consequently increases the pulse wave velocity, see below:

There are several routes on which PWV is measured:
- Carotid–femoral PWV (cf-PWV, the gold standard, commonly used in studies)
- Carotid–radial PWV (cr-PWV, less clinically significant, but often used in studies on vascular function
- Brachial–ankle PWV (baPWV, very common in Asia (Japan, Korea) because devices such as Omron / Fukuda Denshi were built for this purpose, good correlation with cf-PWV, but systematically higher values)
- Aortic PWV per MRI (MRI-PWV, MRI provides the most direct measurement of aortic propagation velocity, is used more frequently in modern studies, e.g. MESA, Multi-ethnic Study of Atherosclerosis)
The results of the different routes usually differ as follows:
- The further peripheral, the stiffer the vessels → higher PWV.
- Aorta = elastic → lower PWV than legs/arms.
- baPWV → usually 1–2 m/s higher than cf-PWV.
- MRI-PWV measures specific segments, therefore values are often lower at a young age and increase more steeply.
Increased pulse wave velocity leads to an increase in systolic blood pressure and a decrease in diastolic blood pressure as a result of increased pulse wave reflection, i.e. an increase in amplitude, an increased workload of the left ventricle and reduced perfusion of the coronaries in diastole. Physiologically and regularly in healthy young people, the second peak in the pulse contour (course of intra-arterial pressure) caused by the pulse wave reflection is lower than the first peak generated directly by the ventricular action (negative augmentation P2 – P1) and shows a clear gap. In addition to the augmentation, the augmentation index, which relates the augmentation to the pulse pressure, is an important parameter. With significantly lower vascular elasticity, the second peak moves closer to the first and can exceed it (positive augmentation). The augmentation index increases with age and blood pressure and decreases with height and heart rate. As a result, smaller people have a slightly higher average cariovascular risk than taller people. Various studies have shown an increase in mortality of 10 – 39% with a pulse wave velocity increased by 1 m/s. On average, women have a slightly higher index than men due to their smaller body size.
Cardiac output
Cardiac output is the product of heart rate and stroke volume and is therefore the most important parameter for supplying the body with blood. Blood pressure is the (arterial) pressure against which the heart has to perform its work of ejecting blood.
Structure of the heart
The heart is divided by a septum into a left and a right heart, each consisting of an atrium and a ventricle: the atria collect the blood and are equipped with significantly weaker muscles than the ventricles, which expel it into the circulatory system with pressure. The left heart ejects into the systemic circulation and has much stronger muscles due to the significantly higher pressure than in the pulmonary circulation, which is supplied by the right heart. The heart therefore has 2 atria and 2 ventricles:
– atrium dextrum right atrium
– ventriculus dexter right ventricle
between them: Valva tricuspidale (tricuspid valve), tripartite leaflet valve
from the ventricle to the lung: Valva pulmonale (pulmonary valve)
– Atrium sinistrum left atrium
– Ventriculus sinister left ventricle
between: Valva bicuspidale (bicuspid valve or mitral valve), bicuspid leaflet valve
from the ventricle to the aorta: Valva aortae (aortic valve). The four valves are located approximately in one plane, the valve plane, and are held in place by the cardiac skeleton, a connective tissue structure that not only serves as an attachment for the muscles and valves, but also electrically separates the atria and ventricles. During ventricular contraction, the valve plane is pulled downwards towards the apex of the heart, thereby increasing the atrial volume, which draws blood from the vena cava, which is under low pressure, into the atrium. As the valve level, which rises again during the relaxation phase of the ventricles with the leaflet valves now open, overlaps the blood volume in the atria, an atrial contraction is not necessarily required for a haemodynamic action of the heart, i.e. the human being is viable in atrial fibrillation, for example.
Of course, the filling and stroke volume of the two halves of the heart are the same, otherwise the blood would accumulate in the small (pulmonary) or large circulation.
Stimulus formation and conduction
The contraction of the heart is caused electrically by an excitation arising in the heart itself. The conduction system:
1. the crescent-shaped sinus node is located at the junction of the superior vena cava; it is the pacemaker and physiologically the only stimulus pattern and fires with 60-80 pulses / min.
2. the AV or artioventricular node is located in the right atrium in the angle between the septum and the tricuspid valve. It has a natural frequency of 40-60 beats / min. It is the backup system in the event of failure of the sinus node and, if necessary, the moderator of the sinus node impulses.
3. The bundle of His or His bundle is the only muscular connection between the atrium and ventricle
4. The left and right Tawara bundles in the left and right ventricle. They bring the impulse down to the apex of the heart and energise the ventricles
5. The fine Purkinj fibres go to the fibres of the working myocardium
The sinus node has no connection to the 2nd-5th; the AV receives the impulse from the sinus node as an electrical signal from the muscles of the atrium. The impulse runs: sinus node -> atrial musculature -> AV -> bundle of His -> Tawara leg -> Purkinj fibres -> cardiac apex -> back up to the bundle of His. It stops in front of the AV.
Cardiac action: the phases
Oxygen-rich venous blood and oxygen-poor arterial blood only exist in the small circulation between the heart and lungs; in the large circulation, the venous blood is oxygen-poor and the arterial blood is oxygen-rich. The deoxygenated blood from the lower extremities and the abdominal and thoracic cavity reaches the vena cava inferior inferior vena cava and the deoxygenated blood from the upper extremities via the vena cava superior vena cava into the atrium dextrum. In diastole (filling phase: the leaflet valves are open and the pocket valves are closed), the blood continues to flow into the vetriculus dexter. During systole (contraction phase of the heart muscle with open valves and closed leaflets), the blood is pumped into the pulmonary trunk and flows to the lungs. As it passes through the lungs, it is enriched with oxygen by diffusion on the semi-permeable membranes of the alveoli and flows back through the venae pulmonalis sinistrae and venae pulmonalis dextrae into the atrium sinistrum. The mitral valve then opens and the blood flows into the sinister ventricle during diastole, from where it is pumped into the aortic arch during systole. Systole is further divided into the tension phase (phase in which the heart muscle has already tensed, but the pressure generated is not yet sufficient to open the valves and expel blood) and the expulsion phase. Diastole is also divided into a relaxation phase (the heart muscle stops contracting and expands again) and a filling phase (blood flows into the atria).
Wall layers of the heart
The heart consists of (from the inside out):
Endocardium
The inner wall of the heart, also known as the inner lining of the heart, lines the inside of the heart and also forms the valves, is completely smooth.
Task:
1. smoothing out unevenness and roughness and keeping the surface as smooth as a mirror so that the flow resistance is as low as possible
2. valve function of the valves
Myocardium
The heart muscle, also known as the working myocardium. The myocardium of the left heart is 2-3 times as thick as that of the right heart and also has 2-3 times the strength: while the pressure in the atria is approx. 0-5 mmHg, the pressure in the right ventricle is 40-45 mmHg and in the left ventricle 120 mmHg. All four atria and ventricles are approximately the same size; of the approx. 150 ml they can hold, approx. 70-80 ml (50-100) are moved during each cardiac action. At a pulse rate of 80, this is approx. 5 l / min or once the entire blood volume per minute.
Doubling the stroke volume and increasing the frequency by a factor of 2.5 results in a maximum of 5 under physical stress.
The cardiac output can be increased under the influence of sympathetic nerve fibres, which release noradrenaline in the myocardium and excitation conduction, and this can also reach the heart via the bloodstream together with adrenaline. These have both a chronotropic and inotropic effect and also a dromotropic effect (conduction time of the AV node is shortened). The opponent of the sympathetic nervous system, the parasympathetic vagus nerve has a negative chronotropic, inotropic, dromotropic and bathmotropic (increases the excitation threshold) effect via acetylcholine. With the Frank-Starling mechanism, the heart adapts the ejection force to the filling: a larger volume means more dilation, which causes the heart muscle to pump more. If there is permanently too much blood volume, a diuretic hormone, the atrial natriuretic peptide (ANP)
tasks of the myocardium:
1. contraction to move the blood forwards in the sense of circulation.
2. conduction: transmitting the electrical impulses that lead to the contractions of the 4 spaces from the point of origin, the sinus node.
Epikard
Outer wall of the heart, sits on the outside of the myocardium and is firmly attached to it
Function: serves to shape and maintain the myocardium and aims to minimise friction with its mirror-smooth surface
There is serous pericardial fluid between the epicardium and pericardium, which reduces the friction between the two.
Pericardium
Pericardium , strictly speaking, the epicardium turns into the pericardium at the outlet of the great vessels, as if the heart were a fist placed in an air-filled balloon so that its wall doubles over the fist.
Coronaries
The coronaries or coronary arteries supply the heart muscle with blood:
the a.coronaria dexter supplies the right ventricle and the right atrium as well as the posterior wall of the heart and the a.coronaria sinister supplies the left ventricle and the left atrium as well as a large part of the ventricular septum. The a. coronaria dexter runs almost horizontally backwards, the a.coronaria sinister is very short and also runs almost horizontally before splitting into 2 branches: the ramus circumflexus goes to the posterior side and the RIVA ramus interventricularis anterior runs downwards and divides the heart into its two halves (right. and left). In diastole, the heart itself is supplied with blood (the systolic contraction constricts the heart vessels, which is why this is not possible). The apex of the heart lies at the 5th ICR medioclavicular. When palpating, remember that the clavicle lies above the 1st ICR, so that the first palpable one is the 2nd.
ECG
P: Excitation of the atrium by sinus node, approx. 100 ms
Q: Beginning of ventricular excitation, conduction from the apex to the base of the heart, 40 ms, < ¼ of the R wave, widened or deeper: sign of past myocardial infarction. As the papillary muscles conduct faster, they contract slightly before the ventricle
P-Q: conduction time from the sinus node to the AV node
R: depolarisation of the myocardium. Widened or notched: Disturbance of conduction, reduced: Indication of previous infarction
QRS: approx. 110 ms, sometimes up to 120 ms
Lungs
Mediastinum
The mediastinum is located in the mediastinum: Heart, aorta, trachea, oesophagus, thymus gland, truncus pulmonalis, n. vagus, ductus thoracicus). The thoracic duct runs behind the left clavicle to the left venous angle towards the heart and transports, among other things, long-chain fatty acids, which are released into the blood with a time delay.
Trachea
Trachea Trachea, shorter than the oesophagus in front of which it lies, length approx. 11-14 cm. Begins at the level of the cricoid cartilage behind the thyroid gland, consists of 16-20 horseshoe-shaped cartilage clasps, towards the back: connective tissue skin, lies in front of the oesophagus, therefore only tissue at the back. Divides, division site: bifurcation tracheae, into right and left main bronchus (still has cartilage clasps), right side is steeper, therefore more likely to obstruct when swallowing. The right main bronchus has 3 main branches, the left 2 main branches corresponding to the number of lobes of the lung. The bronchi branch out further and further, and the number of alveoli increases rapidly at the bottom. The alveoli are surrounded by veins and arteries
Lung
Pulmo or Pneumo lung consisting of a left and right lobe with 3 (right) and 2 (left) lobes (lobus). According to the outlets from the bronchi, 10 segments can be distinguished on the right and 9 on the left. The left lung is somewhat smaller because the heart takes up some space.
The lung consists of the branching tree of the bronchi, each of which ultimately ends with countless alveoli (pulmonary alveoli). Through the interplay of inhalation and exhalation, fresh, oxygen-rich air is constantly transported to the blood-air barrier, the approx. 2.2 µm thin diffusible tissue layer between the airy interior of the lungs and the capillaries. The inhalation enlarges the chest cavity in two ways:
abdominal breathing
– the dome-shaped muscular diaphragm moves downwards and enlarges the space for the lungs, which are fused to it: 1.5 cm when inhaling calmly, 10 cm when inhaling deeply. Excessive diaphragmatic contraction can pull the ribs downwards and thus restrict chest breathing
chest breathing
– the ribcage, which rises forwards and upwards during chest breathing, enlarges the space of the lungs, which adhere to the chest from the inside: the visceral pulmonary pleura (pleura pulmonalis), which lies directly on the lungs, is attached in a sliding manner by means of a serous fluid to the parietal (pleura parietalis) pulmonary pleura, which lines the chest from the inside. The greatest expansion of the chest occurs in the sagittal direction, especially in the cranial region, and further caudally also to some extent in the frontal plane.
If air enters the (only) fluid-filled pleural space between the parietal and visceral leaflets, one becomes detached from the other and the lung no longer follows the excursion of the thorax. If, in the context of pleuritis, one pleura grows together or sticks together with the other, mobility is restricted and inhalation is painfully limited.
With slight breathing, almost only the Mm. Scaleni lift the chest from above, with moderate inspiration, the intercostal muscles are added and with vigorous inspiration all other inspiratory muscles plus the inspiratory auxiliary muscles. Due to the gravity of the costal arches, exhalation also occurs without the use of muscles. Even against gravity, the retraction force (inherent tension of the lung tissue) is sufficient. In addition, the tension of the abdominal muscles lifts the abdominal inhalation, and the gravity of the ribcage (in an upright position) causes the chest exhalation.
When inhaling, the air in the airways above the lungs is also moved; this space consisting of the nasal or oral cavity, pharynx, trachea and bronchi is referred to as the dead space and comprises approx. 150 ml. This is where the air we breathe is warmed, moistened and cleaned of dust (especially in the nose). The mouth is very unsuitable for cleaning dust. The ciliated epithelium of the trachea (windpipe) and bronchi can transport particles back out of the respiratory tract.
Breathing volumes
Various breathing volumes are defined:
Breathing volume: the volume of air normally moved, between approx. 500 ml at rest and 2,5 litres during strenuous exercise
end-expiratory lung volume (lung volume after normal exhalation) =
functional residual capacity
This is subdivided into
– expiratory reserve volume: Volume that can still be exhaled with effort, on average 1 – 2 litres
– Residual volume: Volume that can no longer be exhaled even with the greatest effort, 1 – 1.5 litres, largely escapes when the pleural cavity is opened on both sides
– Inspiratory reserve volume: Volume that can still be inhaled in addition to normal inhalation, on average 2 – 4 litres
– vital capacity: Sum of tidal volume, inspiratory and expiratory reserve volume
– Total capacity: Vital capacity plus residual volume, approx. 5 – 10 litres, slightly smaller in women than in men, strongly dependent on training level
Resting breathing position
The resting breathing position is the point of equilibrium between the retraction force of the lungs and the elastically expanding forces of the ribcage. During the transition from sitting/standing/walking to the supine position, the greater gravitational effect of the ribcage and the pressure of the lung organs against the diaphragm shift the resting breathing position slightly towards the expiratory region. A decrease in the elastic retraction force of the lungs leads to a shift in the resting position of the lungs towards the inspiratory side, in which case the expiratory reserve volume increases and the inspiratory volume decreases (as in emphysema, for example). If the thorax is very flexible, the inspiratory volume increases and the expiratory volume decreases. A low respiratory resting position, i.e. a low expiratory volume with a high inspiratory reserve volume, is desirable because less oxygen-poor air remains in the lungs and inhaling the same volume of air leads to a higher oxygen content of the air in the lungs after inspiration. The quotient of (tidal volume minus dead space volume) by (residual volume plus expiratory reserve volume) is called the ventilation coefficient and is on average 1/8. It should be as large as possible and becomes correspondingly smaller in diseases such as emphysema.
The respiratory rate is on average 15/min (12-20), so approx. 500 ml of air is exchanged in 4 s, with the expiratory volume being longer at a ratio of 3:2, and there is often an end-expiratory breathing pause. On average, 7-8 litres of air are taken in per minute, including ¼ litre of oxygen. Depending on the level of training, a maximum of approx. 120 litres of air are taken in per minute.
The oxygen transferred to the cells during internal respiration is used to „burn“ nutrients: carbohydrates, fats and proteins. Ideally, these are burnt residue-free to CO2 and H2O; in the case of proteins, urea is also produced, which must be excreted by the kidneys. Like the pulse, respiration is also regulated by the medulla oblongata. If regulation were to fail, the oxygen content in the blood would fall (hypoxia) and the CO2 content would rise (hypercapnia) in the event of physical exertion or other increased energy requirements, which would have a detrimental effect on the blood pH. For this reason, the partial pressures for O2 and CO2 are measured in the aortic arch and in the glomus caroticus, as well as the pH and pCO2 from the medulla oblongata itself. Stretch receptors in the alveoli inhibit further respiration (Hering-Breuer reflex). Other impulses from different parts of the body influence breathing. The respiratory rate and tidal volume can be increased in the same way as the heart, but it is more favourable to increase the tidal volume, as this reduces the dead space.
At the beginning, the bronchial tree still contains a significant amount of cartilage to prevent it from collapsing. A surfactant (surface active agent) is produced in the alveoli and released to the surface, which reduces the surface tension. Macrophages phagocytise dust and remnants of haemorrhages. After the structure of the tissue, fluid can leak into the lungs (the air-filled space) in the event of congestion in the lungs due to cardiac insufficiency, resulting in pulmonary oedema.
Before birth, the lungs are not vital, but after birth they have to expand at lightning speed: the water in the lungs is displaced by the air with the help of surfactant and breathing is possible. The newborn’s first cry is proof that the lungs are filled with air.
Functional tests of the lungs
FEV1 (expiratory vital capacity FEV1, Tiffenau test (https://yogabook.org/tests/#tiffeneau): after a maximum inhalation, the maximum amount of air that the subject can exhale in one second is measured (relative second capacity). Depending on their age, healthy individuals achieve 70-80% of their vital capacity. Obstructive lung diseases, reduced lung compliance and weakened expiratory (and auxiliary) muscles reduce this value. The average forced expiratory volume in the first second (FEV1) decreases slowly from puberty onwards and is higher in taller people than in shorter ones. In men, FEV1 is greater than in women of the same height.
In addition, the lung volume of people who live at higher altitudes is generally greater.
FEV1%: the ratio of FEV1 / FVC (Tiffenau index)
PEF (peak expiratory flow): the maximum respiratory flow rate during exhalation in l/s
PIF (peak inspiratory flow): the maximum respiratory flow rate during inhalation in l/s
FEF25 (forced expiratory flow at 25% expiration): respiratory flow strength at 25% expiration
FEF50 (forced expiratory flow at 50% expiration): respiratory flow strength at 50% expiration
FEF75 (forced expiratory flow at 75% expiration): respiratory flow strength at 75% expiration
FEF2575 (mean forced expiratory flow between 25% and 75% exhalation): average respiratory flow strength between 25% and 75% exhalation
Spirometry: determination of tidal volume, vital capacity, inspiratory reserve volume and expiratory reserve volume:
VC (vital capacity), also FCV (forced vital capacity): volume difference between maximum inhalation and maximum exhalation. This parameter can also be differentiated into:
IVC (inspiratory vital capacity): determination of the VC from the exhaled state
EVC (expiratory vital capacity): determination of the VC from an inhaled state
These two can differ slightly.
The VC should be at least 3 liters and is mainly restricted by restrictive lung diseases. In good cases, it is 5 liters, which of course depends on height and build.
The European Coal and Steel Community uses the formula: height in meters to the power of 3 / correction factor * (1.03 – (age – 25)) * 0.75, with a correction factor of 1 for men and 1.1 for women.
A 20% decrease is considered pathological. Other sources give different formulas:
0.052 * height – 0.022 * age – 3.6 for men and
0.041 * height – 0.018 * age – 2.69 for women or even
(27.63 – 0.112 * age) * height for men and
(21.78 – 0.101 * age) * height for women.
There are some contraindications for determining FVC by test:
hemoptysis, pneumothorax, cardiac events such as heart attack, angina pectoris, thoracic, cerebral and abdominal aneurysms, cataracts, recent surgery, dizziness, nausea, acute illness, current or recent viral illness, undiagnosed hypertension.
Respiration is usually only understood as external (lung) respiration, but respiration also includes internal (cellular) respiration. Respiration consists of:
– Ventilation
– Gas exchange in the lungs
– Gas transport in the blood
– Gas exchange in tissue
– Utilisation of oxygen in the cell
– Adaptation of respiration according to need
Respiratory muscles
Inspiratory respiratory muscles
Diaphragm (diaphragm)
Musculi scaleni
Musculi intercostales externi (external intercostal muscles)
Musculi intercartilaginei, i.e. the part of the internal intercostal muscles that runs between the rib cartilages
Inspiratory auxiliary respiratory muscles
Musculi levatores costarum
Musculus serratus anterior (anterior saw muscle)
serratus muscle posterior superior (posterior superior saw muscle)
serratus muscle posterior inferior (posterior inferior saw muscle)
musculus pectoralis minor et major (with arm supported)
musculus sternocleidomastoideus
musculus erector spinae
Exspiratorische Atemmuskeln
Musculi intercostales interni et intimi (innere Zwischenrippenmuskeln)
Musculi subcostales (Unterrippenmuskeln)
Exspiratorische Atemhilfsmuskeln
Musculus obliquus externus abdominis
Musculus obliquus internus abdominis
Musculus transversus abdominis
Musculus transversus thoracis
Musculus latissimus dorsi („Hustenmuskel“)
Musculus quadratus lumborum
Musculus rectus abdominis
The abdominal muscles primarily support rapid exhalation from approx. 40 l / min.
A distinction is made between costosternal (chest breathing) and costodiaphragmatic (abdominal breathing) breathing.The first expands the thorax forwards, while the second expands the lungs downwards and compresses the abdominal cavity, primarily through the diaphragm, causing the abdominal wall to bulge forwards. In the upright position of the upper body (sitting, standing, walking), costodiaphragmatic breathing predominates, as the diaphragm can contract easily and freely downwards. In the supine position, there is increased counterpressure of the abdominal organs against the diaphragm and thoracic respiration gains weight. In the prone position, thoracic inspiration is impeded by the gravity-induced pressure on the chest and abdominal breathing is impeded by the gravity-induced pressure on the abdominal cavity, so that both types of breathing are restricted.
The portal vein vena portae collects the blood from all unpaired abdominal organs (not the kidneys) and channels its substances to the liver. The individual organs: stomach, small intestine, large intestine, parts of the rectum, pancreas, spleen. It is 8-15 mm wide, has a flow velocity of up to 23 cm/s and a pressure between 5 and 20 mmHg, which is difficult to measure. If the blood accumulates in the portal vein or the liver, other venous systems have to drain the blood and are overloaded, forming porto-caval anastomoses:
– oesophageal varices (varicose veins in the oesophagus)
– caput medusae (overload of deep and superficial abdominal and thoracic veins)
– haemorrhoids as a result of varices in the area of the rectum
In addition to the abdominal portal vein, there are also the pituitary portal veins (hypophysial portal veins), which transport various control hormones from the
hypothalamus (supreme regulatory centre for all vegetative and endocrine processes) to the anterior pituitary (forms various effector and control hormones):
releasing hormones (liberins) CRH, thyreoliberin, gonadoliberin, somatoliberin and the inhibiting hormones (statins) dopamine and somatostatin
The HVL produces glandotropic hormones (act on endocrine glands) depending on these:
TSH = thyroid-stimulating hormone
ACTH = adrenocorticotropic hormone
FSH = follicle-stimulating hormone
LH = luteinising hormone
and non-glandotropic hormones:
STH = Somatotropic hormone
MSH = Melanocyte-stimulating hormone
Prolactin
