yogabook / movement physiology
This separate glossary explains many terms and facts about the way our musculoskeletal system works in principle and in the field of gravity. The scope of the topic is difficult to narrow down and is multidisciplinary. The lever law and mass inertia are just as much a part of this chapter as the sine function and the algorithm, an elementary discussion of the behavior of muscles in monoarticular, biarticular and polyarticular cases, the resulting partial tendency to active insufficiency or passive insufficiency, the force-length relationship (which is indeed a polygonal function) or basic principles of movement physiology such as tension belts and rein systems. Elementary principles of training theory must be explained as well as the types of muscle contraction and the types and phases of muscle failure. The multitude of terms and related disciplines may be an indication that an interdisciplinary approach is indispensable for a conscientious consideration of the asanas. We call this multidisciplinary field: movement physiology.
O _ P _
There are separate subpages for some topics:
abduction (generally)
blood circulation
bones
extension deficiency
fasziae
joints
joint shapes
heart rate variability
leg length discrepancy
load maximum
Mikulicz-line
muscles
nervous system
pelvis
posture
regeneration
ROM (Range Of Motion)
resting heart rate (RHR)
tendon
Muscles:
autochthonous back muscles • dorsal hip muscles • hamstrings • muscles (generally) • muscles injuries • rein system
Sports/Motion:
endurance sports • fitness • walking (sportive) • jogging • walking (generally) • strength training: Jo Weider training principles • racket sports • cycling
• rowing • running • swimming • sports during growth • sprinting
A
abdominal respiration
see movement physiology-circulation/abdominal respiration.
Abduction
See movement physiology/abduction.
Abduction (leg / hip joint)
the lateral abduction of a leg (without rotation and movement forwards/backwards), i.e. a movement in the frontal plane. The degree of possible abduction is a function of the degree of external rotation: In zero degree rotation, as in standard anatomical position, abduction is limited to a good 20°. With each degree of exorotation of the leg in the hip joint, the abduction capability increases and reaches its maximum at 90° or even higher, whereby it is then mainly limited by the monoarticular and biarticular extensors of the hip joint. Unfortunately, this fact is not consistently taken into account in the anatomical literature. It is highly relevant for poses such as trikonasana and warrior 2 pose.
Abduction, dorsal (arm / shoulder joint)
increasing the dorsal angle of the arm to the trunk, i.e. in standard anatomical position, lifting the arm backwards and upwards, generally referred to as retroversion in the shoulder joint. Reversing this movement to standard anatomical position is called dorsal adduction.
Abduction, frontal (arm / shoulder joint)
The increase in the angle of the arm in front of the body in relation to the trunk as a movement of the humerus in the glenohumeral joint, i.e. in standard anatomical position the lifting of the arm in the sagittal plane forwards and upwards. Synonym: anteversion in the shoulder joint.
Abduction, lateral (arm / shoulder joint)
Movement in the glenohumeral joint in which the lateral angle (in the fontal plane) of the arm to the trunk is increased. In the internally rotated state, the arm can hardly be abducted laterally by more than 90° before a firm-elastic or hard-elastic movement limit restricts the abduction, but if it is turned out, the abduction even with slightly above-average flexibility is only restricted by a soft-elastic movement limit, and more than 180° is possible with good flexibility.
The lateral abduction of the shoulder joint has a special feature in that on the first degree of abduction (with the arm dropped as in anatomical zero) the main laterally abducting agonist deltoid due to its course mediocaudal to the glenohumeral joint cannot yet generate an abducting torque with any fibre of a caput. This applies to the pars acromialis and even more so to the pars spinalis and pars clavicularis. These still lie up to almost 10 cm mediocaudal to the centre of rotation in the humeral head. The supraspinatus must act as the agonist for the first 10-15 degrees of lateral abduction, before the course of the pars acromialis of the deltoid becomes favourable enough to produce a lateral abduction moment. The supraspinatus then slowly approaches its active insufficiency. From around 60°, the acromial pars of the deltoid becomes actively insufficient and the pinnate parts (pars clavicularis and pars spinalis) take over the rest of the lateral abduction.
Abductors (leg / hip joint)
Term for the group of muscles whose function (not necessarily exclusively) is to abduct the leg, i.e. to spread it to the side. The abductors of the leg include the gluteus medius, gluteus minimus, gluteus maximus, tensor fasciae latae, piriformis and obturator internus muscles.
Achilles tendon
the robust tendon into which the triceps surae (soleus and gastrocnemius) opens in order to bring the dorsal calcaneus closer to the popliteal region during its concentric contraction, which is referred to as plantar flexion or extension of the ankle. The Achilles tendon receives most of its arterial supply proximally and distally. It is most vulnerable in the area between the proximal and dorsal supply. In the case of a dorsal heel spur, the attachment area of the Achilles tendon to the calcaneus calcifies and ossifies. In contrast, Haglund’s heel is a ganglion on the dorsal cranial calcaneus, which presses on the Achilles tendon in a space-occupying manner. Both can irritate the Achilles tendon and trigger bursitis (inflammation of the bursa). Triggers can be mechanical irritation (heel cap of a new shoe), sporting overload (overuse) or a shortening of the gastrocnemius.
active insufficiency
see movement physiology – muscle/active insufficiency.
Active mobility
The range of movement in a joint that can be achieved by the person’s own muscle activity. Physiologically, this is not significantly smaller than that of passive mobility, but the two can differ considerably if there are changes in the joints or muscles. See also: passive mobility.
Active insufficiency
See movement physiology – muscle/active insufficiency.
Adduction
Adduction means moving towards. In the yoga book, the term is not used for the shoulder joint without a further designation (lateral adduction, frontal adduction), but it is used for the hip joint for the medial movement of the leg (also beyond standard anatomical position), as well as for the small and large fingers and toes (hallux, pollex). The conceptual opposite, abduction, is used for the movement away from the midline of the body, midline of the hand or midline of the foot.
Adduction (leg / hip joint)
the movement of the leg from a laterally abducted position to the medial, back to standard anatomical position or its movement beyond standard anatomical position further to the contralateral, i.e. this is a movement in the frontal plane.
Adduction, dorsal (arm / shoulder joint)
the reduction of the angle of the back of the arm to the trunk as a movement of the humerus in the glenohumeral joint, i.e. a movement in the sagittal plane: the movement of the arm from a raised backwards and upwards position back to standard anatomical position. The common term is retroversion.
Adduction, frontal (arm / shoulder joint)
the reduction of the angle of the arm in front of the body in relation to the trunk as a movement of the humerus in the glenohumeral joint, i.e. the movement of the arm from the forward-upward raised state in direction of standard anatomical position.
Adduction, lateral (arm / shoulder joint)
Movement of the arm in the glenohumeral joint, in which the lateral angle (in the fontal plane) of the arm to the trunk is reduced towards standard anatomical position.
Adductors (leg / hip joint)
Term for the group of muscles whose function is (not necessarily exclusively) the adduction of the leg, i.e. bringing the leg in from the side. They mainly originate in the area of the lower and lower lateral pubic bone. All monoarticular adductor muscles attach to different areas of the inner thigh bone, only the monoarticular adductor magnus muscle has an additional origin on the ischium and the biarticular gracilis muscle attaches below the knee joint on the inner upper tibia (on the pes anserinus superficialis). In addition to the gracilis, the adductor muscles of the leg include the adductor brevis, adductor minimus, adductor magnus, adductor longus and pectineus muscles and – in the pelvitrochanteric group of muscles, also caled the dorsal hip musculature – the obturator externus and the quadratus femoris muscles, which originate at locations other than those described above and attach at the trochanter major of the femur. The adductor magnus muscle is the only one that also attaches to the ischium and therefore has a internally rotating and extending effect on the thigh. The adductor compartment of the thigh is divided into:
- superficial: M. pectineus, M. gracilis and M. adductor longus
- middle: M. adductor brevis
- deep: M. adductor magnus and M. adductor minimus
A fact that is not mentioned in many sources, but which is very relevant in practice for asana, is the flexing effect of the adductor muscles from low degrees of flexion as well as the flexion-reducing effect with further flexion. The flexion is supported up to around 80 degrees, after which the flexion-reducing effect increasingly sets in, which overlaps with the flexion-reducing effects of the short hip extensors and, above all, the knee joint with more or less extended ischiocrural group. With less pronounced mobility, a pronounced stretch can be felt in the adductor group in postures such as the 1st hip opening in the front leg.
Aerobic
An aerobic metabolism is one in which the supply of energy from carbohydrates (glucose circulating in the blood and stored in muscles) and fats is covered exclusively by oxygen consumption. The opposite of aerobic is where the oxygen supply is not sufficient to cover the energy requirement. Aerobic performance can be sustained over longer periods of time than anaerobic.
Aerobic threshold
The aerobic threshold is the level of performance demand from which the lactate level in the blood rises from rest (approx. 1.2 mmol/l) to approx. 2 mmol/l. When the aerobic threshold is reached, the energy supply ist no longer purely base on oxygen consumption and therefore more lactate is produced than at rest, but this can be broken down in real time as long as the anaerobic threshold has not yet been reached. The aerobic threshold is highly dependent on the level of training and can be around 60% of the maximum heart rate for people with little endurance training or around 85% for trained people. Training above the aerobic threshold but below the anaerobic threshold improves the vascularization of the muscles as well as the fat metabolism.
afferent (nervous system)
see movement physiology – nervous system/afferent.
Agonist
literally the „actor“, the muscle that performs a movement. Opposing muscles, i.e. muscles that perform the opposite movement, are called antagonists.
Algorithm
An algorithm is a rule for solving a task or a class of tasks. It can refer to a mathematical problem, a technical operation such as installing an operating system or program on a computer, making an object with a machine, or an everyday operation such as tying shoelaces or an apron or a Windsor knot on a tie. The algorithm can be more or less general, but in any case it must consist of a finite number of well-defined steps and should deliver the desired correct result in the usual application cases (termination). Typical algorithms used in practice are both determined (always deliver the same result with the same starting values) and deterministic (always deliver the result in the same, predictable way). There is more than one correct algorithm for many problems. Even if all correct algorithms lead to the same goal, they can do so with different resources (e.g. time or main memory). Getting by with few resources is called efficiency.
Ideally, taking a yoga pose is also described by an algorithm. This does not have to be linear but can contain conditions and branches, such as „IF the contralateral hand does not reach the floor, THEN use a block“ in the example of parivrtta trikonasana. In programming languages, conditional commands of the type IF CONDITION THEN STATEMENT1 (ELSE STATEMENT2) can be found in abundance, whereby an optional substitute statement STATEMENT2 can be specified, which is executed if the condition CONDITION is not fulfilled. In the case of parivrtta trikonasana, for example, the condition could also query whether there are any blocks left and specify support on the lower leg as a substitute instruction. The instruction „use a block“ can in turn represent a control loop of the type „repeat the increase in support by adding a block to the existing blocks until the fingers reach the block“. Such instructions are realized by control structures of the type REPEAT STATEMENT UNTIL CONDITION or WHILE CONDITION DO STATEMENT. Experienced teachers usually have these algorithms in their heads, even if they would not necessarily regard them as such or be able to write them down in every detail. In special cases that involve conditions that are not covered by his algorithm, he needs creativity and has to invent something new. This then enhances his algorithm. Algorithms can be represented in a flow chart, which graphically depicts the conditions, instructions and structures. In the case of asanas, the starting pose would be at the beginning, for example tadasana, and the target pose at the end.
All Cause Mortality
All-cause mortality refers to the mortality rate of a group of people over a specific period of time. This figure is used to describe the health of the group of people or interventions on the group of people. No distinction is made between causes of death, meaning that traumatic causes are not excluded and multifactorial deaths are also taken into account. The inverse of all-cause mortality is the survival rate, also based on a specific period of time. Many different variables and diseases correlate with the all-cause mortality of the population, such as:
- PWV: an increase in ePWV (estimated PWV) of 1 m/s increases the risk by 37%, and for cardiovascular mortality by as much as 41%. Between 6.5 m/s and 8.7 m/s, an increase in overall mortality by a factor of 3.2 has been demonstrated. Cardiovascular mortality increases by a factor of 16.1 between 7.2 m/s and 8.5 m/s.
- Alter
- Systolic hypertension: is a strong predictor
- Obesity: with a BMI of 40 or above, PWV is an independent predictor
- hyperlipidaemia
- Antihypertensive medication indicates underlying hypertension and thus an increased risk.
- Many diseases correlate with elevated ACM, such as
- Cardiovascular: heart attack, heart failure, stroke, chronic arterial hypertension, arteriosclerosis
- Metabolism: Type 2 diabetes mellitus (severe), metabolic syndrome, BMI: Mortality increases from age 35, increases significantly from age 35
- Pulmonary: COPD, lung diseases caused by smoking (such as emphysema, chronic bronchitis), severe forms of asthma, pulmonary fibrosis, lung cancer
- Malignant: pancreatic carcinoma, colorectal carcinoma (bowel cancer), late stages of breast and prostate carcinoma, HIV/AIDS (research needed!), cirrhosis of the liver, hepatitis B/C (with cirrhosis of the liver or hepatocellular carcinoma HCC)
- renal: chronic kidney disease (CKD), end-stage renal failure (dialysis)
- Dementia (especially Alzheimer’s disease, vascular dementia)
- Infectious: sepsis, pneumonia (especially in older people)
- Smoking: one of the strongest risk factors of all
- lack of exercise
- Unhealthy diet, especially high sugar consumption, lots of processed meat, too little fruit/vegetables, trans and saturated fats
- Alcohol: chronic high consumption
- Sleep behaviour: less than 6 or more than 9 hours per day
- Psychosocial: Chronic stress, depression (very severe), anxiety disorders, social isolation, low socio-economic status
- Environment and exposure: Air pollution (PM2.5: high evidence), air pollution (PM2.5: high evidence), chemicals such as pesticides or heavy metals
- In addition, there are correlations with many laboratory parameters that are chronically altered, such as CRP, IL-6, TNF-α, HbA1c, LDL cholesterol, triglycerides, fasting insulin, GFR (kidneys), albuminuria, hypoalbuminaemia, anaemia, leukocytosis, men: hypotestosteronaemia/hypogonadism, untreated hypothyroidism, to a lesser extent: hyperthyroidism
Allochthonous back muscles
all back muscles that are not autochthonous. The allochthonous muscles are migrated limb muscles and are not primarily ones that move the spine but the limbs.
allodynia
see movement physiology – nervous system/allodynia.
anabolic / anabolism
Anabolism usually refers to the entirety of anabolic metabolic reactions, whereby energy supply is not included, but only the formation of more complex substances in the body from simpler ones. Anabolism and catabolism together form metabolism. Either anabolic or catabolic reactions take place in a cell, but not both at the same time. Physiological growth processes occur through anabolic processes.
Anaerobic
Anaerobic metabolism is a metabolism in which the energy supply is not exclusively covered by oxygen consumption but also partly without oxygen consumption, so that lactate is produced in larger quantities. In principle, a small amount of lactate is also produced at rest (up to approx. 1.2 mmol/l), but this can be disposed of without any problems, even far beyond the aerobic threshold of approx. 2 mmol/l lactate can be disposed of in realtime. The point at which this is no longer possible, but lactate accumulates in the blood, muscles and interstitium, is called the anaerobic threshold. It is around 4 mmol/l. Performance above the anaerobic threshold cannot be sustained over a longer period of time. In contrast to glucose, fats cannot be metabolized without an oxygen supply.
Anaerobic threshold
The degree of exertion or performance demand above which the body can no longer supply the muscles with sufficient oxygen, so that more lactate is formed during metabolism than can be broken down. Exceeding the anaerobic threshold leads to an increase in the concentration of lactate in the muscle, blood and interstitium. The lactate concentration is typically determined invasively by means of a blood test (capillary earlobe blood). The anaerobic threshold is approx. 4 mmol/l for most people, but can vary between 2.3 and 6.8 mmol/l depending on the individual. Lactate is also formed without physical exertion up to a concentration of approx. 1.2 mmol/l, increasing with the intensity of physical exertion. In addition to the anaerobic threshold, there is also the (now not uncontroversial) aerobic threshold, which is defined by the fact that the lactate concentration in the blood rises for the first time (with regard to increasing exercise intensity) compared to the resting concentration. For most people, this is around 2 mmol/l.
Endurance performance cannot be sustained above the anaerobic threshold for long periods of time. The anaerobic threshold can be exceeded for a short time (attack in a cycling race, sprint in soccer, etc.) without a drop in performance. It is closely related to a certain heart rate, speed (running, cycling) and power output. There is also a correlation with oxygen uptake: in untrained people, the lactate curve rises approximately parabolically from around 50% of maximum oxygen uptake; in top endurance athletes, this threshold is around 90%. The anaerobic threshold can be recognized simply and non-invasively in ergometry at approximately the point at which the heart rate, which previously rose linearly with the performance requirement, begins to rise non-linearly.
Irrespective of the anaerobic threshold at which continuous endurance performance can still be achieved, the glycogen reserves are exhausted after around 60 – 90 minutes (depending on the level of training), so that performance collapses even without the anaerobic threshold being exceeded. Appropriate food intake during performance cannot usually fully compensate for this effect.
anatomical leg length discrepancy
see movement physiology – leg length discrepancy/anatomical leg length disrepancy.
Ancylosis
Complete stiffening of a joint. This is usually caused by ossification of the joint space or increasing stiffening of the joint capsule, usually due to scarring.
Antagonist
most often: muscular opponent that performs a movement that is at least partially opposite to the muscle under consideration (agonist). The term is also used in other fields such as neurology or endocrinology for nerves or substances that have a reinforcing effect.
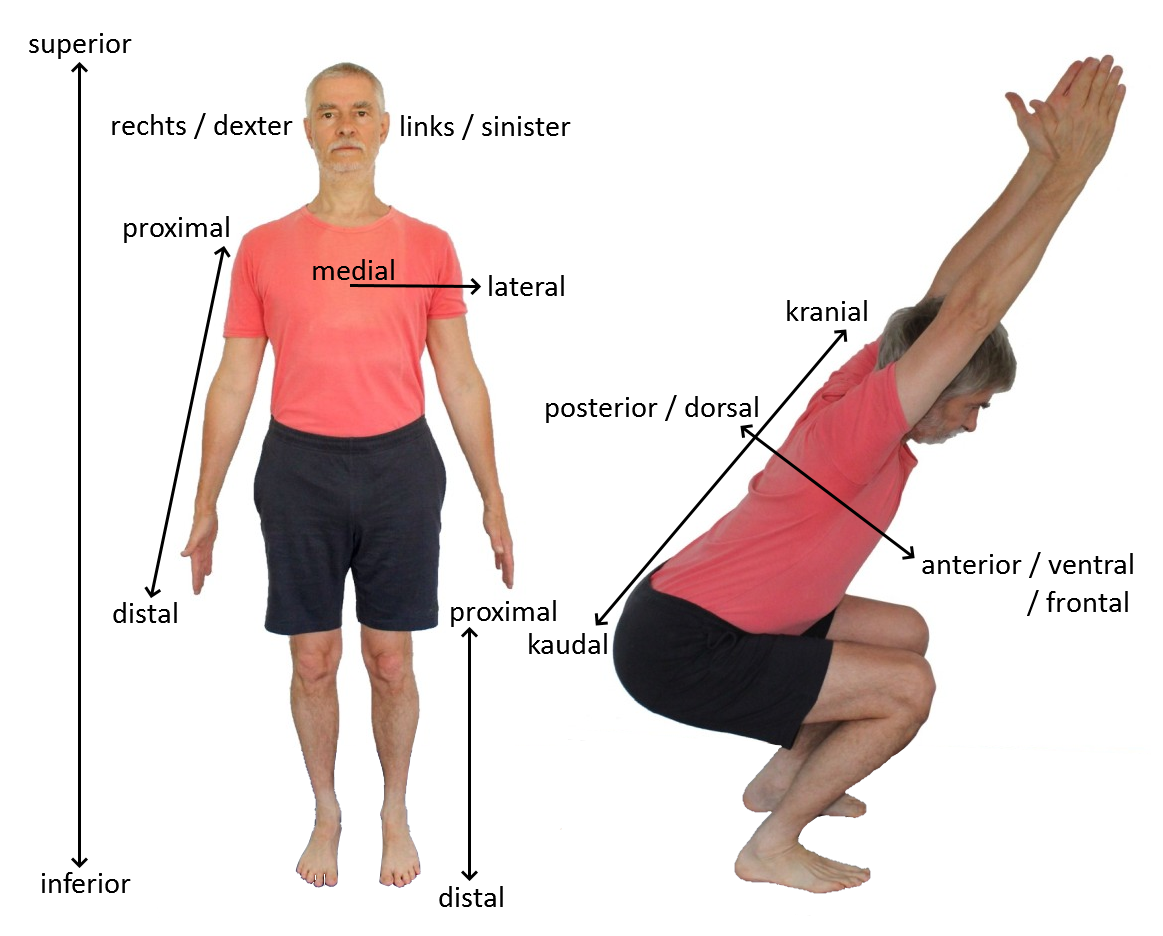
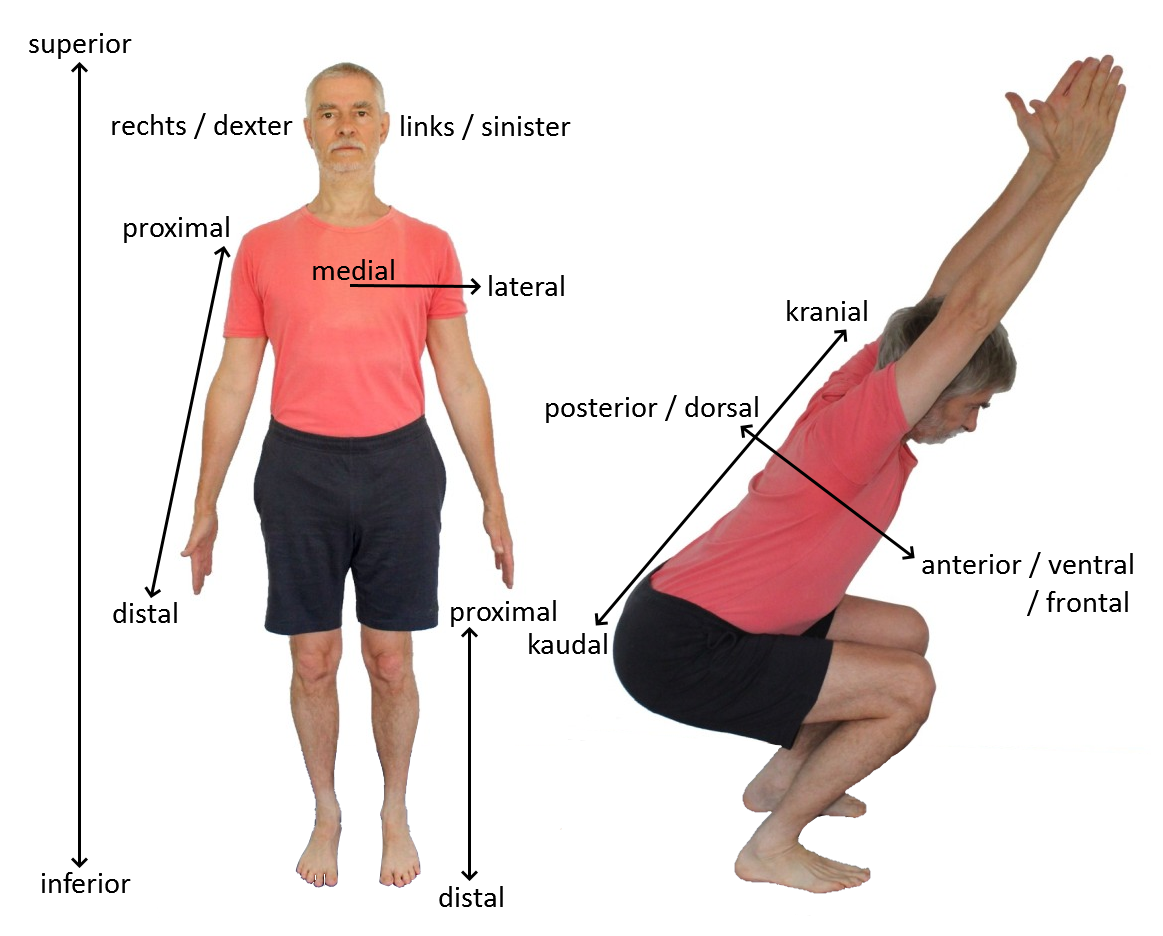
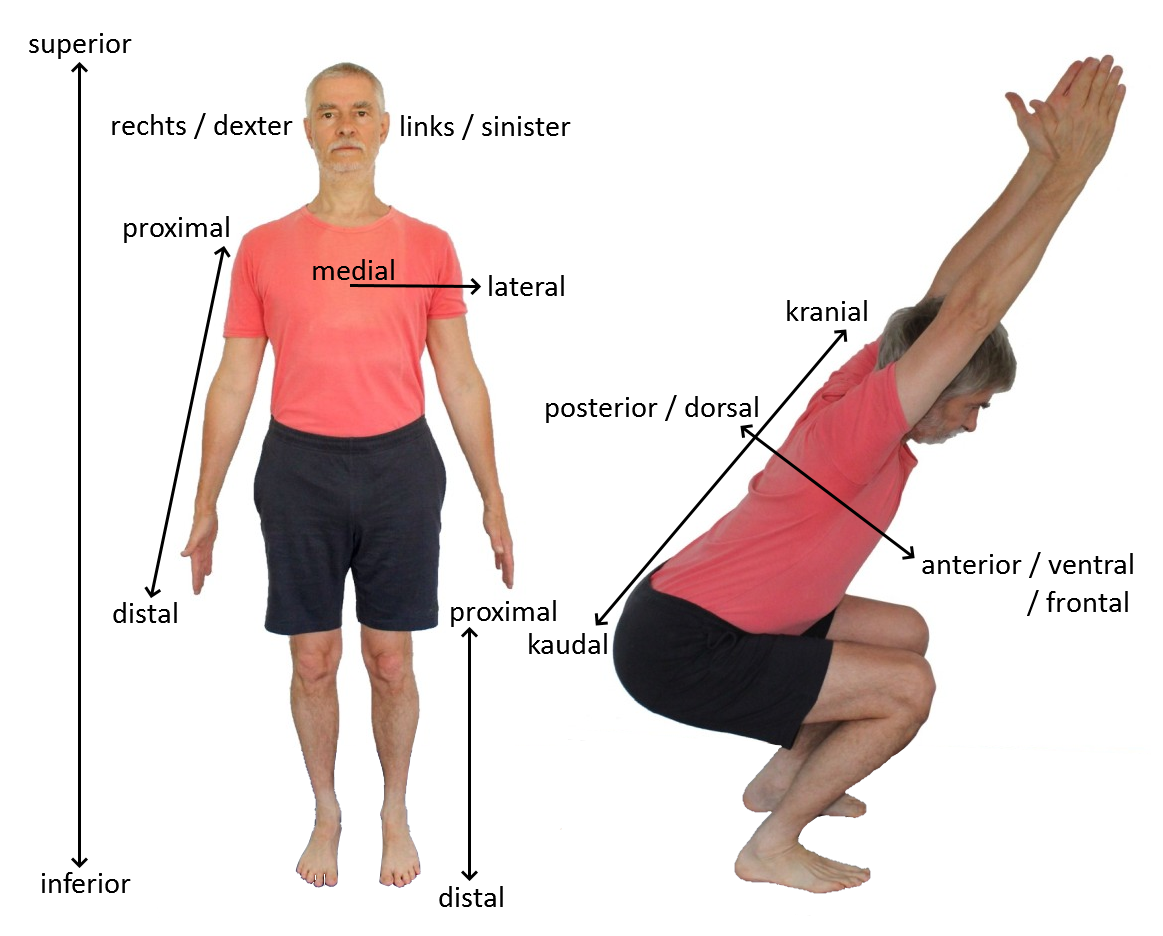
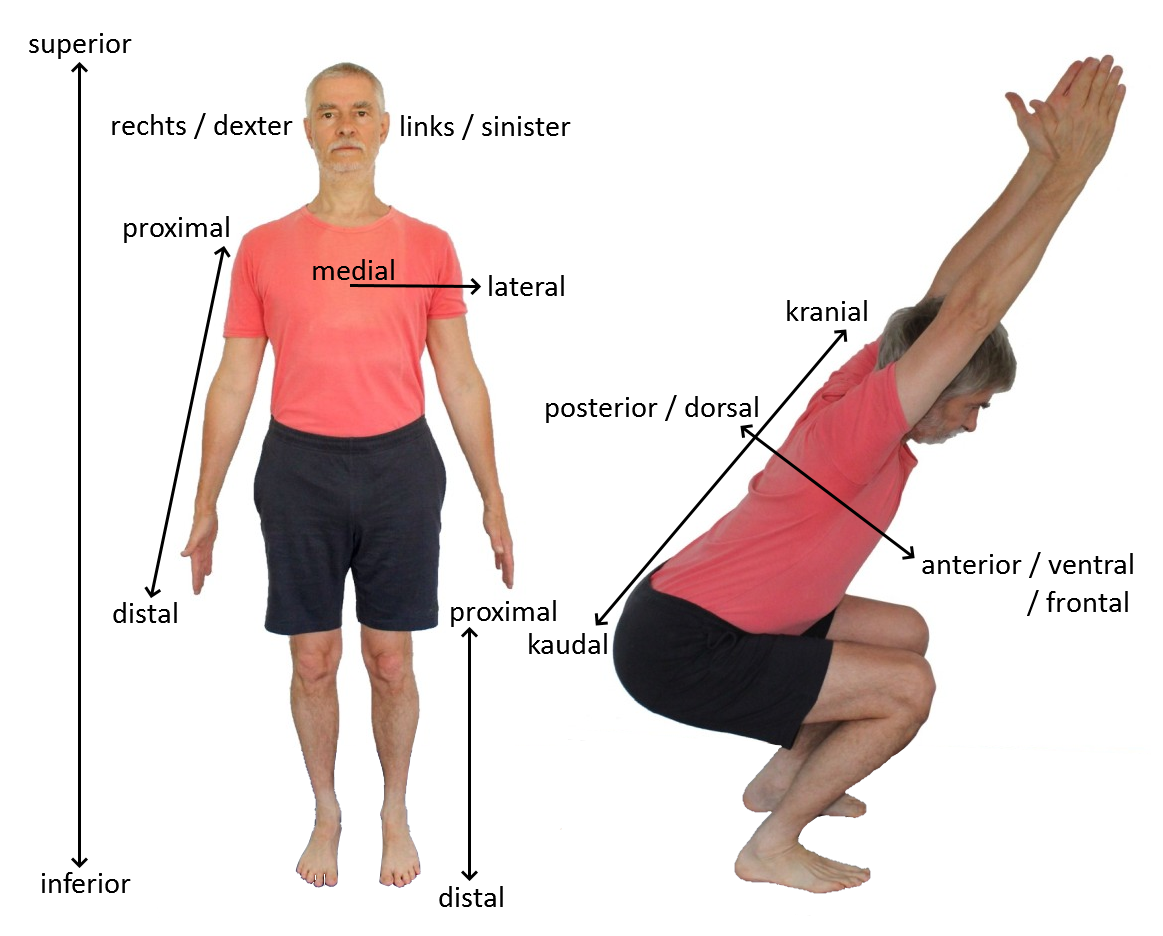
Anterior
denotes a direction and means „in front of or towards the front“ and is identical to the term frontal or ventral. The conceptual opposite is posterior, which in turn corresponds to the term dorsal.
Anteversion (arm / shoulder joint)
Synonym: frontal abduction, lifting the arm forward.
Aponeurosis
flat connective tissue structure that serves as a muscle insertion, including the palmar aponeurosis, the plantar aponeurosis, the retinaculum patellae or the rectus sheath.
Apophysis
see movement physiology – bone/apophysis.
Arachnoid mater
see movement physiology – nervous system/arachnoid mater.
Arch of the foot
The foot has two arches, the das Longitudinal arch of the foot and the Transverse arch of the foot.
– Longitudinal arch of the foot
The concave cavity of the foot seen from the plantar side in the longitudinal direction of the foot. In addition to the passive bracing (tension belt) consisting of the plantar long ligament, the plantar calcaneonavicular ligament and the plantar fascia, which act as a tension belt to prevent the longitudinal arch from collapsing, several muscles are also involved in maintaining this as active bracing: In the lower leg, the deep flexors:
In the foot:
- Abductor hallucis
- Flexor hallucis brevis
- Flexor digitorum brevis
- Quadratus plantae
- Abductor digiti minimi pedis
In addition to the pronounced medial longitudinal arch, there is a very slightly pronounced, relatively rigid lateral longitudinal arch, which is supported by the muscles
When walking and running, the longitudinal arch flattens (the foot extends) in the standing leg in order to rebuild itself during and after pushing off through the use of the plantar foot muscles. A reduction or collapse of the longitudinal arch results in a flat foot. See also the overview map of the dorsal foot muscles.
Transverse arch of the foot
The concave cavity of the midfoot and forefoot seen from the plantar side in the transverse direction of the foot. The passive tension consists of the transverse metatarsal ligament and the plantar cuboideonavicular ligament as well as the plantar aponeurosis, the active tension consists of the lower leg muscles
and among the intrinsic foot muscles, especially the:
- Caput transversum of the Adductor hallucis
A reduction or collapse of the transverse arch can be seen in a splayfoot, which is usually easily recognized by the formation of calluses in the area of the metatarsophalangeal joints 2-3. See also the overview map of the dorsal foot muscles.
Arm flexors
All muscles that perform or support flexion in the elbow joint. These are primarily the biceps, brachialis and brachioradialis. Of the muscles that attach to the medial humeral epicondyle, only the palmaris longus is still considered a weak flexor of the elbow joint. The other muscles that attach there, such as the superficial and profound finger flexors, flexor carpi radialis and flexor carpi ulnaris, are not considered as such, although they cover the elbow joint. The muscles attached to the lateral epicondyle of the humerus also do not support flexion.
Arm stretchers
all muscles that perform or support an extension in the elbow joint. The only muscle to which this applies is the triceps. The anconeus, which is also located on the dorsal side of the elbow joint, is so weakly effective as an extensor that most authors only consider it to tense the joint capsule.
Arthrodesis
Arthrodesis usually refers to the irreversible surgical stiffening of joints in the sense of permanent invasive stiffening using an inflexible technical material. This is used, for example, after destruction of the joint due to trauma, severe infections, rheumatoid arthritis or osteoarthritis (arthrosis). In the latter case, the permanent pain of activated osteoarthritis is relieved and the instability eliminated. However, arthrodesis may also be indicated for other conditions, for example if a joint has become unacceptably unstable and no other treatment option is available. Arthrodesis may also be necessary if an artificial joint (endoprosthesis) has become unstable and cannot be replaced.
Where an endoprosthesis is available that technically largely reproduces the joint function, this option is generally preferred. While TEP is commonly used for the hip and knee joints, (permanent) arthrodeses are used for the hand and wrist, the joints of the foot and the spine if indicated. The cartilage of the joint surfaces is removed and, if necessary, autologous bone substance (e.g. from the iliac crest spongiosa) is inserted to improve the result. Nails, screws and plates are available for fixation. Temporary arthrodeses are usually K-wires (Kirschner wires). In the area of the spine, arthrodeses are called spondylodeses. Arthrodeses cause a change in movement patterns and shift the motion to neighboring joints, which are exposed to additional stress as a result. Depending on the stiffened joint, the loss of joint function can be compensated for to a greater or lesser extent.
Artery
see movement physiology – blood circulation/artery.
Arteriole
see movement physiology – blood circulation/arteriole.
Arthrogenic muscle inhibition (AMI)
see movement physiology – muscle/AMI.
ASA Classification
The ASA classification of the American Society of Anaesthesiologists must be preoperatively performed by anesthesiologists in the context of premedication in order to assess the risk of anesthesia.
A distinction is made between ASA grades 1 and 6:
- ASA 1: healthy patient
- ASA 2: Patient with minor disease without restrictions
- ASA 3: Patient with disease with significant impairment
- ASA 4: Patient with life-threatening disease
- ASA 5: Moribunder patient who is unlikely to survive without surgery
- ASA 6: deceased patient with detected brain death, organ donor
In grades 2-5, the following lethality is observed:
- ASA 1: 0,06%
- ASA 2: 0.47%
- ASA 3: 4.39%
- ASA 4: 23.48%
- ASA 5: 50.77%
Aseptic bone necrosis
ischemic bone necrosis (caused by a lack of supply), as occurs in the following diseases:
- Scheuermann’s disease: top and bottom plates of the vertebrae
- Perthes‘ disease: head and neck of the femur
- Osgood-Schlatter disease: tibial tuberosity
- Osteochondrosis dissecans: Femoral condyles (articular mice/articular calculus)
- Kienböck’s disease: Os lunatum (hand)
- Köhler’s disease I: Os naviculare (foot)
- Morbus (Freiberg-)Köhler II: Heads of the metatarsal bones
Atony point
see movement physiology – muscle/atony point.
Atrophy
Physiological (e.g. by ageing or involutional atrophy: degeneration of organs that are no longer required, such as the thymus) or pathological reduction in the number (hypoplasia) or size (hypotrophy) of cells, which is associated with a loss of efficiency of the cell structure, furthermore with increased susceptibility and premature wear. There can be many different forms depending on the causes:
- Pressure atrophy: prolonged exposure to pressure
- Inactivity atrophy: prolonged non-use or immobilization
- Trophic and nervous atrophy: supply problems or lack of nerve impulses
- Endocrine atrophy: hormonal causes that lead to atrophy
- Skin atrophy: various causes
- Malnutrition (marasmus), emaciation (cachexia) in consumptive diseases such as tumors, TB
Attachment
The insertion of a muscle, tendon or ligament, which – in contrast to the origin – is located further distally, is usually referred to as an attachment.
Auscultation
Autochthonous back muscles
see movement physiology – autochthonous back muscles.
ANS (autonomic / vegetative nervous system)
see movement physiology – nervous system/VNS (autonomous nervous system).
Avulsion
Bony avulsion of a tendon, i.e. under load the tendon tears out a piece of bone at the insertion site. This occurs in particular when the bone structure is damaged, but sometimes also due to extreme (usually eccentric) load without pre-existing damage to the bone.
Avulsion fracture
Synonym for avulsion.
Axial misalignment
Axial misalignment is a deviation from the norm, usually of the extremities. The most common and best known are axial malalignments of the knee joint in the frontal plane: knock knees and bow legs. In addition, malalignments occur in the sagittal plane as genu recurvatum (extremely hyperextensible knee joint) and very rarely as genu procurvatum (extension deficit, for example due to arthrofibrosis, cyclops after cruciate ligament plastic surgery, meniscus entrapment) as well as in the transverse plane as internal and external torsion. Physiologically, the hip joint, the knee joint and the ankle joint lie on the same line, the Mikulicz line, the weight-bearing line of the lower limb. Physiologically, the knee joint has an external angle of 173° – 175°, which is caused by the angle in the femur (the CCD angle between shaft and neck). A deviation of the lower leg from its expected and physiological course towards the medial side, i.e. a varus position, is referred to as bow leg or genu varum. If the lower leg deviates outwards, i.e. there is a valgus position, this is known as a knock-knee or genu valgum. In the lower extremity in particular, axial misalignments usually lead to damage to the musculoskeletal system over time, not least depending on the intensity of use. Similar axial misalignments are occasionally found in the upper extremity, but with a few exceptions these often remain asymptomatic for longer due to the much less heavy use compared to the lower extremity (standing, walking, running). In the elbow joint, a small valgus position is physiological; up to 10° is considered physiological in men and up to 15° in women. Angles beyond this are considered cubitus valgus. Cubitus valgus and its varus counterpart cubitus varus usually have a traumatic background or result from a chronic tendency to dislocate. In asanas, care must be taken to ensure that the misalignments do not become more pronounced. Depending on the construction of the pose, the effect of gravity tends to further express an existing valgus or varus position, as the line of support does not run in a straight line through the joint, but results in a valgus or varus torque from the existing malposition. This can impair the ligament and cartilage structure and thus cause joint instability and arthrosis (osteoarthritis). As in the case of the knee joint, a realignment osteotomy would be considered after completion of longitudinal growth in the case of pronounced malalignment. If the function of the joint is impaired or nerves are affected, the decision may have to be made earlier. When performing asanas, an appropriate force must be built up in the respective joints of the trunk (shoulder joint or hip joint) in such a way that it neutralizes the damaging torque as well as possible. For example, if there is a clear valgus position of the elbow joint in purvottanasana with the hands pointing backwards, a force in the direction of lateral abduction must be built up in the shoulder joint; in the case of a varus position lateral adduction, of course. The same applies to the upface dog and downface dog. In general, when feet oder hands are punctum fixum, the force must be exerted in the opposite direction in which the limb mid joint (elbow joint, knee joint) deviates from the expected line, that is in the direction in which the limb end joint (wrist or ankle) deviates from the expected path. With the foot or hand as a punctum fixum a relieving moment in the limb mid joint is created. The rotational situation of the limb in the pose must be carefully observed. In the downface dog and all other overhead poses of the arms, external rotation is less possible, which slightly changes the direction in which pressure would ideally be applied.
Axon
see movement physiology – nervous system/axon.
B
Ball joint
see under movement physiology – joint shapes/joint shapes
Bankart lesion
Partial or complete avulsion of the lower glenoid labrum in the shoulder joint due to anterior dislocation of the shoulder joint. The Bankart lesion is a cause of recurrent dislocations. If the labrum alone is torn off, it is referred to as a soft lesion; if the bone is also affected, as in the case of an avulsion, it is referred to as a hard lesion.
biarticular
see movement physiology – muscle/biarticular.
Blood
see movement physiology – circulation/blood.
Blood-brain barrier
see movement physiology – circulation/blood-brain barrier.
Blood pressure
see movement physiology – circulation/blood pressure.
Blood vessel
see movement physiology – circulation/blood vessel.
Blood volumina
see movement physiology – circulation/blood volume.
Body Composition
To determine body composition, a CT scan is performed, usually a transverse section at the level of L3, from which the proportions of the various tissues are calculated:
- Area of skeletal muscle
- Area of visceral adipose tissue (VF)
- Area of subcutaneous adipose tissue (SF)
- Area of intramuscular adipose tissue (IF)
Furthermore, the skeletal muscle index (SMI) is calculated from the ratio of muscle area to body height: muscle area [cm²]/body height [m]². For the sake of simplicity, the summative values lean body mass (LBM) and lean muscle mass (LMM) are then often used.
Body mass
Body mass refers to the physical mass of the body. In application, however, the weight of this mass in the Earth’s gravitational field is usually more relevant. Various authors have given slightly different values for the parts of the body based on different samples, here are just a few examples.
| Amber Men / Women | Fisherman | Hochmuth | |
| Head | 6,72 / 8,12 | 7,06 | 8,1 |
| Trunk | 46,30 / 43,90 | 42,70 | 49,7 |
| Upper arm | 2,65 / 2,60 | 3,36 | 2,8 |
| Forearm | 1,82 / 1,82 | 2,28 | 1,6 |
| Hand | 0,70 / 0,55 | 0,84 | 0,6 |
| Thigh | 12,21 / 12,89 | 11,58 | 9,9 |
| Lower leg | 4,65 / 4,34 | 5,27 | 4,0 |
| Foot | 1,46 / 1,29 | 1,79 | 1,4 |
The centers of gravity of the partial body weights of these body parts lie relatively exactly on the lines connecting the joint rotation centers. In the case of the extremities, they can be specified as proximal proportions of the total distance between the rotation centers of the joints as follows:
upper arm: 47%,
forearm 42%,
thigh 44%,
lower leg 42%,
foot 44%.
This reflects the fact that the limbs of the extremities narrow distally. The center of gravity of the head is approximately midway between the auditory canals, that of the torso at about 44% of its length cranially.
BMI (Body Mass Index)
The BMI is now an outdated measure for determining obesity. It fails because fat and muscle mass are not differentiated, so that the BMI falsely certifies muscular athletes as overweight. The BMI is calculated for adults from the age of 18 as body weight : (height)^2 and is roughly divided into the following ranges:
- up to 16: critical underweight
- 16 to 18.5: slightly underweight
- 18.5 to 25: normal weight
- 25 to 30: slightly overweight
- over 30: overweight
A modified formula is available for children between the ages of 2 and 17. The Waist-to-Height-Ratio is much more helpful than the BMI.
Here you can find a calculator for WHtR and BMI.
Body Shape Index
The Body Shape Index (BSI) developed by Nir/Krakauer takes into account height, waist circumference and BMI to calculate an index that also measures abdominal visceral fat: U * (l^5/BMI^4) ^ 1/6 or U /(BMI^(2/3) * l^(1/2)). From 0.083 onwards, the risk of various diseases is considered to be increased, and from 0.091 onwards, it is considered to be doubled. If the individual BSI is set in relation to the mean value (population) and the standard deviation, the ABSIz value is obtained, from which risk groups can be derived:
- up to −0.868: very low
- up to −0.272: low
- up to +0.229: normal
- up to +0.798: high
- above +0.798: very high
The BSI addresses the cardinal flaw of the BMI, which fails to distinguish between muscle and fat and classifies muscular athletes with a high BMI as at risk. By including waist circumference in the numerator of the term, a distinction is made between muscle distributed throughout the body and fat located in the abdominal area.
bone
See movement physiology – bone and the overview of all bones.
Bone adaption
see movement physiology – bone/bone adaption.
Bone marrow
see movement physiology – bone/bone marrow.
bounce / bounce reversal
In strength training, reversal of momentum refers to the process of transitioning from eccentric to concentric contraction, which is performed in such a way that the eccentric contraction is not slowly stopped at the end, but before the end of the (often inertial) eccentric contraction, the muscles are innervated as strongly as is required for the concentric contraction and also for overcoming the inertia required in this situation. As a result, fewer muscle fibres need to be recruited, which makes the reversal easier than it would be after a stop. The effect can be in the order of 30%. In the process, kinetic energy is stored in the elasticity of the tendon, which can then be used for concentric contraction. The danger here is that the tendon elasticity is usually significantly overestimated by the performers, so that cumulative damage to the tendon to symptomatic insertion tendopathy or even tendon rupture. Depending on the robustness of the bone tissue.
Bounce momentum
The kinetic energy that is stored in the bounce (reversal) and facilitates the concentric contraction. The bounce (reversal) is often referred to as the bounce itself.
Bradycardia
see movement physiology – circulation/bradycardia.
Bradypnoea
see movement physiology – circulation/bradypnoea.
bradytrophic
Bradytrophic means slow-metabolizing. This describes a property of tissues and reflects their metabolic rate and their turn over. Tissues with a slow metabolism often take more than a year to completely regenerate; in the case of cartilage, this can no longer take place at all due to the very slow metabolism. As a result, they heal very slowly after injury and regenerate very slowly after stress. Many of the bradytrophic tissues are not supplied by arteries and are therefore not permeated with capillaries, but are only supplied by diffusion through changing pressure in movement. This applies to cartilage and parts of the bones, for example. However, there are also mixed forms, such as the meniscus of the knee, which is capillarized on the outside and not on the inside. With their slow metabolism, slow healing and slow regeneration, they are preferentially affected by overuse syndromes. The conceptual opposite of bradytrophic is tachytrophic.
Bursa
The bursae are fluid-filled cushions, usually in the course of muscles or tendons, to keep local pressure peaks away from them. For example, the iliopectineal bursa buffers the course of the iliopsoas tendon via the eminentia iliopubica. When the hip joint is extended, the line connecting attachment and origin of the iliopsoas lies behind the eminentia iliopubica, so that there must be significant pressure on the tendon. Without a bursa, the tendon would quickly become irritated and degenerate.
Bursae can be connected to a regional joint and are then described as communicating with it. Bursae can also communicate with each other.
A distinction is also made between bursae that are present at birth (constant) and bursae that have developed as a result of triggers (inconstant).
– Structure of the bursa
Bursae consist of two layers:
- Membrana fibrosa (outer layer, also known as stratum fibrosum): consists mainly of collagen fibers
- Membrana synovialis (inner layer): produces and, if necessary, reabsorbs synovial fluid and thus enables smooth, pain-free movement.
– Classification according to buffer function
- Bursa subcutanea, especially where skin lies directly on bone
- Tendon bursa (bursa subtendinea) between tendons and bone
- Intervertebral bursa (subligamentousbursa) between ligaments and bone
- Muscle bursa (submuscularbursa) between muscles and tendons or bones
- Fascial bursa (subfascialbursa) between a fascia and the underlying bone
– Classification according to occurrence
- constant / congenital: occurring in the same place in all people
- inconstant / reactive: acquired. Skin bursae are always reactive.
An overview of many burses in the human body can be found here.
C
Callus
see movement physiology – bone/callus.
Capillaries
see movement physiology – circulation/capillaries.
Capsule
see movement physiology – joint/capsule.
Capsule ligament
see movement physiology – joint/capsule ligament.
Capsulitis
see movement physiology – joint/capsulitis.
Cardiac output CO
see movement physiology – circulation/cardiac output.
Carpal tunnel
Palmar depression in the carpus (entirety of the carpal bones) through which the median nerve, the tendons of the profund finger flexors (flexor digitorum profundus muscle), superficial finger flexors (flexor digitorum superficialis muscle) and the long thumb flexor (flexor pollicis longus muscle) run. Some authors also include the flexor carpi radialis muscle. The carpal tunnel is covered by a retaining ligament (retinaculum), the flexor retinaculum. Swelling of the tendons can lead to pressure on the nerve and thus to carpal tunnel syndrome, a nerve compression syndrome.
Carpus
The entirety of the carpal bones, see under bones of the hand.
Cartilage
see movement physiology – joint/cartilage,
movement physiology – joint/hyline cartilage,
movement physiology – joint/fibrocartilage,
movement physiology – joint/elastic cartilage.
catabolic / catabolism
Catabolism usually refers to metabolic reactions that break down substances. These reactions serve to generate energy, eliminate waste/detoxify, and provide building materials. Stress and strain have a catabolic effect because they require energy and, in some cases, building materials. Catabolism and anabolism together form metabolism. Either anabolic or catabolic reactions occur in a cell, but not both at the same time. Necrosis leads to catabolism, while physiological growth processes reduce catabolism.
cauda equina
see movement physiology – nervous system/cauda-equina.
Caudal
refers to a position close or (in comparison) closer to the lower end of the trunk. The conceptual opposite is cranial.
Causalgia
see movement physiology – nervous system/Causalgia.
Center of gravity
The center of gravity of a (usually 3-dimensional) body is the mass-weighted average of the positions of its mass points and is therefore also simply referred to as the „center of mass“; a more correct term would be „mass-weighted average“. This means that the center of mass does not necessarily have to be in the body; counterexamples are a boomerang or a person standing in downface dog of in the back arch.
CNS (central nervous system)
see movement physiology – nervous system/CNS (central nervous system).
Cerebrospinal fluid
see movement physiology – nervous system/cerebrospinal fluid.
Cervical spine (cervical spine)
The part of the spine consisting of 7 vertebrae above the thoracic spine and below the occiput (occipital bone). The uppermost vertebrae C1 (atlas) and C2 (axis) have a special shape to allow maximum rotation.
Circumduction
Circumduction (pathological or unphysiological) refers to a circular movement of the leg in the hip joint when the hip flexors, the muscles that can move it forward in a straight line, fail, are insufficient or are too weak to meet the requirements. In the Wernike-Mann gait pattern, this can be seen as a consequence of apoplexy, for example, but multiple sclerosis can also lead to this.
Chondrosis
In principle, chondrosis refers to any cartilage degeneration, but the term is usually used as chondrosis intervertebralis in relation to the intervertebral discs. With increasing age, the intervertebral discs change adversely in several ways: the proteoglycan content of the nucleus pulposus decreases, which reduces the water-binding capacity (swelling capacity), and the collagen content increases, which makes the nucleus pulposus firmer and harder. In addition, defects develop in the annulus fibrosus, in which the fibrous tissue arranges itself into fibrils, which can allow the passage of material from the nucleus pulposus and cause a prolapse. Overall, the intervertebral disc loses height, which is consistent with the decrease in height with age, even without a change in the shape of the spinal column, for example due to hyperkyphosis of the thoracic spine. Chondrosis of the intervertebral discs puts a strain on the facet joints, so that sooner or later these will lead to osteoarthritis (arthrosis) called spondylarthrosis, which often results in facet syndrome. Furthermore, the risk of disc hernias (herniated and bulging discs) increases. In addition, the changes in the intervertebral disc affect the vertebral body, which tends to develop spondylosis, which can be seen radiographically as irregularly compacted top and bottom plates; spondylophytes (osteophytes of the vertebral body) are also common. Spondylosis is known to be a natural sign of ageing in many vertebrates.
Cold
Cold is physically a lower degree of molecular vibration. This is an aggravating factor for physiology. Muscles are less elastic in the cold, blood circulation in the body in general and in the muscles in particular is poorer because the capillaries contract in response to the cold so that less heat energy is lost to the outside world. The synovia becomes more viscous and joint lubrication deteriorates. As a result of these factors, performance decreases and the risk of injury increases significantly. Moisture is an important cofactor of cold due to increased thermoconductivity.
Collagene
Collagen is a group of structural proteins that form fibre bundles and are mainly found in connective tissues in humans (tendons, ligaments, bones, cartilage, blood vessels and teeth). It makes up around 25-30% of the total mass of proteins in humans. Collagen molecules are long amino acid chains that form a left-handed helix. Three of these helices are interwoven to form a dextrorotatory superhelix (tropocollagen) stabilised by hydrogen bonds, the actual collagen. The helix is very elongated, the pitch (from one turn to the next) is 0.94 nm compared to 0.54 nm for an alpha-helix. Above all, collagen has an extraordinary tensile strength. Collagen is divided into several types, of which type 1, type 2 and type 3 are of outstanding importance in the movement apparatus. There are also a further 25 types of collagen. Tropocollagen is organised in fibrils, each containing the collagen molecules offset by a fifth of their length (equivalent to 67 nm). Collagen is formed in the extracellular space and its organisation is controlled by fibroblasts. The diameter of the collagen fibrils ranges from 20 nm to 500 nm, depending on the type. The production of collagen is dependent on ascorbic acid (vitamin C).
Collagen type 1
Collagen type 1, the most common, is found in skin, tendons, fascia, bones, blood vessels, internal organs and dentin and forms thick, firm fibres with high tensile strength. Type 1 is altered in osteoporosis imperfecta and Ehlers-Danlos.
Collagen type 2
Collagen type 2 is a structural protein of the hyaline and elastic cartilage as well as the vitreous body of the eye. It tends to form looser or thinner fibres and elastic tissue.
Collagen type 3
Collagen type 3 is a component of granulation tissue and is also found in vascular walls, internal organs, skin, uterus and cornea. It also forms rather loose or thinner fibres and its elasticity is used in skin, blood vessels and internal organs.
Collateral ligaments
Collateral ligaments are ligaments of joints that lie parallel to the extension of a part of an extremity and not on the flexor or extensor side, but medially or laterally. In the example of the knee joint, these are the medial and lateral collateral ligaments.
Collateral ligament (knee)
the inner and outer ligaments running longitudinally on the medial and lateral side of the knee joint, which tighten when the knee joint is extended and thus prevent internal rotation and external rotation of the lower leg in the knee joint. Another function of the collateral ligaments is to prevent varus movements and valgus movements by absorbing corresponding forces. See knee joint: Collateral ligaments.
Communicating / communicating
Connection between two spaces, to be physiologically connected. This term is used, for example, when two bursae are connected to each other or when a bursa is connected to the associated joint space, i.e. a connection exists between them that allows the exchange of synovia. If a communicating bursa is referred to without specifying a further anatomical structure, communication with the joint cavity is meant.
Compact bone
see movement physiology – bone/compact bone.
concentric muscle failure
see movement physiology – muscle/concentric muscle failure.
Condyle
see movement physiology – joint/condyle.
Condyloid joint / ellipsoidal joint
see under joint shapes
Congruence
see movement physiology – joint/congruence.
Constant
Property of an anatomical structure to be regularly developed in all people. Examples include bursae or ligaments, which all people develop, whereas others are not found regularly and are then called inconstant.
Contraction
See movement pyhsiology – muscle/contraction.
Contraction, concentric
See movement physiology – muscle/concentric contraction.
Contraction, types of
See movement physiology – muscle/contractions, types of.
Contraindication
A contraindication is a circumstance that prohibits the use of a remedy or procedure, here a pose, an exercise, the use of an aid, a transition or something else.
Contract
refers to a fixed misalignment that can no longer be brought into the physiological position as the conceptual opposite of reducible. Contractual malpositions cannot be corrected conservatively.
Contractile force / Contractive force
See movement physiology – muscle/contractile force
Coronary artery
See movement physiology – circulation/coronary artery.
Corrective osteotomy
also known as axial correction: surgical removal of a wedge-shaped piece of bone to correct an incorrect joint position. The corrective osteotomy is mainly used for the two large joints of the lower extremities, for the knee joint in the case of pronounced knock knees or bow legs or for the hip joint, for example in Perthes‘ disease. The aim of the osteotomy is to prevent serious damage that is to be expected as a result of the malalignment, such as arthrosis in the case of knee malalignment or necrosis of the femoral head in the case of Perthes‘ disease.
correlation
Correlation refers to a relationship between variables that is not necessarily causal, either positive or negative, such that in the case of a „positive correlation,“ the second variable increases or decreases with the first, and in the case of a „negative correlation,“ the two behave inversely: if one increases, the other must decrease. Correlation is a fundamental statistical measure of relationship. For example, a higher VO2max correlates with lower all-cause mortality, whereas all-cause mortality correlates positively with systolic blood pressure. In some cases, the two variables have a common cause, but this is not necessarily the case. Correlations are non-directional, meaning that, unlike an implication, for example, they can be read from left to right and from right to left. The correlation coefficient uses a number between -1 and 1 to indicate how strong and how directional the relationship is, with large values representing a strong relationship and small values representing a weak one. No relationship is indicated by the value 0. Negative values indicate a negative correlation, which is stronger the closer the number is to -1.
Cortikal bone
see movement physiology – bone/cortical bone.
Cranial
refers to a position near or (in comparison) closer to the upper end of the trunk or head. The conceptual opposite is caudal.
Cranial nerves
see movement physiology – nervous system/cranial nerves.
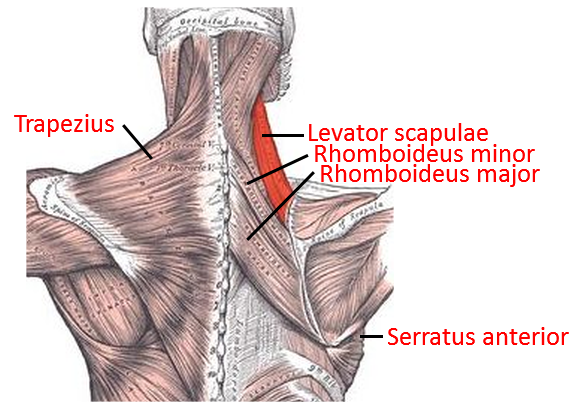
craniocingular muscles
Muscles that run from the skull to the shoulder blade:
Crepitations
The term crepitations, usually used in the plural, refers to a palpatory or auscultatory „crackling“ or „rustling“, sometimes also referred to as „crackling rattle“. This also includes „snowball crunching“, which is typical of tendovaginitis. Other conditions with crepitations are fractures and advanced osteoarthritis, in which bones (instead of their cartilage surfaces) are rubbing against each other.
cross-bridge cycle
see movement physiology – muscle/cross-bridge cycle.
Cruciate ligament
the two ligaments that run extra-articularly but intracapsularly in the knee joint and prevent the tibia from shifting ventrally or dorsally in relation to the femur: anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). If they are damaged, unphysiological displacements occur, resulting in instability during movement and increased wear of the knee joint. Damage such as overstretching and tears can be recognized by the anterior or posterior drawer effect. For more information, see knee joint: cruciate ligaments.
Cubital tunnel
lateral depression in the elbow area, a few centimeters proximal and distal to the elbow joint, through which the ulnar nerve runs, which primarily supplies the 4th and 5th fingers. Therefore, prolonged pressure on the nerve or trauma can lead to cubital tunnel syndrome (sulcus ulnaris syndrome, ulnar groove syndrome), the second most common nerve compression syndrome in humans.
Cyclical movement
A cyclical movement is a sequence of movements whose end is identical to the beginning, so that it can be performed as often as desired in succession. Examples include all forms of walking, running, sprinting, but also the dips of the downface dog, of the handstand, of the staff pose, caturkonasana jumping or – in sporting disciplines – the bench press or rowing. Basically, most forms of locomotion that allow you to cover a greater distance belong to the cyclical movement patterns.
Cycling
see movement physiology – cycling.
Cytokines
Cytokines are proteins with autocrine, paracrine and endocrine effects that enable cells to communicate with each other. These include, in particular, interferons (IFN-α, IFN-β, IFN-γ) and interleukins (currently 35 are known), as well as tumour necrosis factors (TNF-α, TNF-β/LT-α, TNFγ/LT-β). In addition, there are colony-stimulating factors and tissue-specific cytokines such as apidokines, myokines, osteokines and neurokines. The main difference between cytokines and hormones is that hormones are produced and secreted by dedicated glandular cells, whereas cytokines are produced by any cell in a cell cluster. Apart from this, the concentration of cytokines in the interstitium or serum is usually about 1000 times lower, but can also increase by this amount in the event of infection or trauma.
D
Dead space / dead space volume
see movement physiology – circulation/dead space volume.
Degree of strength
In the case of muscular, neurological or other diseases that affect muscle performance, a distinction is made between six degrees of strength:
- 0 = Plegia = complete lack of movement in the muscle
- 1 = visible muscle twitching without movement
- 2 = visible muscle twitching with minimal movement
- 3 = muscle movement in the limb without overcoming gravity
- 4 = muscle movement in the limb with significant weakness
- 5 = full strength
Dehiscence
Pathological persistence of a gap between two anatomical structures, tissues or within a tissue after trauma. Dehiscence can result from the intrinsic tension of the tissues or, as in the case of the tendon, from the tone of its muscle, which pulls the tendon stump still attached to the muscle away from the enthesis.
Dendrite
see movement physiology – nervous system/dendrite.
Depression (shoulder blade)
Downward movement of the shoulder blade (caudal, towards the pelvis). The scapula is (terminologically) „depressed“. The muscles performing the movement are the depressors of the scapula. The counter-movement is called elevation.
Depressors (shoulder blade)
Muscles that move the shoulder blade caudally, i.e. in the direction of the pelvis:
- Trapezius (pars ascendens, most important dorsal depressor)
- Latissimus dorsi (only indirectly)
- Serratus anterior (directly)
- Pectoralis minor (directly, most important ventral depressor)
- Pectoralis major (only indirectly)
Dermatome
see movement physiology – nervous system/dermatome.
Diaphysis
The area of a long bone between the growth plates. This is where the bone marrow is located.
Diastole
See movement physiology – circulation/diastole.
Diastolic
See movement physiology – circulation/diastolic.
Diastolic blood pressure
See movement physiology – circulation/diastolic blood pressure.
Dimension of movement
see movement physiology – joint/dimension of movement.
Dips
Training form with cyclical movement in which flexion and extension of the elbow joint are used to strengthen the triceps using the body’s gravity. The position of the body in relation to the arms can vary. This makes dips the analogy to squats, as both strengthen the extensors of the middle joints of your limb.
Disc meniscus / Meniscus disciformis
Contrary to previous opinion and according to the latest research, this is not a congenital anomaly of the meniscus shape, but rather an anomaly acquired as a result of incorrect mechanical loading, in which the inner meniscus is rarely (5%), but usually (95%) the outer meniscus is not crescent-shaped, but rather disc-shaped, in 20% of cases also bilaterally. No disc meniscus has yet been detected in the embryonic stage. The disc meniscus often remains asymptomatic and undetected for a long time. The disc meniscus was described by Young as early as 1889. Depending on the literature, 0.4% to 17% of the population are affected, and in Asian countries, especially Japan, significantly more. Pinching of the meniscus between the tibia and femur can lead to a reproducible, usually painful snapping phenomenon, which does not usually occur before the 6th – 8th year of life. MRI can detect the disc meniscus. It tends to have central tears. Its fixation can vary greatly, which can lead to free flexibility, pressure on the joint capsule or locking of the joint with corresponding pain. Tears are an indication for arthroscopic removal and restoration of a physiological shape. If the meniscus proves to be insufficiently fixed, this must also be repaired. Complete removal of the meniscus, even of just the lateral or, rarely necessary in this context, the medial part, leads to a tens of times higher risk of arthrosis, which is why it must be avoided without the strictest indication.
Distal
refers to a position in a limb far or (comparatively) further away from its attachment to the trunk. The conceptual opposite is proximal.
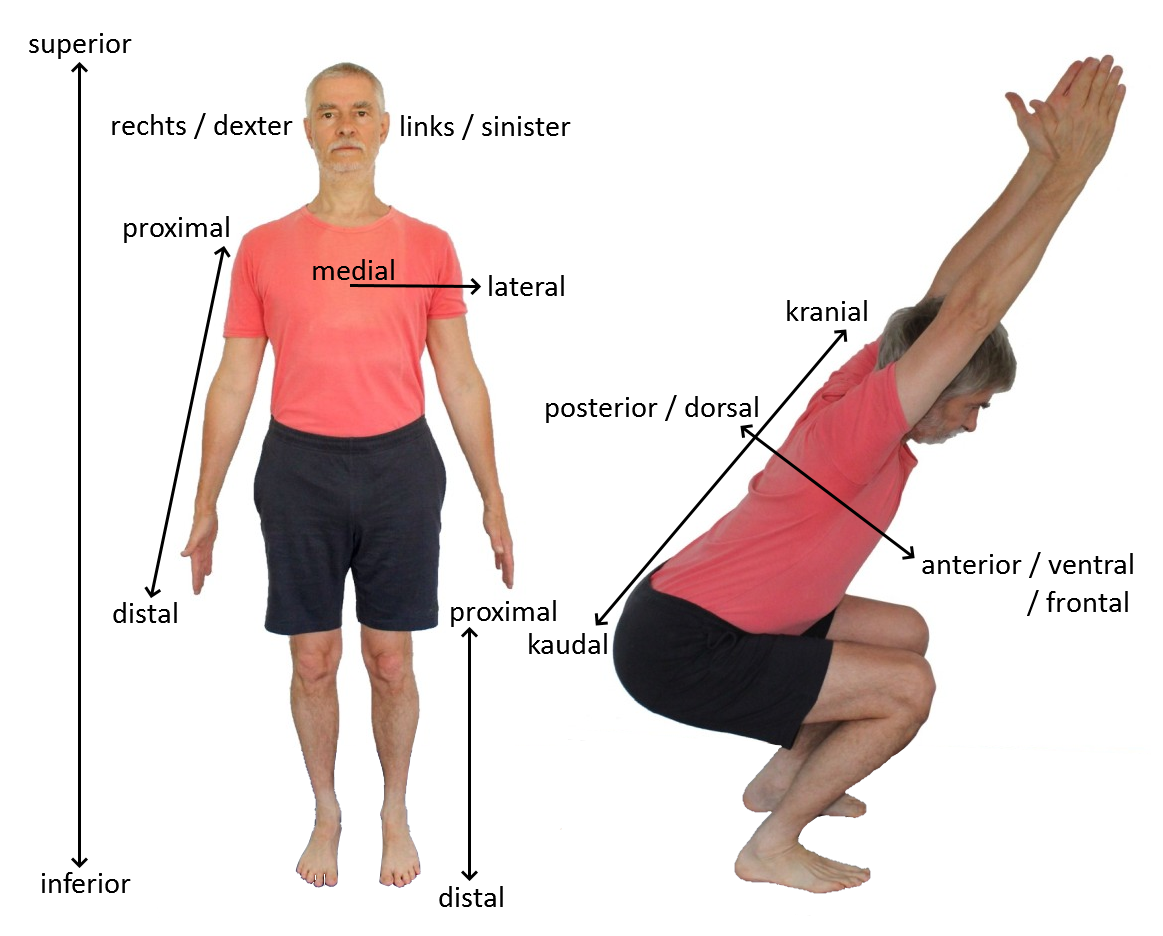
Dorsal
denotes a direction and means „on the back“, „behind“ or „to the rear“ and is identical to the term posterior, except that the latter is hardly used in limbs. The conceptual opposite is frontal, which in turn corresponds to the term anterior or ventral.
Dorsal flexion (foot)
Reduction of the dorsal (back of the foot) angle of the foot to the lower leg. This movement is carried out by a group of muscles that are also referred to as „dorsiflexors“. For the kinetics of walking, the foot dorsiflexors are of much less importance than the plantar flexors, which (depending on the walking style) can make a significant contribution to propulsion through extension (plantar flexion) in the ankle. In addition to the monoarticular soleus, this is primarily the gastrocnemius, which also flexes in the knee joint, giving it a favorable working range, as the knee joint is flexed and the ankle dorsiflexed when stepping forward, but the opposite occurs in both joints when pushing backwards: palmar flexion and extension in the knee joint. A comparable structure is completely absent in the dosriflexors, none of them covers the knee joint. This is also not necessary, as the force they can exert is far less, as they only have to prevent the toes from hitting the ground through dorsiflexion of the ankle when the foot is pulled forward for the next step, but as mentioned above, they do not have to contribute to propulsion.
Dorsal flexion (hand)
Reduction of the dorsal (back of the hand) angle of the hand to the forearm in the wrist.
Dorsal hip muscles / pelvitrochanteric muscles
see the movement physiology – dorsal hip muscles.
Dorsal flexors (foot)
These are generally referred to as dorsiflexors, see there.
Dorsiflexors (foot)
All muscles that perform dorsal flexion in the ankle (more precisely: the ankle joints, although this movement occurs almost exclusively in the ankle and only very subordinately in the Chopart and Lisfranc joint lines), i.e. reduce the dorsal (dorsalis pedis) angle of the foot to the lower leg or move the dorsum of the foot towards the lower leg. These are M. extensor hallucis longus, M. extensor digitorum longus, M. tibialis anterior.
Dorsiflexors (hand)
Muscle group that moves the back of the hand towards the forearm:
- Extensor digitorum
- Extensor digiti minimi
- Extensor carpi ulnaris
- Extensor carpi radialis longus
- Extensor carpi radialis brevis
- Abductor pollicis longus
- Extensor pollicis longus
- Extensor indicis
Dura mater
see movement physiology – nervous system/dura mater.
Dyskinesia
Disturbance of the physiological movement sequence: disruptive factors lead to non-physiological movement. In addition to the musculoskeletal system, this term is also used in other disciplines.
Dysphagia
Difficulty swallowing.
Dyspnea
Shortness of breath.
Dystrohpy
Misgrowth of tissue, but in contrast to atrophy due to genetic or traumatic causes or in the context of diseases such as Sudeck’s disease (CRPS 1) or Duchenne muscular dystrophy. As with atrophy, there is a reduction in the performance of the cell structure, increased susceptibility and premature wear and tear.
E
EAMC (Exercise Associated Muscle Cramp)
Everyone’s tendency to cramp is different, but it can be said that physical exertion, if it is very intense or in short sarcomere length or performed at a certain minimum intensity over a longer period of time, can lead to a cramp (see here) in the relevant muscles in most people. The tendency to cramp generally increases with rising ambient temperatures, compared with normal room temperatures. Markedly lower ambient temperatures also increase the tendency to cramp. Furthermore, a lack of electrolytes is an important predisposing factor. Like other cramps, EAMC can be stopped by targeted stretching.
Eccentric contraction
See movement physiology – muscle/eccentric contraction.
Eccentric muscle failure
see movement physiology – muscle/eccentric muscle failure.
efferent
see movement physiology – nervous system/efferent.
Elevation (shoulder blade)
Movement of the shoulder blade upwards (cranial), away from the pelvis. The executing muscles are the elevators of the scapula. The opposite movement is called depression. The elevation of the shoulder blade corresponds to its elevation when shrugging. The further the arms are abducted (laterally or frontally), the more the possible elevation depends on the flexibility of the latissimus dorsi and subordinate also the pectoralis major, for example, which – attached to the main trunk – are indirect depressors of the scapula. In an upright posture, elevation occurs against the force of gravity, so that it is automatically reset from its effect. Nevertheless, many people keep their shoulder blades partially elevated for endogenous reasons, which leads to tension in elevators such as the levator scapulae or the trapezius.
Elevators (shoulder blade)
Muscles that move the shoulder blade cranially, i.e. towards the head:
- Trapezius pars descendens
- Levator scapulae
- Rhomboideus major
- Rhomboideus minor
- Serratus anterior
Ellipsoidal joint / Condyloid joint
see movement physiology – joint shapes.
Elongation
Elongation refers to the non-physiological stretching of tissues or structures such as muscles, tendons, ligaments or vessels, often referred to as overstretching. In the case of an elongated ligament, it is insufficient in terms of its function to limit movement between the connected bones in a physiological manner. The joint therefore loses stability, which can promote the development of osteoarthritis. If a tendon is elongated, depending on the extent, this can mean that the muscle can no longer move the bone to which the muscle is attached via this tendon through its entire physiological range of motion. If it is significantly elongated, even when the muscle is fully contracted, no force is exerted on the bone, which means that the muscle no longer has any resistance against which it can be trained. This also eliminates the possibility of increasing its tone through training so that it can compensate for the elongation of the tendon. This muscle is therefore non-functional.
Endocardium
see movement physiology – circulation/endocardium.
Endurance
Endurance is the physical ability to perform prolonged exertion, i.e. the resistance to fatigue and the ability to regenerate quickly. Endurance is one of the basic components of fitness. This usually relates to sporting activities, but is not limited to these. In working life, too, endurance is sometimes required. At its simplest, endurance is the ability to perform more or less consistently over as long a period as possible. The slight vagueness of „more or less constant“ refers to the fact that, in practice, topographical conditions or wind modulate the performance requirement when running, for example. In addition to the absence of physical fatigue, mental endurance, i.e. the absence of mental fatigue, is also a not insignificant factor, whereby both factors influence each other. Endurance also includes recovering as quickly as possible after a performance.
Endurance sports
see movement physiology – endurance sports.
Energy
Energy is the quantified ability to cause something, be it in the form of work or radiation, i.e. also heat. Energy occurs in various forms that can basically be converted into one another, for example as potential, kinetic, electrical, chemical and thermal energy. When a person lifts an object, they „consume“ chemical energy and add potential energy to the object. If you accelerate your bicycle, you convert chemical energy into kinetic energy. A conventional filament bulb converts electrical energy into 95% heat radiation and 5% light radiation.
Enthesiopathy (Enthesopathy)
Synonymous with insertional tendopathy, the ischaemic or overuse-induced degenerative tendinopathy.
Epicardium
see movement physiology – circulation/epicardium.
Epicondyle
see movement physiology – bone/epicondyle.
Epiphysis / Epiphysis ossis
see movement physiology – bone/epiphysis.
Epiphyseal joint / growth plate
see movement physiology – bone/epiphyseal plate.
Eversion (foot)
Eversion, as the exact opposite movement to inversion, is the sum of movements in the lower ankle joints (posterior lower ankle joint/subtalar joint and Chopart joint line) and dorsiflexion in the upper ankle joint: eversion consists of pronation, dorsiflexion and abduction.
Examination methods / physical examination methods
Methods of physical examination include:
excitatory
see movement physiology – nervous system/excitatory.
Exclusion diagnosis
A diagnosis of exclusion is an entity (disease) that remains after all entities compatible with the differential diagnosis of a given finding (the set of all information from anamnesis, clinic, examination methods) have been excluded by all (currently relevant) examinations.
This does not mean that the exclusion diagnosis must be unambiguous, but no counterexample is known to date. However, unambiguousness can be achieved by formulating the exclusion diagnosis in a correspondingly comprehensive manner. A disease can only be a diagnosis of exclusion if there is no direct detection procedure using investigative methods for it. The term „diagnosis of exclusion“ reflects the current state of knowledge through the phrase „currently relevant“. Scores can substantiate the suspicion of a diagnosis of exclusion, but by definition they do not serve as proof.
Formally, therefore, there is an operator DIFFERENTIALDIAGNOSIS that maps a given finding B to the corresponding differential diagnosis DIFFERENTIALDIAGNOSIS(B). An operator is a mapping, and therefore each result of DIFFERENTIALDIAGNOSIS is unique for any given finding B. If the operator DIFFERENTIAL DIAGNOSIS(DIFFERENTIALDIAGNOSIS(B)), which represents the exclusion procedure, is applied to the differential diagnosis DIFFERENTIALDIAGNOSIS(B), the result is the „residual set“, which can be represented by the „WITHOUT“ operator of set theory: EXCLUDEDDIAGNOSIS(DIFFERENTIALDIAGNOSIS(B)) = DIFFERENTIALDIAGNOSIS(B) WITHOUT {E1, E2, E3,…}, if the Ei are the excluded entities.
If the exclusion diagnoses are to be unique in general, they must therefore be sufficiently broad so that the cardinality of DIFFERENTIALDIAGNOSE(B) WITHOUT {E1, E2, E3,…} is always less than or equal to 1.
Exhalation
see movement physiology – circulation/exspiration.
Exostosis
see movement physiology – bone/exostosis.
Exspiration
see movement physiology – circulation/exspiration.
Expiratory auxiliary respiratory muscles
see movement physiology – circulation/expiratory auxiliary respiratory muscles.
Expiratory respiratory muscles
see movement physiology – circulation/expiratory respiratory muscles.
Expiratory reserve volume
see movement physiology – circulation/expiratory reserve volume.
Extension (elbow joint)
Extension in the elbow joint, i.e. increasing the (internal) angle between the upper arm and forearm to 180° and possibly beyond (hyperextension).
Extension (finger joint)
With the exception of the thumb, in addition to the metacarpophalangeal joint (MCP), there are 2 joints per finger, a proximal joint (closer to the wrist: proximal interphalangeal joint, PIP) and a distal joint (further away from the wrist: distal interphalangeal joint, DIP). In both, extension (stretching) in the sense of increasing the palmar (internal) angle is possible up to 180° and possibly beyond (hyperextension). Hyperextension of all finger joints is physiological to a small extent, somewhat more in the metacarpophalangeal joint than in PIP and DIP. However, if a metacarpophalangeal joint of a little finger can be hyperextended by at least 90°, a point is awarded in the Bighton score for hypermobility.
Extension (cervical spine)
Tilting the head backwards towards the back, i.e. „craning the neck“. The extension of the cervical spine is also often referred to as reclination.
Extension (hip joint)
Reduction of the dorsal (back of the body) angle of the thigh to the pelvis, the opposite of „hip flexion„, i.e. a dorsal movement of the thigh in the sagittal plane.
Extension (knee joint)
Reduction of the patella-side (extensor side) angle in the knee joint, i.e. enlargement of the back-of-knee (popliteal) angle in the knee joint up to 180° and possibly beyond (overstretching).
Extension (spine)
Movement that occurs in parts of the spine or the entire spine as a result of the vertebrae tilting backwards in the sagittal plane over several vertebral segments, i.e. the spinous processes move closer together. Extension is possible to a much lesser extent in the thoracic spine than in the cervical and lumbar spine. This is partly due to the plane of movement of the respective facet joints.
Extension deficit
see movement physiology – extension deficit.
Extensors (knee joint, „knee extensors“)
The only extensor of the knee joint is the quadriceps. There are no synergists in either the thigh or the lower leg (in contrast to flexion of the knee joint, where there is the gastrocnemius for supporting flexion).
external reflex
see movement physiology – nervous system/external reflex.
External rotation / outward rotation (arm)
Turning out the arm in the shoulder joint: in neutral zero moving the biceps and inner elbow forward. See under external rotation for more information. When clapping, for example in concerts or theater, the lunging movement is an external rotation of the arm.
External rotation / outward rotation (leg)
Rotation of the thigh in the hip joint, for more information see just below.
External rotation / outward rotation (hip joint)
Rotation of the thigh that results from the fact that (in relation to standard anatomical position) the inner knee is moved more forwards and the outer knee more backwards. The degree of exorotation capability in the hip joint depends on the movement of the leg in the sagittal plane, i.e. flexion / extension, although much less so than in the case of the dependence of abduction capability on the rotation situation. The capability to turn out (externally rotate) in the hip joint is generally much more pronounced than the capability to turn in. For reasons, see internal rotation in the hip joint.
External rotation / outward rotation (knee joint)
The knee joint allows the lower leg to rotate in relation to the thigh when the knee joint is not extended. When it is, the tension of the collateral ligaments prevents this movement. If it is still possible, this is an indication of collateral ligament damage. External rotation is performed by the only muscle of the outer hamstrings, the biceps femoris. The counter-movement is the internal rotation in the knee joint performed by the inner hamstrings. As a rule, external rotation is somewhat more powerful and possible to a somewhat greater extent than internal rotation.
External rotation / outward rotation (shoulder joint)
Rotation of the humerus in the glenohumeral joint, which is described in standard anatomical position by the fact that the medial elbow rotates forward, i.e. the olecranon rotates medially.
External rotators / outward rotators (shoulder joint)
the muscles that perform the external rotation (outward rotation) in the shoulder joint: infraspinatus, teres minor, deltoideus (with its pars spinalis).
External rotation / outward rotation (shoulder blade)
see outward rotation of the shoulder blade
External rotators / outward rotators (shoulder blade)
see outward rotators of the shoulder blade
External torque
Torque acting on a joint from the outside (not from the body), which acts in the direction of flexion or extension of the joint or as torque in the direction of rotation.
Extremum
Extremum is the mathematical term for the fact that a function (with not necessarily only a one-dimensional range of values) is smaller everywhere in an environment than at the extreme point (maximum) or is greater everywhere (minimum). The algorithms that describe the yoga poses contain many extremal tasks of the type „stretch the arm with shoulder blade maximally towards the ceiling“, as it is said in urdhva hastasana, for example, or „tilt the pelvis maximally into flexion„, as it is said in uttanasana. As explained in the introduction, many extremes are linked to side conditions that must be fulfilled exactly. For example, the maximum hip flexion in uttanasana requires that the knee joint has a 180° angle, i.e. is anatomically in 0° flexion, as the angle in the knee joint has a serious influence on the capability to flex in the hip joint since the hamstrings are biarticular and span both.
Extrinsic
Term for muscles that move the digits of the fingers or toes,
but do not originate in the hand or foot, but in the forearm or lower leg.
F
Fascia
see movement physiology – fasciae.
Fibrosis
Fibrosis is a pathological proliferation of connective tissue, i.e. collagen fibers and connective tissue cells in tissues. Fibrosis always leads to a reduced elasticity of the tissue and later possibly to organ insufficiencies. Most known fibroses are secondary.
Fibrotization
Fibrosis is the transformation of organ parenchyma (functional tissue) into connective tissue.
Fibularis group
The fibularis group is a group of pronators of the ankle located in the lateral lower leg (movement takes place in the subtalar joint and subordinately in distal joint lines such as the Chopart or Lisfranc joint line). Fibularis longus, fibularis brevis and fibularis tertius are present in almost all people. A fibularis parvus is considered a variety in which this group is rich. The varieties are differentiated according to their origin because they generally have the same attachment. Most of the origins of the varieties lie distal to the origin of the fibularis longus.
Finger extensors (finger extensors)
Group of muscles that extend the fingers in the metacarpophalangeal (MCP), proximal (PIP) or distal (DIP) interphalangeal joint:
- M. extensor digitorum: common extrinsic finger extensor, located in the forearm
- Mm. lumbricales (hand): intrinsic flexor, flexes in the metacarpophalangeal joints (MCP), but extends in the proximal (PIP) and distal (DIP) joints; helpful for fine grasping, writing
- M. extensor indicis: extrinsic index finger extensor, one of the few extrinsic extensors not originating from the lateral epicondyle
Finger flexors
Group of muscles that flex the fingers in the metacarpophalangeal (MCP), proximal (PIP) or distal (DIP) interphalangeal joint. This group consists of:
- M. flexor digitorum profundus (extrinsic): flexes the distal joints (DIP) of fingers 2-5, their proximal joints (PIP), the metacarpophalangeal joint (MCP) and the wrist.
- M. flexor digitorum superficialis (extrinsic): flexes proximal joints (DIP) of fingers 2-5, their proximal joints (PIP) and metacarpophalangeal joints (MCP), the wrist and (with very little force) the elbow joint.
- Mm. lumbricales (intrinsic): flex in the metacarpophalangeal joints and extend in the proximal (PIP) and distal (DIP) joints; helpful for fine grasping, writing
- in the case of the little finger: M. flexor digiti minimi brevis (hand): flexes the proximal joint (PIP)
firm-elastic
see movement physiology – joint/firm elastic.
Fitness
see movement physiology – fitness.
flexibility
see movement physiology – joint/flexibility.
Flexion (elbow joint)
Flexion in the elbow joint, i.e. reduction of the (internal, on the biceps-side) angle between the upper arm and forearm to approx. 30°. While the extension limited is hard-elastic, flexion is usually limited firm-elastic and only rarely soft-elastic. The muscles responsible for flexing the elbow joint are the arm flexors.
Flexion (finger joint)
With the exception of the thumb, there are 2 joints per finger in addition to the metacarpophalangeal joint, a proximal interphalangeal joint (closer to the body, PIP) and a distal interphalangeal joint joint (further away from the body, DIP). Flexion (bending) in the sense of reducing the palmar (internal) angle to possibly 90° is possible in both.
Flexion (hip joint)
Reduction of the frontal (anterior) angle of the thigh to the pelvis, a movement in the sagittal plane. The term „anteversion“ in the hip joint is sometimes used as a synonym. Flexion is performed by the hip flexors, with the hip extensors acting antagonistically.
Flexion (knee joint)
Enlargement of the patella-side (extensor side) angle in the knee joint, i.e. reduction of the popliteal angle in the knee joint. The muscles involved are the knee flexors, i.e. the hamstrings plus the gastrocnemius, the gracilis and the sartorius.
Flexion (neck)
Tilting of the head forward towards the chest, sometimes also referred to as inclination. This is nothing other than the flexion of the cervical spine. The opposite movement is reclination.
Flexion of the spine
Forward flexion of the spine, i.e. reduction of the ventral angle of the vertebral bodies in the sagittal plane. Flexion of the spine in the thoracic and lumbar spine is mainly caused by the straight and oblique abdominal muscles. The opposite movement is the extension of the spine, which is mainly caused by the autochthonous back muscles.
Flexion deficit
Analogous to the extension deficit, whereby the boundary between presence and absence is usually less clearly defined. While the 180° angle is a clear and both geometrically and physiologically plausible limit and nonattainment defines an extension deficit, the case of a flexion deficit is much less simple. After all, many people have more or less pronounced flexibility restrictions not only in the monoarticular muscles that cover their joints, but also in the biarticular and polyarticular muscles, which become relevant depending on the position of the neighboring joints. In addition, in the case of the hip joint, knee joint and elbow joint, extension corresponds to the standard anatomical position and is also frequently taken at least in approximation, e.g. when standing and variably also when walking and in standing handling. The movement-physiological plausibility of the 180° also arises from the fact that in the corresponding joint in the vertical position of the articulation partner, no flexion moment results in the joint from the overlying partial body weight, which in the case of the joints mentioned is likely to be closely causally linked to upright gait.
In the case of a flexion deficit, a limit must be set more or less arbitrarily. If flexion is to be performed actively, often the performing muscles become passive insufficient, which means they cannot flex the joint any further because the antagonists are not flexible enough, so that from a certain point of flexion, their extension moment, which increases with each degree of angle, can no longer be overcome by the agonists, especially as in many cases monoarticular agonist muscles can exert increasingly less force on the descent of the force-length function towards the minimum sarcomere length and thus, in this case, cause increasingly less flexion moment. At a certain point, the agonists then work at such a short sarcomere length that they become actively insufficient and typically begin to cramp. External force can then be applied in an attempt to flex the joint, which should at least prevent the (actively insufficient) agonists from cramping.
If a flexion deficit is suspected, both the actively and passively achievable flexion must therefore be assessed, whereby the latter should in many cases lead to an increasing sensation of stretching in the antagonists with increasing force exerted. For a correct assessment, a possible influence of biarticular and polyarticular antagonists must be excluded in both cases.
Flexors (knee joint, „knee flexors“)
Most of the flexors of the knee joint are located in the back of the thigh: the entire hamstrings, with the exception of the monoarticular caput breve of the biceps femoris, flexes the knee joint (i.e. the muscles semimembranosus, semitendinosus and biceps femoris caput longum), as well as the gracilis , located in the inner thigh and sartorius muscle in the ventral thigh. The tensor fasciae latae also has a flexing effect in the knee joint via the IT band when the knee joint is bent at an angle of more than 30°. Other flexors of the knee joint are the lower leg muscles gastrocnemius and (weakly also) plantaris as well as (very week) the popliteus located in the knee pit, whose main task is to reverse the final rotation, which is why its fibers run transversely rather than longitudinally.
Force
Force is the physical term for a directed effect on a body that can change its direction or position, deform it or cause other changes. Since forces are directed and their strength is a scalar quantity, they can be easily represented as vectors. The direction of the vector is then the direction of the force and the length of the vector, i.e. the mathematical norm, is the strength of the force. Forces can be added vectorially. Opposing forces of equal strength cancel each other out. In a general sense, force refers to the ability to cause something. If a force is exerted along a certain path, this is work. A simple example of this is lifting an object. In order to hold it against gravity, a certain force is required, such as spring tension. This force is opposed to its gravitational force and is equal in magnitude. If the object is now lifted by one meter by exerting more force on it than is required to simply hold it, work is done and the lifted object has a higher potential energy than before. The work performed is therefore equivalent to the increment in energy. If the body is not lifted but heated, it also contains more energy, in this case thermal energy. The concept of work must therefore be generalized so that heating can also be understood as work. This also explains the maintenance of body temperature against the constant loss of heat to the environment. The muscle performs work and consumes energy, the greater the heat dissipation (e.g. at low ambient temperature and insufficient clothing or in the body’s „cooling mode“ during and after greater physical exertion), the more.
In terms of yoga poses, there are many different forces at work, first and foremost the gravitational force exerted by a partial body weight (correct, which acts on a partial body weight) and the tendon force of the muscles, which hold a joint in position or induce movement. However, a muscle functions very differently from a spring balance, a bar or a support, which could be used to prevent gravity-induced movement. According to its construction and control, the muscle is subject to a constant alternation of muscle fibers, which together apply a certain amount of tendon force over time. Therefore, the application of a certain amount of tendon force consumes a certain amount of (chemical) energy over a period of time. If the tendon force required by the muscle is above a certain threshold for a certain period of time, this exceeds the supply or disposal capacity and the muscle begins to tire and burn as a result. The factors of time and tendon force are in relation to each other. It is therefore clear that, in contrast to locked objects, holding an asana costs energy, the greater the forces to be exerted, the more. The energy required comes directly from the reaction of ATP to ADP, i.e. ultimately from food. Another example of energy consumption without any externally visible work being performed is the simultaneous and equally intense tensing of the elbow flexors and elbow extensors, so that no movement results in the elbow joint. In order to achieve and maintain the desired tendon force, other muscle fibers must constantly be brought into action to perform their share of the „holding work“ and consume energy in the process.
Force-length function (often: „force-length relation“)
see movement physiology – muscle/force-length-function.
Force-velocity-function (Force-velocity-relationsship)
see movement physiology – muscle/force-velocity-function.
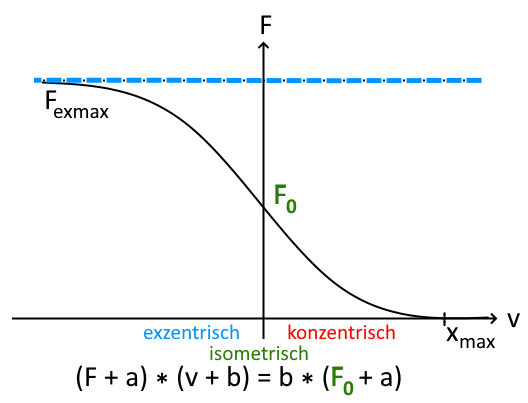
with v as the contraction speed, F as the muscle force, F0 as the isometric maximum force and empirical constants a,b.
In simple terms, this means that the faster a muscle contracts, the lower its force and the slower the eccentric movement, the greater the force.
Force arm
In terms of biomechanics, this is the lever arm, i.e. the length of the lever on which a force moves a load around a center of rotation.
Forefoot running
Running style usually used at fast speeds and shorter distances. The landing point is just before the body’s center of gravity. The flexion angle in the knee joint is a maximum of 10°, the angle in the ankle is over 90°. Forefoot running requires running shoes with a low drop (the height difference of the heel minus the height of the ball of the foot), a stable longitudinal arch and good muscular equipment. Barefoot rearfoot runners also quickly switch to forefoot running. When switching from other running techniques to forefoot running, adaptation difficulties can occur with corresponding symptoms, apart from sore muscles, this is mainly achillodynia. The wear pattern of the shoes shows the greatest abrasion in the area of the 5th toe. The advantages of forefoot running include better energy efficiency, reduced ground contact time, less need to cushion the landing, better shock absorption by the longitudinal arch of the foot, tendons and muscles of the lower leg, reduced overpronation. Disadvantages are high demands on the muscles and their tendons and a great tendency to overstrain them, especially for forefoot running beginners. Footwear requirements: flat, flexible, low drop, no pronation support, sufficiently flexible and yet stable in the toe area. Greater tendency to Achillodynia, PFPS, metatarsalgia and weakening of the hamstrings. Contraindications for forefoot running are: Hallux valgus, hallux ridigus, kinked foot, flat foot, splayfoot, achillodynia, PFPS, tendency to calf problems.
Fracture healing
see movement physiology – bone/fracture healing.
Free leg / playing leg
The leg not connected to the ground (the one connected to the ground is the standing leg) but performing a posture or movement, see the definition of standing leg.
Frontal abductors of the (shoulder joint)
The muscles that perform frontal abduction (also known as anteversion) in the shoulder joint: deltoid, coracobrachialis, biceps and, under certain conditions (mainly only low degree of present frontal abduction), parts of the pectoralis major.
Frontal adductors of the (shoulder joint)
the muscles that perform frontal adduction in the shoulder joint, i.e: Teres major, latissimus dorsi, triceps (only caput longum), deltoid (pars spinalis, pars acromialis partially) and under certain conditions (mainly low degree of present frontal abduction) pectoralis major.
Frontal
denotes a direction and means „in front of or towards the front“ and is identical to the term anterior or ventral. The conceptual opposite is dorsal, which in turn corresponds to the term posterior.
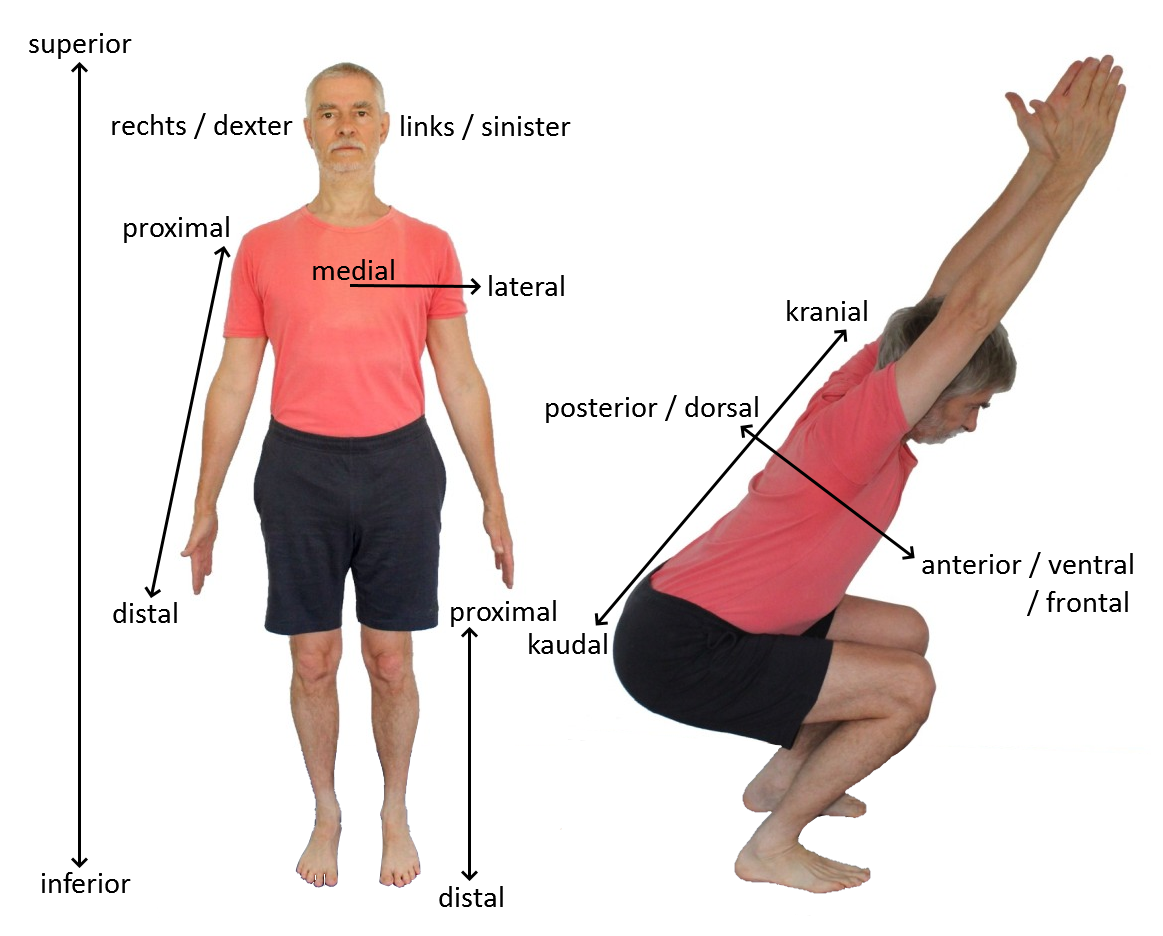
Frontal plane
a vertical plane running from left to right through the person in standard anatomical position, i.e. it runs parallel to the plane through the left and malleoli as well as through the left and right acromion.
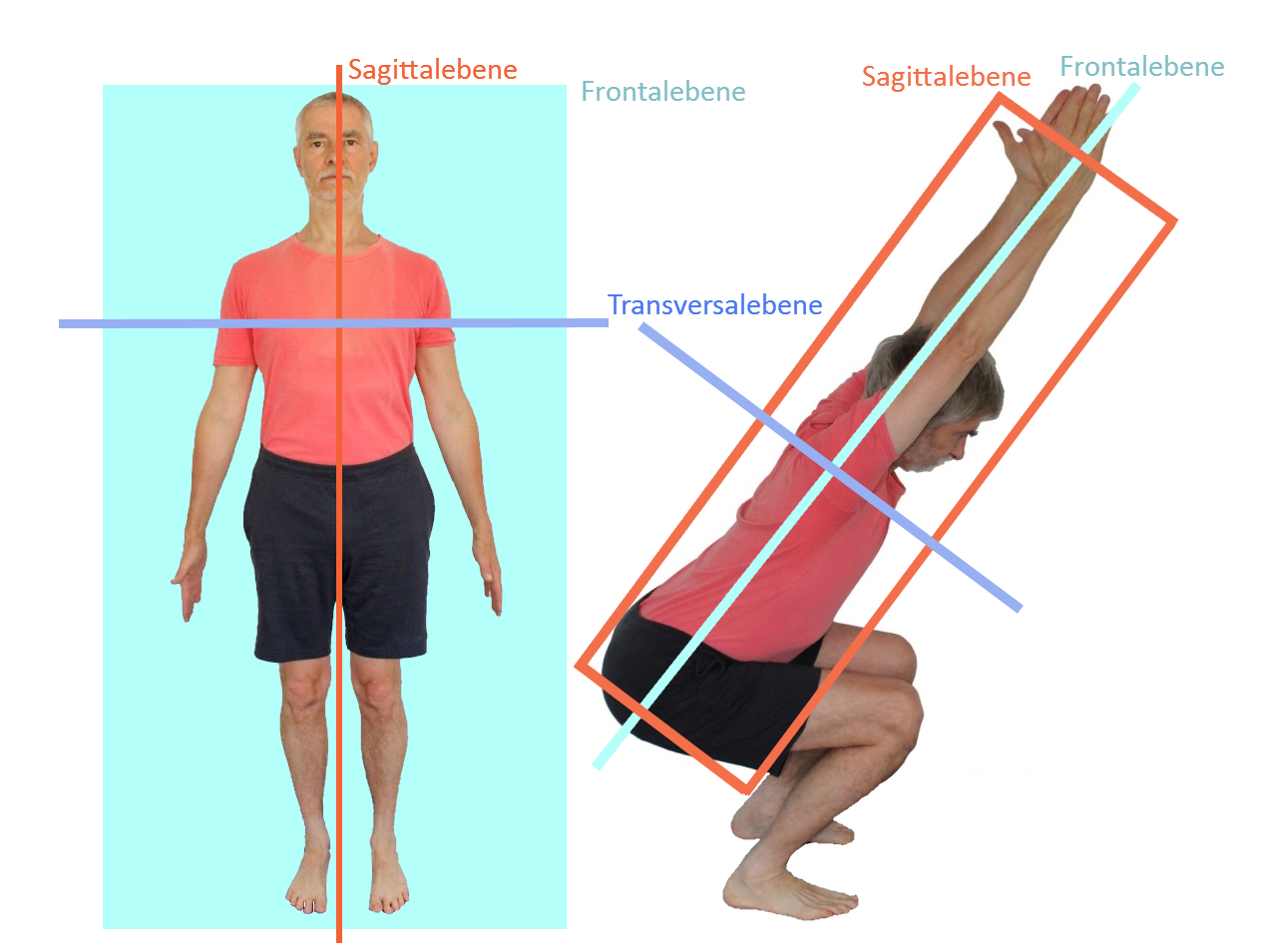
Function test
functional pain
see movement physiology – nervous system/functional pain.
Functional test
Foot deformity
Congenital or acquired malalignment of foot bones: Clubfoot, flatfoot, kinked foot, splayfoot, pointed foot, hollow foot, sickle foot, fallen arches. Foot deformities can be reducible or contractured. If contractural deformities are more pronounced, surgical intervention is usually necessary to prevent consequential damage to other parts of the the musculoskeletal system.
G
GCS Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is a system for assessing consciousness disorders and brain dysfunction, which evaluates the following three areas:
- Opening the eyes (1-4 points)
- Best verbal response (1-5 points)
- Best motor response (1-6 points)
This means that the results range from a minimum of 3 points to a maximum of 15 points. Results below 14 are classified as pathological and require action to be taken:
| 12 – 13 points | mild disturbance of consciousness | monitoring |
| 9 -11 points | moderate Bewusstseinsstörung | readiness for intubation |
| 3 – 8 points | heavy disturbance of consciousness, coma | Protective intubation due to lack of protective reflexes |
Recent traumatic brain injuries are classified according to GCS as
- 3-8 points: heavy
- 9-12 points: moderate
- 13-15 points: mild
For children aged 3 years and older, the statements are worded slightly differently whereas the GCS is not applicable for children under 3 years of age.
See also:
https://flexikon.doccheck.com
GIRD (Glenohumeral Internal Rotational Deficit / Glenohumeral Endorotation Deficit)
GIRD (Glenohumeral Internal Rotational Deficit) is a glenohumeral internal rotational deficit that is usually not due to shortened external rotators of the shoulder joint but to a thickening and hardening of the dorsal/dorsoinferior joint capsule that has developed in response to certain activities such as throwing. Dorsal hardening pushes the humeral head ventrally, while dorsoinferior hardening can push the humeral head dorsosuperiorly. Dorsal hardening in particular tends to stretch the anterior capsule. In addition to competitive gymnastics, overhead throwing sports are particularly affected. GIRD often occurs in throwers, with the first changes to the dorsal joint capsule occurring after 40 – 60 throws already. It often lead to or is part of a thrower’s shoulder.
It is assumed that the GIRD must be regarded as an early indicator of shoulder problems requiring treatment. The result is a picture of glenohumeral instability, an internal impingement tendency and a predisposition to damage to the glenoid labrum such as the SLAP lesion, often leading to the end of the patient’s career. GIRD is diagnosed when there is a deficit of 20° to the contralateral side.
Ginglymoid joint / hinge joint
see movement physiology – joint types/hinge joint.
Giving way phenomenon
Inadequate yielding under load, usually of weight-bearing joints such as the knee joint. In the knee joint, cruciate ligament ruptures and other injuries are common causes of a Givingway phenomenon. Pain phenomena associated with arthritis or patella misalignments, as well as muscular deficits or neuromuscular disorders, may also be considered as causes. Orthoses and strengthening training, possibly also coordination and proprioception training, can help conservatively; ligament ruptures can be treated surgically. For the giving way of the knee joint, see the Jakob giving way test
Glutes
the three gluteal muscles: gluteus maximus, gluteus medius, gluteus minimus.
Gravity perpendicular
The gravity perpendicular is the projection of the center of gravity of a body onto the supporting surface along the direction of gravity. The supporting surface does not necessarily have to be horizontal. If a pose or an arrangement of physical bodies is to be statically stable, the center of gravity must lie in the physical support base. The closer the gravity perpendicular is to the edge of the support base, the less stable the configuration or pose will be. Likewise, the higher the center of gravity is above the supporting surface, more precisely: the greater the distance between the center of gravity and the gravity perpendicular (i.e. the difference in height between the two points), the less stable the pose will be. In both cases, the loss of stability results from the decrease in the tilting moment, i.e. the moment that must be applied to cause the body to tilt, as the lever arm becomes longer with increasing height of the center of gravity and therefore the force required to tilt the body decreases.
Gravity (gravitational force)
For the purposes of our considerations, gravity can simply be equated the gravitational force or mass attraction. The gravitational force is one of the four basic forces of matter. It causes masses to attract each other. It increases linearly with mass and decreases quadratically with distance. Unlike electric and magnetic forces, gravity cannot be shielded and is not influenced by the density of the environment (e.g. a vacuum). On earth, the center of the earth is considered to be the center of gravity, apart from the fact that earth’s surface is anything but round or uniform on closer inspection, as differences in density and height play a role. Gravity is very important for the asanas and their transitions. For example, the gravity perpendicular must lie in the physical base of support if a pose is to be statically stable. In order to maintain most posts (poses such as savasana and viparita karani are exceptions), muscles must work against the gravitational effect of certain partial body weights. This means that some poses cannot be held for any length of time because the muscles cannot provide any amount of strength endurance, examples include urdhva dhanurasana, staff pose or warrior 2 pose. For many transitions in which the physical support base changes, e.g. changing from two to four supporting limbs or vice versa from four to two, gravity implies that these transitions cannot be performed arbitrarily slowly, as the effect of gravity over time will end the transition in between with a different result than the intended one. Examples of this are the jump from downface dog to uttanasana and back or from uttanasana into staff pose as well as the jumping side change in the hip opener 1. Gravity is also important in inversion poses such as headstand, in which blood shifts from the lower to the upper regions of the body, leading to a perceived (and actual) fullness of blood in the head, for example. Further, gravity is important for flexing moments in joints such as the knee joint in virasana or warrior 2 pose.
Gravitational effect
The effect that gravity has on a movement. Although the gravitational force of a partial body weight or a dumbbell is always the same regardless of its position in space and in relation to the human body, the effects that it produces, i.e. the torques generated in joints, and therefore the contraction forces (tendon forces) to be applied by the muscles, vary between zero and a maximum, depending on the angle to the direction of gravity: at an angle of 90° we see the full effect, i.e. the maximum torque, is achieved, at 0° the torque is zero. The effect becomes clear in exercises such as lateral raises and front raises, which are completely light at the start of the movement and become increasingly heavy with increasing abduction towards 90° despite the increase in muscle strength according to the force-length function and the increased lever arm of the deltoid.
Groin pain
see movement physiology – nervous system/groin pain.
Growing pains
see movement physiology – nervous system/growing pains.
Gyroscopic force
The gyroscopic force, or more precisely the gyroscopic effect, is the inertia of an axis of rotation against changes. A symmetrical gyroscope or a rolling wheel stabilizes itself, which is well known to cyclists as the tendency to tip over decreases with speed (all other things being equal). The gyroscopic effect helps to prevent sideways instability in movements such as the one-legged handstand upswing if the swing is performed fast enough.
H
habitual
Constant, repetitive, habitual behavior. This refers, for example, to postural habits such as a hunched back when working at a computer or constantly raised (partially elevated) shoulder blades. Habitual factors can influence and impair the function of the musculoskeletal system and internal organs.
Hamstrings / ischiocrural muscles
see movement physiology – hamstrings.
hard-elastic
see movement physiology – joint/hard-elastic.
Heart
see movement physiology – circulation/Heart.
Heart rate
see movement physiology – circulation/heart rate.
Heart rate recovery HRR / Recovery pulse
see movement physiology – circulation/heart rate recovery.
Heart rate variability / HRV
see movement physiology – HRV.
Heel drop
Drop is the height difference between the heel and the ball of the foot. A high heel drop therefore corresponds to a higher „heel“. The drop of a shoe has an influence on the running style, the load distribution on the muscles and the strain on the musculoskeletal system. Basically, a higher drop results in a lower stroke of the Achilles tendon, a working range shifted towards a shorter sarcomere length and thus a lower utilization of the performance of the triceps surae. In addition, a greater drop hinders rolling the foot at longer stride lengths and higher speeds and would lead to side effects. On the other hand, a moderate drop may be indicated temporarily for achillodynia, but it is not a permanent solution or causal therapy.
Hindfoot
the two tarsal bones calcaneus and talus.
Hindfoot valgus
Disorder of the foot position with valgus position of the calcaneus and often also other tarsal bones. This disorder is usually based on a tibialis posterior dysfunction syndrome (posterior tibial tendon dysfunction, PTTD) and results in fallen arches or later flat feet. Once the disorder has manifested itself to this extent, a splayfoot often develops and even later a hallux valgus.
Hindfoot varus
Disorder of the foot position with varus position of the calcaneus and often also other tarsal bones. In contrast to disorders with valgus position of the calcaneus, this is significantly rarer and usually occurs with hollow foot or clubfoot.
Hinge joint / ginglymoid joint
see movement physiology – joint types/hinge joint.
Hip extensors (hip extensors)
Term for a group of muscles whose function (not necessarily exclusively) consists of extension in the hip joint, i.e. reducing the dorsal angle between the thigh and pelvis. This includes the three-part, mainly monoarticular buttock muscle with its maximus part (only this covers the SI joint with some fiber areas in addition to the hip joint), medius and minimus as well as the semitendinosus muscle, semimembranosus muscle and the biceps femoris with its caput longum (but not caput breve). The adductor magnus also belongs to this group with the fibres that come from the ischial tuberosity.
Antagonists: Hip flexors: iliopsoas, rectus femoris
Hip flexors
Term for a group of muscles whose function (not necessarily exclusively) consists of flexion in the hip joint, i.e. reducing the angle between the thigh and pelvis at the front of the body. In addition to the biarticular rectus femoris pars quadriceps, which also extends the knee joint, these are the monoarticular iliacus muscle, which only covers the hip joint, and the psoas major muscle, which also covers some vertebral joints and the SI joint. Any psoas minor that may be present is only seldom part of the hip flexors, as it usually attaches to the pubic bone instead of the thigh. Even if the adductors also have a slight hip flexor effect (in low degree of flexion of the hip joint only), they are usually not included. The tensor fasciae latae also has a hip flexing effect. However, the strongest hip flexors and therefore the most frequently mentioned are the iliopsoas, consisting of the psoas major and iliacus, and the rectus femoris, part of the quadriceps. The rectus femoris flexes in the hip joint and extends in the knee joint, whereby the movement in the hip joint requires more contraction per degree of flexion than the extension in the knee joint requires. This is due to the different distances of the muscle (in the case of the hip joint) or its tendon/patella (in the case of the knee joint) from the center of rotation in the joint, so wee see different lever arms.
To test the strength of the hip flexors, for example, you can actively lift your straight legs out of savasana, either individually or together. If this is easy and quick, the hip flexors should be strong enough for all everyday situations. If this is difficult or very slow, you can test how strongly a thigh in a supine position with 90° flexion in the hip joint (with the knee joint loosely bent so that the rectus femoris does not cramp) can be moved further towards the chest against external resistance. While the first test primarily tests the strength of the rectus femoris and, secondarily, the tensor fasciae latae, which also flexes the hip (as the distance between the parts of the iliopsoas or its tendon and the center of rotation in the hip joint, the center of the femoral head or the center of the ball of the acetabulum is still very small) the second test primarily tests these muscles, which have an excellent force arm at 90° flexion in the hip joint. If this test is conspicuous in the sense of a lack of exerted (objectively or subjectively assessed) strength, this indicates a lack of strength in the iliopsoas. Physiologically, the force that can be achieved by the iliopsoas at 90° flexion (or the corresponding torque in the hip joint, which is more difficult to measure) is significantly greater than the force to be expected in the first test. In some pathological cases, the test must also be performed in lateral comparison.
The flexibility test is somewhat more difficult. The hip flexor flexibility test provides an initial assessment. If it is successful, sufficient flexibility of the iliopsoas and, for all everyday cases, sufficient flexibility of the rectus femoris can be assumed. The hip flexor flexibility test measures the relevant hip flexors as a functional unit. The rectus femoris is usually the most restrictive, more than the hip flexors in the pelvis (the iliopsoas), as the knee joints are widely flexed. If the flexibility of the iliopsoas is to be assessed with the hip flexor flexibility test set-up, the flexion of the knee joints must be limited to aprox. 90°. The knee joints can then only be lifted passively from the floor by the supporter/examiner. Another test, although its specificity is not ideal, is the hip opener 1 . In this test, the pelvis is lowered as far as possible with the rear knee joint extended, which at a certain point may mean extension in the corresponding hip joint and provides a good indication of its ability to extend if – and this is a real prerequisite or limitation – the hip extensors of the front leg are sufficiently mobile not to hinder the lowering of the pelvis. In practice, there are certainly cases in which the gluteus maximus or the hamstrings of the front leg, for example, prevent further lowering of the pelvis, which becomes noticeable through clear and increasing stretching sensations in the corresponding muscles as the lowering progresses. Other poses to assess the flexibility of the iliopsoas include warrior 1 pose, back arch, purvottanasana, setu bandha sarvangasana and ustrasana. In the latter four poses, the knee joint is bent at 90° at best, so that the rectus femoris is generally not a limiting factor. In addition to the quadriceps stretch on the wall 2, the following orthopaedic tests are also suitable for assessing the flexibility of the rectus femoris:
Intensive use of the iliopsoas can lead to psoas syndrome (sometimes also referred to as leaning) as an overuse phenomenon. If a psoas minor is present and shortened, it can cause a psoas minor syndrome, i.e. depending on whether it is bilateral, a scoliosis or a hollow back.
Hollow back (lumbar spine hyperlordosis)
The spine has two physiological lordoses (concave curves when viewed dorsally, i.e. from the rear) and one physiological kyphosis (convex curve when viewed dorsally). All three curves must not fall below or exceed a certain level in standard anatomical position. A hollow back is generally defined as a lordosis of the lumbar spine that exceeds the physiological level and is often caused by muscular imbalances in the leg/pelvic region, primarily due to shortened hip flexors. In general, these often arise habitually (e.g. due to sitting too long and too often) as well as due to weak leg muscles in childhood/adolescence, but also due to repetitive activities or sports in which the hip flexors are used forcefully or very frequently and repeatedly. See also the article in the FAQ. For the possible effects of a hollow back, see the pathology page.
HSR (Heavy Slow Repetition, HSRT, Heavy Slow Restistance Training)
HSR is a strength training technique in which the repetitions are performed slowly in order to achieve good strengthening with minimal side effects. Good strengthening of the tendon tissue should also be achieved with sufficient weight/resistance. A minimum duration of three seconds is set for both the concentric contraction and the eccentric contraction. HSR has proven itself in the movement therapy of insertion tendopathies.
Hyperaesthesia
see movement physiology – nervous system/hyperaesthesia.
Hyperalgesia
see movement physiology – nervous system/hyperalgesia.
Hyperextension
see movement physiology – joint/hyperextension.
Hyperkyphosis
Hyperkyphosis is a kyphosis of the thoracic spine that is excessively pronounced in standard anatomical position compared to the physiological state. Rarely and with a clearly pathogenic value it also could occur in the lumbar spine or cervical spine. In the case of the thoracic spine, hyperkyphosis is also commonly referred to as a „hump“ or „hunch“.
Hyperlordosis
a lordosis of the lumbar spine or cervical spine that is excessively pronounced in standard anatomical position compared to the physiological state. In the case of the lumbar spine, it is also referred to as a hollow back.
Hypermobility
see movement physiology – joint/hypermobility.
Hypermobility syndrome
see pathology – hypermobility syndrome.
Hyperpathia
see movement physiology – nervous system/hyperpathia.
Hyperpronation / overpronation (foot)
excessive pronation when running / walking. It predisposes to some lower limb disorders, especially when the lower limb is used more intensively: DGS (piriformis syndrome), plantar fasciitis, Heel spur, Runners knee, Achillodynia (Achilles tendonitis), shin splints syndrome, (internal)meniscus damage, Pes-anserinus syndrome, but contrary to previous opinion not for PFPS (chondropathia/chondromalacia patellae).
Of the three phases of ground contact of a foot during walking or running (landing phase, support phase, push-off phase) is the middle phase and the support phase is the one in which overpronation, i.e. excessive lowering of the inner foot compared to the outer foot, is recognisable and comes into play. This results in excessive strain on the medial structures of the leg system. Around half of runners are affected by overpronation, women more than men. kinkfoot, lower foot, flat foot, obesity and fatigue can lead to overpronation, as well as weakness of the supinators or overcrossing when running. Special models of running shoes are available for overpronators. Beginners are more frequently affected.
Hypersupination
excessive supination during running and walking. Only 2-3% of runners are hypersupinators. This puts excessive strain on the lateral structures of the leg system and predisposes to supination trauma. There are generally no special models of running shoes available for supinators, partly because this group is very small, on the other hand, because with sufficient dorsal guidance of the foot by the shoe, the foot floats outwards and thus the supination trauma can be avoided. In addition, hypersupination can lead to (internal)peniscus damage. X-legs, hollow foot, Insufficiency of the foot and lower leg muscles and weak ligaments can predispose to oversupination.
Hypomochlion
A hypomochlion is a body structure, such as a part of a bone or a retinaculum, which increases the lever arm of a muscle or its tendon. These can be bone edges, bony protrusions, incisures or a sesamoid bone. A bony hypomochlion is, for example, the patella, the pisiform bone or the sesamoid bones of the hallux.
Hypothenar
The ball of the hand opposite the thumb on the side of the little finger with its musculature:
I
Immobilization
the therapeutic immobilization of an area of the body, for example after fractures or illnesses or for the purpose of transporting seriously injured people in order to prevent further damage that is difficult to foresee. This can be done using aids such as splints or casts or a stretcher with straps.
Impingement
Impingement refers to the pathological (and fundamentally pathogenic) contact of one structure, usually a bone, with another structure. Common impingements include those of the shoulder joint (known as subacromial impingement ) and the hip joint (known as femoroacataluar impingement FAI).
Incidence
Incidence refers to the number of new cases of a particular entity (or, in general, cases or events) in a particular population group over a particular period of time. For example, the number of new cases of herniated discs among office workers in one year. The incidence rate is then the corresponding proportion of the population.
Inferior
denotes a position close or (in comparison) closer to the feet. The conceptual opposite is superior. The term thus goes beyond the term caudal, which refers to a position close to the lower end of the trunk.
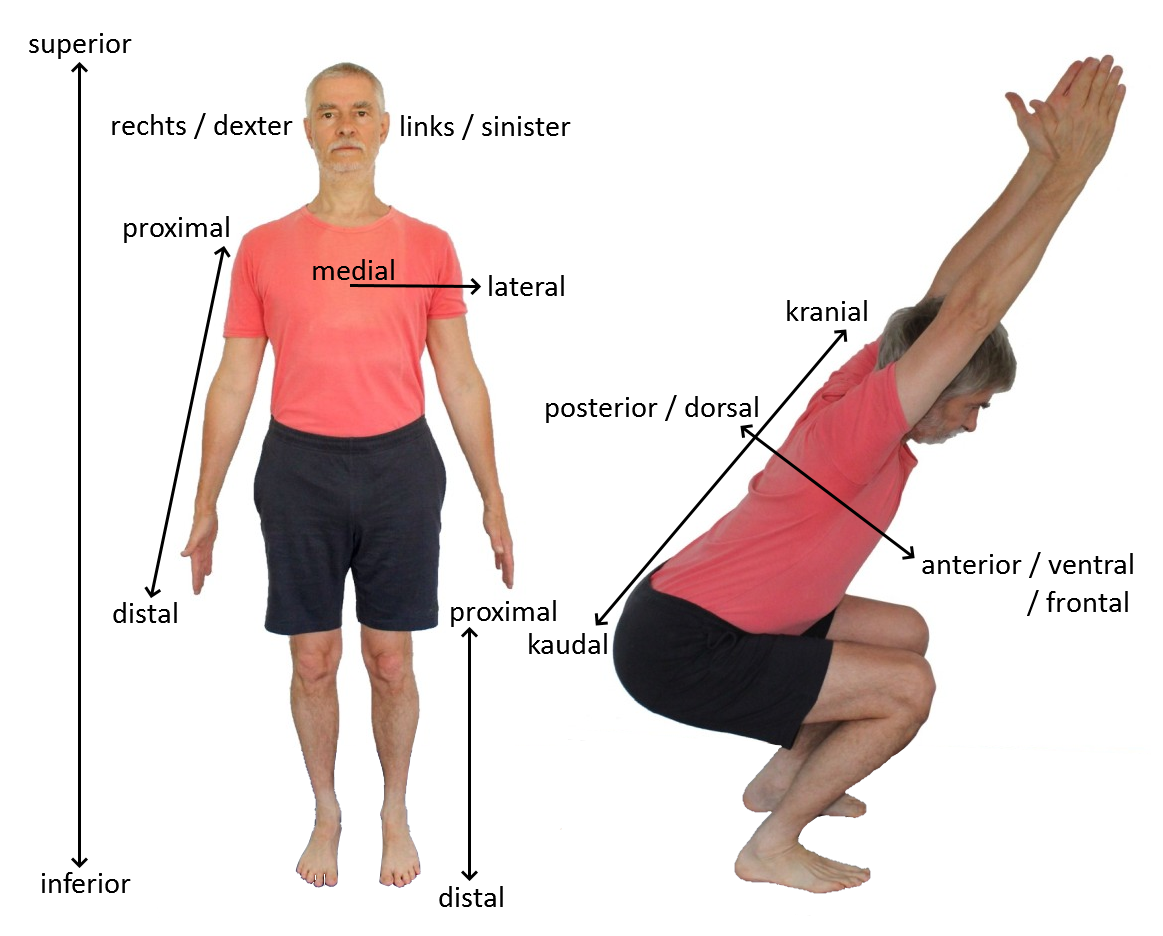
Inconstant
Some anatomical structures are present in all people; these are called constant. Those that are not regularly present are called inconstant. Examples include certain ligaments such as the medial transverse retinaculum of the knee joint or bursae, which only become pronounced when a structure is stressed.
Inflammation
The body’s own reaction to harmful stimuli. These stimuli can be
- Chemical (acids, alkalis, toxins, enzyme exposure as in pancreatitis)
- Physical (pressure, friction, trauma, foreign bodies, metabolic products such as uric acid crystals (e.g. in gout), heat, cold)
- Traumatic
- Germs (bacteria, viruses, fungi, parasites)
- Allergens
- Autoallergens (triggers of rheumatic and autoimmune diseases)
Inflammations not caused by pathogens are referred to as aseptic. Inflammation is a reaction of the body with which it attempts to restore the initial physiological state, which is why it is also referred to as an inflammatory reaction. For repair, the affected area must be supplied with more blood and the pores of the membranes must be widened by appropriate inflammatory mediators so that immune cells (leukocytes) can flow into the area. Terminologically, the suffix „-itis“ is added to the anatomical name of the inflamed anatomical structure. Not all inflammatory processes make sense from a medical perspective. There are also autoimmunological inflammatory processes in which the body damages healthy endogenous cells. This misbehavior is due to a malfunction of the immune system in which, for example, antibodies previously formed against a pathogen also act against the body’s own tissue as part of a cross-reaction. Inflammation can occur in organs, the surrounding connective tissue, blood vessels and lymph vessels. There are 5 typical signs of inflammation:
- Dolor (pain)
- Calor (overheating)
- Rubor (redness)
- Tumor (swelling) and
- Functio laesa (Functional limitation)
Depending on how pronounced or voluminous the inflamed tissue is and how deep it is in the body, some of these 5 signs may not be perceptible.
Signs of inflammation
There are 5 typical signs of inflammation:
- Dolor (pain)
- Calor (overheating)
- Rubor (redness)
- Tumor (swelling)
- Functio laesa (Functional limitation.)
Depending on how pronounced or voluminous the inflamed tissue is and how deep it lies in the body, some of these 5 signs may not be perceptible. Rubor and tumor are due to increased permeability (mediated by interleukin-1 and prostaglandin I2), which causes increased plasma and blood cells to enter the tissue. Dolor is caused by pain messengers such as prostaglandin E2, prostaglandin I2, bradykinin and other kinins as well as cytokines (tumor necrosis factor) and is intended to protect the affected area. Calor is caused by the increased metabolic activity mediated by cytokines such as interleukin-6 (via the production of prostaglandin E2). In some cases, irreparable cells are abandoned (apoptosis, programmed cell death) or parts of tissue necrotize so that new cells can replace them. Under unfavorable conditions, pathogens causing inflammation can escape the local immune system and spread through the bloodstream to afferent tissues (sepsis) or lead to inflammation in the lymphatic tract (lymphangitis). Therapeutically, it must be examined whether the inflammatory process should be influenced so that the symptoms are alleviated, or whether the body should carry out the repair undisturbed according to its own mechanisms, which may lead to faster healing.
inhibitory
see movement physiology – nervous system/inhibitory.
Incongruent / incongruence / incongruity
see movement physiology – joint/incongruent.
Incongruence osteoarthritis
see movement physiology – joint/incongruence osteoarthritis.
Inhalation
see movement physiology – circulation/inspiration.
Insertion
The area of a bone where a ligament or the tendon of a muscle is fixed. In the case of a muscle, the proximal insertion is called the origin and the distal insertion is called the attachment, without distinction we talk of insertion. Some muscles insert non-tendinously to a bone, such as the origin of the iliacus in the iliac fossa of the ilium.
Inspection
Inspiration
see movement physiology – circulation/inspiration.
Inspiratory auxiliary respiratory muscles
see movement physiology – circulation/inspiratory auxiliary respiratory muscles.
Inspiratory respiratory muscles
see movement physiology – circulation/inspiratory respiratory muscles.
Inspiratory reserve volume
see movement physiology – circulation/inspiratory reserve volume.
Instability
see movement physiology – joint/instability.
Intercostal muscles
see movement physiology – circulation/intercostal muscles.
Internal rotation / inward rotation (leg)
Turning the femur in in the hip joint, for more information see internal rotation (hip joint).
Internal rotation / inward rotation (hip joint)
Rotation of the thigh that results from the fact that (in relation to standard anatomical position) the inner knee is brought backwards and the outer knee forwards. The degree of possible internal rotation in the hip joint depends very little on the movement of the leg in the sagittal plane, i.e. on flexion/extension, quite unlike the possibility to abduct depends on the rotation situation, for example. The ability to turn the leg in in the hip joint is generally much less pronounced than the ability to turn it out.
This may be due to human movement behavior since time immemorial: internal rotation of a leg when walking or running leads to the legs bumping into each other even at a slight angle. In contrast, external rotation of the legs is already obligatory for a quick change of direction while running, but even more so for sitting postures such as the cross-legged position. A low center of gravity is advantageous for lifting an unstable object, so the knee joints are bent. If the object is very heavy, the center of gravity of the object should be close to the center of gravity of the body, which is not possible when the knee joints are bent forward, but only when the knee joints are bent to the side with the legs open. This is likely to have been another important factor in the history of mankind, which is why a capability to turn out the leg wide developed in the hip joints.
Internal rotation / inward rotation (knee joint)
Internal rotation of the lower leg in the flexed knee joint is performed by the muscles of the inner hamstrings: semimembranosus, semitendinosus, furthermore the gracilis, and additionally the sartorius, i.e. all muscles that attach to the pes anserinus. For the countermovement, see external rotation in the knee joint. In the extended state of the knee joint the collateral ligaments and the cruciate ligaments prevent any rotation.
Internal rotation / inward rotation (arm / shoulder)
Turning the arm in in the shoulder joint: in neutral zero moving the biceps and inner elbow backwards. For more information, see here.
Internal rotators (arm / shoulder)
the muscles that turn in the upper arm in the shoulder, i.e. in standard anatomical position the inner elbow is rotated medially. These are subscapularis, pectoralis major, deltoideus (pars clavicularis), teres major, biceps (caput longum), latissimus dorsi.
Interstitium
see movement physiology – circulation/interstitium.
intramuscular coordination
see movement physiology – nervous system/intramuscular coordination.
Inward rotation / internal rotation (shoulder blade)
Movement of the scapula in the plane in which it mainly expands, with the inferior angulus (lower tip) downwards-inwards, which reverses the outward rotation, that is, returns the scapula from the outward rotated position in which it is when the arm is raised far. These muscles rotate the scapula inwards.
Inward rotators / internal rotators (shoulder blade)
Muscles that perform the internal rotation of the shoulder blade:
- Latissimus dorsi (indirect)
- Levator scapulae
- Pectoralis minor
- Pectoralis major (indirect)
- Rhomboideus major
- Rhomboideus minor
Interspinal system
the muscles that run between the spinous processes of various vertebrae and belong to the medial tract of the autochthonous back muscles: Interspinalis (lumborum, thoracis, cervicis) and spinalis (thoracis, cervicis, capitis).
Intertransversal system
the muscles that run between the lateral transverse processes of different vertebrae and belong to the lateral tract of the autochthonous back muscles: intertransversarii lumborum (mediales and laterales), thoracis, cervicis (anteriores and posteriores), which, innervated unilaterally, flex the spine laterally and extend it when innervated on both sides.
Intervertebral disc (spinal disc, discus)
Elastic cartilaginous buffer between bones, which serves to improve pressure distribution and increases the contact surface of the cartilage coverings of the bones, thus reducing possible wear and tear. There are intervertebral discs between vertebral bodies, but also in classic joints such as the wrist and the acromioclavicular joint. Together with the articulating bones and the associated ligaments, the intervertebral discs are symphyses. The functional principle can be clearly seen in the example of the large intervertebral discs between the vertebral bodies: the nucleus pulposus is highly water-binding, so that the liquid part distributes the pressure as evenly as possible between the interfaces according to Pascal’s principle. This keeps the point pressure low and consequently the wear. See also the intervertebral disc between the vertebrae.
Intrinsic
Term for muscles that move the phalanges of the fingers or toes and originate in the hand or foot.
Inversion (foot)
Inversion is the sum of movements in the upper and lower ankle joint, consisting of supination, plantar flexion and adduction of the foot.
Ischaemia
see movement physiology – circulation/ischaemia.
Ischaemic pain
see movement physiology – circulation/ischaemic pain.
Isometric contraction
See movement physiology – muscle/isometric contraction.
Isometric muscle failure
see movement physiology – muscle/isometric muscle failure.
Isotonic contraction
See movement physiology – muscle/isotonic contraction.
J
Jogging
see movement physiology – jogging.
Joint
see movement physiology – joints.
Joint shapes
See movement physiology – joint shapes.
K
Kinetic chain
The term kinetic or kinematic chain originates from mechanical engineering and was coined at the end of the 19th century. It was first applied to the physiology of movement by Steindler, who differentiated between an open (OKC, open kinetic chain) and a closed (CKC, closed kinematic chain), but left room for interpretation by saying only that in the case of the CKC, the terminal link (e.g. an extremity) is restricted in its movement by a resistance. In a later definition by Grey, the terminal limb must be fixed. So if it moves the body weight, it is a CKC. Panariello only refers to the lower limb and therefore requires the feet to be fixed. The definition of the strictly and absolutely closed chain according to Steindler, in which the distal or proximal segment is fixed and the movement is polyarticular, is more practical.
Kinetic energy
The energy stored in the movement of a body. If the body is decelerated abruptly, this energy is converted into heat or cold deformation, for example. The speed is included as a quadratic factor in the energy of the body, while the mass is included as a linear factor. In order to accelerate a body, energy must be used, which is then contained in it as kinetic energy, i.e. one form of energy is converted into another.
Kinetic load
The term kinetic load, which is not commonly used in physics, is used here to describe a load that is caused by a moving body instead of a body at rest. The meniscus of the knee joint serves as an example. In anatomical zero, the load on each (left and right) of the two menisci of the knee joint is 42-45% of the body weight, or around 350 N per knee, depending on the literature used. During jogging or running, each leg is alternately unloaded as a free leg in the flight phase and then loaded again in the standing leg phase.
When the leg is lifted using the strength of the hip flexors at the start of the free leg phase, the meniscus and the cartilage of the tibia and femur is relieved by the inertia of the lower leg and foot so that at the beginning of the standing leg phase it is not only loaded again with the above-mentioned part of the body weight, but also with the mass inertia of the above
partial body weight (torso, head, arms) after the foot is placed on the ground.
The kinetic energy contained therein must be absorbed by the meniscus and the two cartilages of the tibia and femur. This hardly happens in the form of heat energy, but mainly in the form of elastic deformation of these cartilages. This phenomenon is intensified by the fact that the body’s centre of gravity oscillates in height, i.e. is at its highest approximately in the middle of the flight phase. Kinetic load refers to the effect that, in addition to the static load (weight force of the supported partial body weight), there is a kinetic energy that is dependent on the square of the speed, which leads to a significantly greater effect (e.g. elastic deformation or kinetic energy) beyond the effect of the static weight force (e.g. elastic deformation or non-elastic deformation such as cracks) on the supporting structures.
Knee lift
The extent to which the leg is lifted when running. Too little knee lift is usually the result of muscular weaknesses in the leg and hip flexor muscles. It predisposes to circumduction of the leg and various joint problems.
Kyphosis
Hunchback; the kyphosis can be physiological (kyphosis of the thoracic spine) or pathological (e.g. hyperkyphosis of the thoracic spine or kyphosis of the lumbar spine or cervival spine). More about this on the pathology page.
L
Labrum
A labrum is a cartilage lip. Such structures are particularly necessary where a very small, flat joint surface has to hold a bone with a large radius/circumference. Examples include the two large joints on the trunk with a large range of motion: the hip joint and the shoulder joint, where the shoulder joint requires a labrum much more urgently than the hip joint.
Lactate threshold
The lactate threshold is the maximum load at which the same amount of lactate can be removed as is produced. It represents the beginning of the anaerobic zone, which generally starts at 80% of maximum performance capacity. From this threshold onwards, an increasing oxygen debt and an increasing accumulation of lactate in the muscle are unavoidable.
Lever
Mechanical force transducer consisting of a rigid body that can be rotated around a fixed point (rotation center). A force applied to the body is converted into a rotary motion, whereby the applied force is converted into a torque.
Lever arm
The distance between the rotation center and the point at which the force of a lever is applied is referred to as the lever arm.
Leverage principle / law of the lever
For a lever in equilibrium, the sum of all applied torques (with respect to an identical reference point) is zero. In the case of a two-point lever, this is known as „force * force arm equals load * load arm in general“, where force arm or load arm are lever arms and mean the distance of the point where the force is applied or the load is moved resp. to the rotation center.
Limit of movement
see movement physiology – joint/limit of movement .
Load arm
In terms of biomechanics, this is the lever arm on which a load moves around a center of rotation, i.e. usually the distance of the object’s center of gravity from the center of rotation.
Lateral
denotes a position far or (in comparison) further away from the center, seen in the transverse plane. The conceptual opposite is
medial.
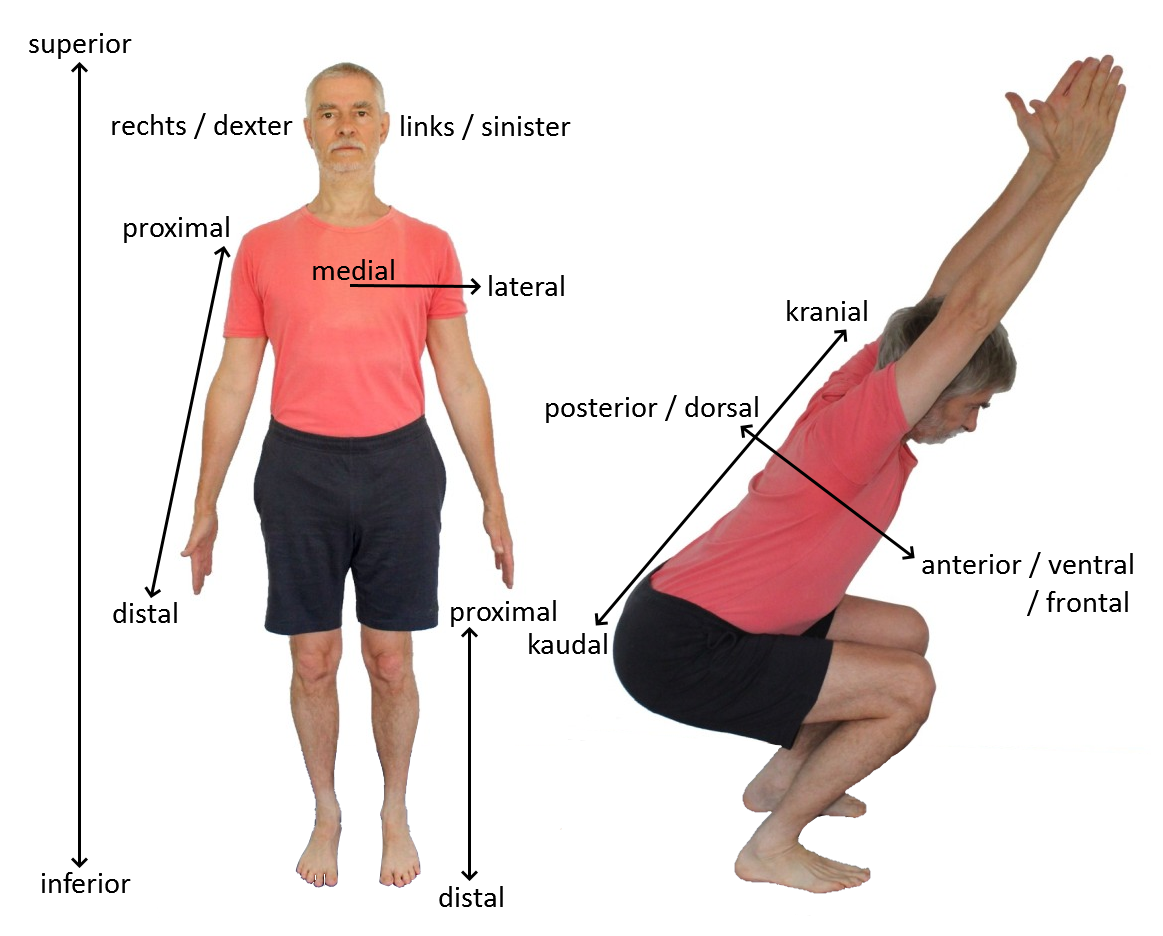
Lateral abductors of the (shoulder joint)
the muscles that perform lateral abduction in the shoulder joint: deltoid with all three heads, strongest with the pars acromialis, supraspinatus (even before the deltoid can build up a remarkable moment), biceps (weak with the caput longum).
Lateral adductors of the (shoulder joint)
the muscles that perform lateral adduction in the shoulder joint: triceps (caput longum only), teres minor, teres major, latissimus dorsi, deltoideus (partly with pars spinalis and pars clavicularis), pectoralis major.
Lateral tract
Part of the autochthonous back muscles: intertransversal system, spinotransversal system, sacrospinal system and the levatores costarum.
Lateral flexion
Lateral flexion of the spine. This is possible in all parts of the spine, depending on their different flexibility, i.e. it is least pronounced in the thoracic spine and most pronounced in the cervical spine. Depending on the area of the spine, various lateral flexor muscles cause lateral flexion of the spine; for a list, see lateral flexors.
Lateral flexors
The muscles that perform lateral flexion, i.e. lateral bending of the spine. These are
- General: oblique abdominal muscles, latissimus dorsi, quadratus lumborum, as well as the oblique system of the autochthonous back muscles: spinalis, semispinalis, longissimus, iliocostalis, multifidi, intertransversarii, interspinales.
- Specifically in the thoracic spine: Levatores costarum
- Specifically in the lumbar spine: psoas major, if present also psoas minor
- Specifically in the cervical spine: sternocleidomastoid, levator scapulae, scalenus anterior, scalenus posterior, scalenus medius, rectus capitis anterior, also autochthonous muscles: longus colli, splenius, obliquus capitis superior, rectus capitis posterior minor, rectus capitis lateralis
Lateralization (shoulder blade)
Maximum lateral movement of the shoulder blade, i.e. away from the spine without pulling it clearly forwards. This position is clearly far from retraction, but also far from protraction. It is usually most easily achieved when the arm is stretched outwards away from the spine at around 90° lateral abduction, as is the case in 2nd warrior pose or trikonasana. If the arm were moved from the position in which it is in the warrior 2 pose (90° lateral abduction) in the sense of a transverse adduction maximally forwards and later medially, the shoulder blade would begin to move into protraction at around 20° adduction if the flexibility is good. With less good flexibility, it may start earlier.
Lateralization is also possible in maximum frontal abduction, e.g. in caturkonasana, when the palms are pressed together forcefully. The difference between lateralization and protraction can easily be demonstrated experimentally if the arm is maximally adducted transversely from lateralization with the arm raised to 90° lateral abduction.
Lean Body Mass LBM / Fat Free Mass FFM
LBM refers to lean body mass, i.e. muscles or, in the case of myosteatosis, their lean portion, as well as bones, organs and all body components and fluids that are not fat. This means that LBM is always significantly higher than
LMM.
Lean Muscle Mass LMM
refers to the proportion of muscle in the body or its fat-free proportion in the case of myosteatosis. This means that LMM is always significantly smaller than LBM, as the latter also includes bones, organs, fluids and pathways.
Leg length discrepancy/inequality
see movement physiology – leg length discrepancy.
Lesser glutes
Collective term for the gluteus medius and gluteus minimus muscles, which are functionally supported by the gluteus maximus, a „large“ gluteus. Topologically, this covers the small glutes, which primarily abduct in the hip joint but also extend with the posterior fibres or flex with the anterior fibres. However, the small glutes do not have an turn out the femur.
Ligament
see movement physiology – joint/ligament.
Linea alba
The „white line“ between the two left and right parts of the rectus abdominis, i.e. the midline of the abdomen. It therefore lies in the median plane. Physiologically, it runs exactly vertically in standard anatomical position. Deviations from this need to be clarified. A curvature of the linea alba, for example, usually indicates scoliosis, while a deviation from the vertical in standard anatomical position indicates a difference in leg length. It is not uncommon for both to occur together, as leg length discrepancies tend to cause pelvic obliquity and, consequently, scoliosis.
Linea terminalis
The curve formed by the promontorium of the sacrum, pars lateralis of the sacrum, linea arcuata, eminentia iliopubica, pecten ossis pubis, tuberculum pubicum and symphysis, which separates the lesser pelvis cranially from the greater pelvis.
Lisfranc joint line
The Lisfranc joint line is the line connecting the joint surfaces of the bases of the metatarsal bones, that is, the line between the tarsus and the metatarsal bones, see under ankle joint: Lisfranc joint line.
LMN (Upper MotoNeuron)
see movement physiology – nervous system/LMN.
Load intensity
Load intensity is a variable that must be defined differently for different types of exercise. In the case of strength training, it is determined by the number of repetitions. In descending intensity, this is plotted against the number of repetitions as follows (Rühl, 1992):
- 100% – 1
- 95% – 2
- 90% – 3-4
- 85% – 5-6
- 80% – 7-8
- 75% – 9-10
- 70% – 11-13
- 65% – 14-16
- 60% – 17-20
- 55% – 21-24
100% is the load intensity that just allows a single repetition (in succession without regeneration time, the so called one repetition max.). If you are not working with repetitions of cyclical movements, but instead maintain isometric load over time, you must specify the minimum time interval to which 100% is assigned, which could be one second, for example. In general, the times until isometric muscle failure occurs are specified. When using external weights, a weighting depending on the weight is obvious. This does not necessarily have to be linear. All lower load intensities must then be assigned longer times, whereby the maximum time interval of an isometric load is likely to be quite individual, and in quite a few cases also dependent on other internal (e.g. tone of the antagonists) or external factors (e.g. temperature). In the case of stretching, the subjectively perceived intensity must be evaluated, for example using the usual Numerical Rating Scale (NRS), which is also used for the evaluation of pain or other symptoms, in which the numbers 0 (no intensity / sensation / discomfort at all) to 10 (strongest imaginable pain) are evaluated. Only two values are given a priori:
- 100% – 10
- 0% – 0
In addition, the assignment can be linear, logarithmic or otherwise non-linear. In addition to the load intensities mentioned, other constructs can also be defined, such as the load in watts (W) when cycling or the speed cycled or the running pace under specified conditions.
Load maximum
see movement physiology – load maximum.
Locomotor system / Musculoskeletal system
see movement physiology/locomotor system
Lombard phenomenon
Lombard’s phenomenon, which is sometimes incorrectly described as a
reversal of muscle function, occurs in the ischiocrural muscles, in that they appear to support the extension of the knee joint in a closed kinetic chain during walking or running, although they are definitely flexors of the knee joint. This results from the fact that they are also extensors of the hip joint and produce an effect there due to the larger lever arm in the hip joint, which supports the extension of the knee joint due to the closed kinetic chain with the foot as the punctum fixum, although they nonetheless generate a flexing moment in the knee joint, but this is outweighed by the movement of the thigh in the hip joint is outweighed .
Long bone / tubular bone
see movement physiology – bone/long bone.
longitudinal muscle adaptation
see movement physiology – muscle/longitudinal muscle adaptation.
Lordosis
convex from the front (ventral) or concave from the back of a part of the spine, physiologically this is the case to a certain extent in the lumbar spine and cervical spine.
LMN (Lower MotoNeuron)
see movement physiology – nervous system/LMN.
Lumbar spine
The lumbar spine is the part of the spine directly above the sacrum, usually consisting of 5 vertebrae, but lumbarization of sacral vertebrae or sacralization of lumbar vertebrae or even a supernumerary lumbar vertebra are not uncommon.
Due to its position above the sacrum, which is further ventral cranially, the lumbar spine physiologically curves in a concave lordosis (seen from behind). Permanent upright position or kyphoses of the lumbar spine are pathogenic. The lumbar spine is an important area of origin for an important hip flexor, the psoas major, which, when shortened, hyperlordoses the lumbar spine instead of (only) physiologically lordosing it. In contrast to the thoracic spine, the lumbar spine is free of rib attachments.
Lung
see movement physiology – circulation/lung.
Lymph
see movement physiology – cicrculation/lymph.
Lymph node
see movement physiology – circulation/Lymph node.
Lymphatic system / lymph system
see movement physiology – circulation/lymph system.
Lymph vessel / lymphatic vessel
see movement physiology – circulation/lymph vessel.
Lymphvalve / lymphatic valve
see movement physiology – circulation/lymph valve.
M
Malleolus fork
The „fork“ formed by the tibial and fibular malleolus, which surrounds the talus and thus the first tarsal bone.
Masking
It can sometimes be observed that typical effects of a pose do not occur because other statistically and physiologically less likely difficulties prevent them from appearing. Once these difficulties have been overcome, the typical effect then appears. This behavior is called masking of the statistically and physiologically expected phenomenon. Masking phenomena are often the result of the use of the musculoskeletal system in everyday life, work and sports behavior in terms of the activities performed and postures adopted.
Masking cascade
a sequence of masking effects, all of which mask a typically expected effect as well as each other. When the first masking effect is overcome, the second becomes visible, after its release the third, and so on. Once the entire masking cascade has been released, the typical, statistically and physiologically expected effect occurs.
(Mass) inertia
The ability of a rigid body in motion to continue this motion without automatic acceleration or deceleration (which is negative acceleration). If no external forces (such as air resistance or gravity) were acting on the body, it would continue to move in an infinitely linear fashion. As this law applies to both positive and negative acceleration, acceleration from rest is also covered. If it is a rotary motion, it is referred to as an inertia torque or moment of intertia.
Maximum heart rate / HFmax
There are various formulas for estimating the maximum heart rate depending on age and other factors:
- Spanaus (for athletes): 226 – 1.0 × age (women) or 223 – 0.9 × age (men)
- Tanaka (for athletes): 208 – 0.7 x age
- Hossack: 206 – 0.597 x age (women) or 227 – 1.067 x age (men)
- Edwards: 210 – 0.5 × age (in years) – 0.11 × body weight (women) or 214 – 0.5 × age – 0.11 × body weight (men)
The formulas are less accurate for athletes with decreasing age and more accurate with increasing age, even if very significant deviations are possible in individual cases. It is known that 60-year-old trained athletes max reach and tolerate 200 bpm. On the other hand, it is also known that older people who have been training at the cardiac performance limit for years can suddenly experience problems such as cardiac arrhythmias or heart failure (insufficiency).
In contrast to the calculation of the training zones, the resting heart rate is not relevant for determining the maximum heart rate, as far as is known. If the maximum heart rate is determined experimentally, the muscle mass used plays a major role.
In a study of cyclists and runners, three quarters of the 13 different prediction models underestimated the maximum heart rate by up to 5 beats, while some overestimated it by up to 5 beats. In general, the maximum heart rate does not appear to be strongly dependent on the level of training; well-trained people tend to have a lower HRmax. In the study, the HRmax of runners was 1% higher and the VO2max 3% higher than that of cyclists. According to another study, men generally have an almost 2% higher HRmax, an approximately 7% higher HR reserve and a half per cent better HR recovery, but the decrease in HRmax with age appears to be slightly lower in women.
Maximum strength
see movement physiology – muscle/maximum strength.
Maximum load
see movement physiology – maximum load.
Medial
refers to a position close to or (in comparison) closer to the center, i.e. seen laterally in the transverse plane. The conceptual opposite is lateral.
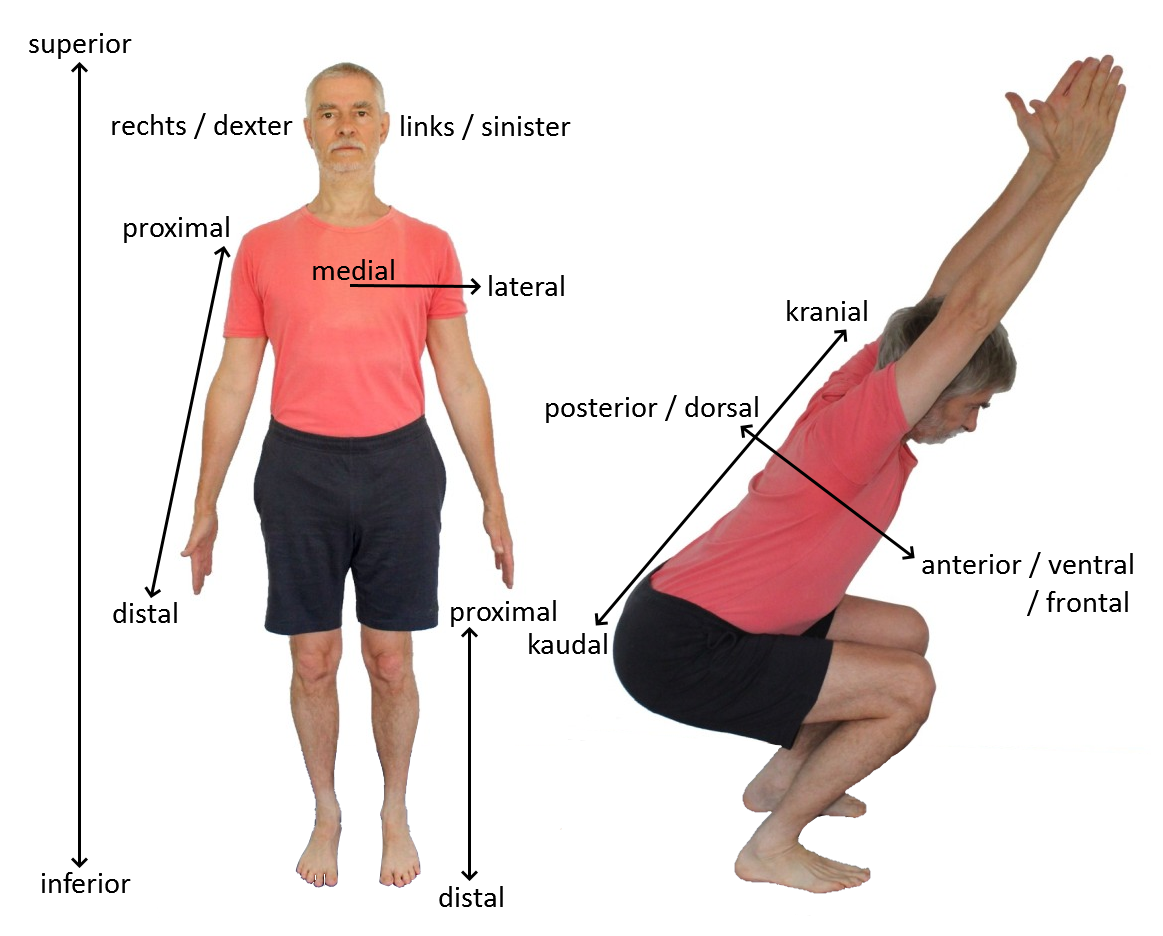
Medial tract
Part of the autochthonous back muscles: interspinal system and transversospinal system.
Median plane / midsagittal plane
The sagittal plane that divides the body into a left and a right half, running exactly in the middle of the body.
Mediastinum
see movement physiology – circulation/mediastinum.
Medulla oblongata
see movenemt physiology – nervous system/medulla oblongata.
Medullary cavity
see movement physiology – bone/medullary cavity.
Meninges
see movement physiology – nervous system/meninges.
Meniscus
Disc-shaped but non-circular continuous („meniscus“ means „little monk“) cartilage that has a buffering effect in a joint. In the case of the knee joints, the menisci are divided into three zones, of which the inner meniscus is not supplied with blood and therefore degenerates more easily and the outer meniscus is less susceptible due to its blood supply. In addition to degeneration due to excessive wear or lack of exercise, traumatic meniscus tears are not uncommon. See also the in the pathology section: meniscus damage. The task of the menisci of the knee joint is to keep some of the force with which the femur rests on the tibia of the lower limb away from the cartilage coverings of the bone ends, i.e. to relieve them. Other menisci are located in the acromioclavicular joint or the ulnar wrist, for example.
Meniscus root
see joint – knee joint/meniscus root
Metaphysis
see movement physiology – bone/metaphysis.
Metatarsal head
Metatarsal heads are the distal ends of the metatarsal bones. The proximal ends are called the base.
Metatarsus
The section of the foot around the metatarsal bones, i.e. between the tarsal bones and the toes.
Mikulicz line
see movement physiology/Mikulicz-line.
Midfoot running
Compromise between rearfoot running and forefoot running.
Middle hand
The section of the handaround the metacarpal bones, i.e. between the carpal bones and the fingers.
Metacarpal bone / Metacarpalia
the bones between the carpal bones and the fingers. One metacarpal bone belongs to each ray.
Moment
the effect of a force acting on a point of a rotatable body, e.g. as a tilting moment or torque
monoarticular
see movement physiology – muscle/monoarticular.
Monotonous
A mathematical term that states that a function (with a one-dimensional, ordered range of values) never decreases (monotonically increasing) or never increases (monotonically decreasing). If it is also impossible for sections to remain constant, this is referred to as strict monotonicity. If, for example, the position of the heel (to be precise, one of the processes of the calcaneus) in the transition from the downface dog to the upface dog or vice versa is represented as a function of the distance to the wall, this should ideally be strictly monotonic. In contrast, in this transition the shoulder position (determined by the center of rotation of the glenohumeral joint, for example) cannot be a monotonic function in sufficiently mobile people, as the distance from shoulder to heel is greater than in both positions when the hip joint is extended.
Morning stiffness
With morning stiffness, a distinction must be made as to whether it relates to the muscles or the joints. It must be distinguished from start-up pain, as the stiffness itself does not necessarily have to be painful. A certain degree of muscular morning stiffness in the area of the autochthonous back muscles is physiological: the intervertebral discs of the spine reabsorb fluid overnight after the partial body weight bearing down on them has squeezed fluid out of them during the day. This effect can be clearly seen in a decrease in body size throughout the day. If the intervertebral discs absorb fluid overnight, the muscles covering the vertebral segments are then under noticeably increased tension, which is accompanied by a feeling of stiffness and, not least, increased susceptibility to injury.
Joint stiffness in the morning, on the other hand, is an important symptom of serious joint diseases such as arthrosis, rheumatoid arthritis (rheumatism), polymyalgia rheumatica and Morbus Bechterew. In the latter, it mainly affects the spine, but also the area
sacrum and buttocks. The morning stiffness of arthrosis usually lasts only half an hour and subsides slowly, while the morning stiffness of RA, for which morning stiffness and start-up pain are the main symptoms, lasts longer. The symptoms often also restrict the employment of those affected. The average impairment of work activity in a study with over 1000 RA patients was 8-9 hours per week, while they only had an estimated effectiveness/productivity of 40%. However, this is not a sufficiently sharp differentiation criterion, as 1/6 of all those affected by arthritis of the hand have at least one hour of stiffness. In arthrosis, there is often also pain in the morning. In ankylosing spondylitis, morning stiffness usually lasts for more than half an hour. Stiffness often occurs even after longer periods of rest during the day.
Motoneuron
see movement physiology – nervous system/moto neuron.
motor unit
see movement physiology – nervous system/motor unit.
Motor end plate / myoneural junction
see movement physiology – nervous system/motor end plate.
Muscle
See the dedicated page on muscles and the overview of all muscles.
Muscle belly
see movement physiology – muscle/muscle belly.
Muscle failure
see movement physiology – muscle/muscle failure.
Muscle fibre types
see movement physiology – muscle/fibre types.
Muscle head
see movement physiology – muscle/muscle head.
Muscle injuries
see movement physiology – muscle injuries.
Muscle pennation
see movement physiology – muscle/pennation.
muscle performance
see movement physiology -muscle/muscle performance.
muscle performance capability
see movement physiology-muscle/muscle performance capability.
Muscle spindle
see movement physiology – muscle/muscle spindle and movement physiology – nervous system/muscle spindle.
(muscular) imbalance
Imbalance in the tone, strength or flexibility of the muscles that cover a joint. The agonist-antagonist ratio – which also refers to one or more dimensions of movement – or side disrepancies play a role here. This can be caused by incorrect posture, incorrect loading, one-sided training, one-sided activities, poor technique, injuries or insufficient regeneration, as well as a lack of exercise. This can result in painful muscle tension, overloading of tendons and damage to the joint, especially the cartilage. If incorrect posture is accompanied by an end-degree position, such as a pelvis tilted effortlessly in maximum extension or a hyperextended knee or elbow joints, it can alter ligaments, fascia, capsules and cartilage. The imbalance is not a disease in itself, but it can become pathogenic from a certain degree. Most people have some form of imbalance to a greater or lesser extent, but these can often remain asymptomatic for a long time or remain completely asymptomatic. Common examples of muscular imbalances include
- Shortened hip flexors leading to a hollow back, overtensioning of the autochthonous back muscles of the lumbar spine, weakness of the abdominal muscles and hip extensors
- Rounded back (in direction of a hunch), caused by poor posture or shortened pectoral and abdominal muscles (pectoralis major), for example
- Head forward posture, which overstrains the neck muscles and causes the cervical spine flexors to slacken
- Overtension of the protractors and weakness of the retractors of the shoulder blades
- Partially elevated shoulder blades resulting in weak depressors and hypertonus of the trapezius and levator scapulae in particular
- Sitting with a leaning back and a lumbar spine kyphosis, which weakens the autochthonous muscles and puts them under excessive tension, at the same time weakening the hip flexors and hip extensors.
- Imbalance of the internal rotators and external rotators of the shoulder joint due to activities at the computer, working in an internally rotated position as well as throwing activities
- Imbalances in all parts of the spine resulting from sleeping positions such as side sleeping and stomach sleeping, especially when the extremities legs or arms are positioned asymmetrically.
- Imbalances resulting from sitting with one thigh crossed on top of the other or frequent sitting cross-legged or in lotus position for long periods, especially with favoring one leg
- Weaknesses in the abductors of the hip joint, which become visible through Trendelenburg or Duchenne signs
- Imbalances by poor posture due to somatizing
As a rule, imbalances are not detectable with imaging techniques, but rather with electromyography (EMG). In addition to the anamnesis, functional diagnostics are the most important diagnostic tool. One of the typical pathomechanisms is that muscles that have postural tasks (muscles with a more tonic function, often more profound) are overloaded by a poor posture, whereupon other muscles step in that have more moving (phasic, usually more superficial) than holding tasks. However, these will tire all the more quickly and react by shortening and hardening. It must be assumed that they break down serial sarcomeres under these conditions. In principle, the more the body is challenged, whether in sport, leisure or at work, the greater the effect of imbalances. They then have the effect of reducing performance, disturbing well-being, delaying regeneration and increasing susceptibility to injury. Quite a few of the imbalances are also likely to result from activities in these areas of life. The increased tone and tension of a muscle can reduce blood flow (see the extreme case of compartment syndrome) and thus cause pain. This pain can lead to further deterioration, possibly in other muscles, through avoidance behavior. This vicious circle must be broken by training. Put into a simple formula of cause and result:
- Increased demand results in hypertrophy, increase in strength and tone (depending on sarcomere length under stress)
- Reduced demand results in dystrophy and loss of strength, often also of flexibility
- Overload results in hypertrophy with a tendency to tension
In the case of imbalances, it is always necessary to think beyond the affected area, and in terms of muscle chains and the effect of gravity, other affected areas must also be examined.
Musculoskeletal system / locomotor system
The locomotor system or musculoskeletal system is the part of the body that keeps it in shape and enables targeted changes to this shape, for example for the purpose of locomotion or voluntary actions. The musculoskeletal system is divided into an active musculoskeletal system and a passive musculoskeletal system:
– Active musculoskeletal system
The active musculoskeletal system includes the skeletal muscles together with their tendons and tendon sheaths, their connective tissue covering (fasciae around muscle fibers, muscle fiber bundles and heads), and the bursae, which protect muscles or their tendons against hard pressure, for example from bones.
– Passive musculoskeletal system
The passive part of the musculoskeletal system, also known as the supporting/bracing apparatus, consists of the bones with their cartilage coverings and connecting cartilage and the joints with their various parts, which, in addition to the bones involved, are primarily the ligaments, intervertebral discs (where present) and joint capsules, as well as the synovia formed by the innermost layer of the capsule.
Myocardium
see movement physiology – circulation/myocardium.
Myogelosis
see movement physiology – muscle/myogelosis.
Myokines
see movement physiology – muscle/myokines.
Myosteatosis
Myotome
see movement physiology – nervous system/myotome.
N
Night pain
Night pain means pain that only occurs at night. It is usually joint pain caused by arthritis, osteoarthitis/arthrosis and rheumatic diseases, especially rheumatoid arthritis. Generally, this type of night pain often also occurs during the day when resting for long enough. During pregnancy, night pain also occurs from time to time, mainly due to fluid accumulation in the lymph vessels of the extremities, especially the legs. Several liters of fluid can be stored, which leads to tension pain and tenderness in the support area.
Narrrowuse syndrome
Narrowuse syndrome refers to all disorders that result from the limited use of the musculoskeletal system. To give an example: an office worker who has a sedentary computer-equipped job, where he walks to the printer and the coffee machine about once in the morning and once in the afternoon, each time standing in an adjoining room on the same floor, and who also doesn’t make himself comfortable on the couch every other afternoon or so, but goes for a long ride on his racing bike, is certainly performing well in terms of cardiopulmonary prevention with his sporting activity. In addition, the strength of the lower extremities should be ensured in some important main functions. However, his range of movement is very limited and he only uses many joints in a very narrow ROM, some of them very frequently under load. It is to be expected – and practice regularly confirms this – that his flexibility will decrease both in the joints that he uses only a little and when he does, then in a small ROM, and in the joints that he uses very frequently but with a not too large ROM.
He misses frontal abduction and lateral abduction in the shoulder joint, also exorotation and abduction in the hip joint. This is also predominantly in clear flexion, which should at least significantly shorten the short head of the biceps femoris. Given the work performed by the hamstrings, the frequently iterated medium range movements in the knee joint also contribute to its significant movement. The rectus femoris is well below medium sarcomere length both in occupational and even more so in athletic activity, so that it is also likely to shorten significantly consiodering its power development when cycling. The same naturally applies to the iliopsoas. In general, extension is underrepresented in his flexion-oriented lifestyle, both in the hip joints and in the spine. The elbow and knee joints are also rarely extended. His cervical spine can be in hyperlordosis if he sits poorly, just as it typically is when riding a racing bike. The thoracic spine will also often be in kyphosis, assuming poor sitting behavior, and it certainly is when riding a racing bike. Extensions in many joints will therefore be difficult for him. The expected progressive contractures will sooner or later becomd incomfortable and, in time, disorders will manifest.
If fitness in its classic definition is seen as a product of the basic components of endurance, strength, flexibility, coordination and speed, then the test person will not find himself at the top of the list of fitness athletes, as the discipline of flexibility significantly depresses the product. He will not score particularly well (achieve a good factor) in „speed“ either, as admittedly the muscular performance of some of the muscles of the lower extremities and the associated hip joint muscles is not bad and therefore a minimum level of speed must also be present. However, due to his limited flexibility, he will have a rather low ROM and will therefore not gain much swing in real speed exercises such as throwing movements and jumping movements to get to the front of the field. After all, the kinetic energy (whether of the thrown object or the accelerated limb) can be described as an integral of the force developed over the radian measure. movement physiology – nervous system
Nerve
see movement physiology – nervous system/nerve.
Nerve fibre
see movement physiology – nervous system/nerve fibre.
Neuroplexus
see movement physiology – nervous system/neuroplexus.
Nerve impulse
see movement physiology – nervous system/nerve impulse.
Nerve system / neural system
see movement physiology – nervous system.
Nerve root
see movement physiology – nervous system/Nerve root.
Nerve root compression syndrome
see movement physiology – nervous system/nerve root compression syndrome.
neuro-endocrine system
see movement physiology – nervous system/neuro-endocrine system.
Neuron
see movement physiology – nervous system/neuron.
neuropathic pain
see movement physiology – nervous system/neuropathic pain.
neuroradicular
see movement physiology – nervous system/neuroradicular.
Neurotransmitter
see movement physiology – nervous system/neurotransmitter.
Neutral zero
Upright posture in which the feet are parallel and closed, the knees are extended, the pelvis is upright, the upper body including the cervical spine is straight and the arms rest against the body in such a way that the inner elbows and palms – in contrast to standard anatomical position – point towards the body. Neutral-zero corresponds to tadasana and must not be confused with the very similar standard anatomical position.
Neutral zero method
The range of motion within a movement dimension is usually specified using the neutral zero method, starting with flexion and ending with extension. If both are possible, there is a zero in the centre, e.g. 150° – 0° – 5° for 150° flexion and 5° extension or hyperextension in the knee joint. If there is a mobility restriction of any kind, a zero is shown at the end of the affected side and the achievable value is in the centre, e.g. 150° – 10° – 0° for an extension deficit of 10° in the knee joint.
Night pain
see movement physiology – nervous system/night pain.
Nociceptor
see movement physiology – nervous system/nociceptor.
Nociceptive pain
see movement physiology – nervous system/nociceptive pain.
NRS (Numeric Rating Scale / Numeric Analog Scale)
The method of assessing intensities or other quantities (quantifiable variables) with numbers, usually from 0 to 10, is usually referred to as Numeric Rating Scale (NRS). This method is mostly used to query pain intensities. Here, 0 stands for „no perceptible pain sensation at all“ and 10 for the maximum imaginable pain. Multiplied by the number 10, percentages can then be obtained. The NRS is usually used to measure current pain, but it can also be used to measure average pain over a period of time. In principle, the NRS is also suitable for completely different uses than pain intensity.
Nutation / contranutation
The movement of the SIJ (sacroiliac joints) around a horizontal transverse line of approx. maximum 4 degree.
O
oblique abdominal muscles
the oblique abdominal muscles: Mm. obliqui externi abdomini and Mm. obliqui interni abdomini, which are crossed at a large angle and contribute to the rotation of the trunk, lateral flexion and flexion in the lumbar spine and lower thoracic spine. With regard to rotation, they are partly synergists and partly antagonists to the corresponding muscles of the oblique system of the autochthonous back muscles, and antagonists with regard to their extensor effect. The oblique abdominal muscles belong to the expiratory auxiliary respiratory muscles.
Obstructive
see movement physiology – circulation/obstruktive.
1RM (Einwiederholungsmaximum)
The 1RM or one-repetition maximum is the maximum weight that can be achieved in a specific exercise in a single, cleanly performed repetition after an adequate warm-up. These are usually exercises such as bench presses, neck presses, rowing, lat pulldowns, deadlifts or squats. As these exercises invariably involve several muscles that work together synergistically or in a kinetic chain, the 1RM only represents the maximum repetition of the individual muscles in terms of their tendon force, which is much more difficult to determine. If it is not possible to determine the 1RM, for example because a correspondingly high resistance cannot be achieved with an adjustable grip strength trainer or a training device does not provide a correspondingly high weight capacity, the 1RM can be approximated from a different, not too large number of repetitions using the following table, which shows the assignment of the number of repetitions to the percentage of 1RM.
- 1: 100%
- 2: 95%
- 3: 92%
- 4: 89%
- 5: 86%
- 6: 84%
- 7: 81%
- 8: 79%
- 9: 76%
- 10: 74%
- 11: 71%
- 12: 68%
Opposition
Opposing the thumb to the hand, enables objects to be gripped. The little finger is also capable of opposition to a small degree.
Origin
The origin usually refers to the insertion of a muscle, tendon or ligament, which – in contrast to the attachment – lies further proximal.
Orthosis
Non-invasive orthopaedic aid attached externally to the body with the purpose of providing support, restricting movement or relieving pressure on tissue or joints. This includes all types of splints, support devices, girdles and corsets. Orthoses can be complex and made of several materials. Bandages are not usually included. The orthosis is therefore a – usually passive – piece of exoskeleton attached to the body from the outside.
Ossicles
Chipped bone particles (the pathological case: a joint mouse / loose body ) or very small (physiological) bones.
Osteochondrosis
Sclerosis of the subchondral area of the vertebral bodies occurring as a result of chondrosis.
Osteophyte
see movement physiology – bone/osteophyte.
Outcome
Outcome or therapy result refers to the final result of a measure, mainly therapy or prevention. The former term therapy success is no longer used today because it is not value-neutral. Clinical studies can be used to evaluate procedures by measuring the outcome against previously defined endpoints using various criteria. These criteria can be, for example, survival time, tumour-free intervals, biomechanical parameters, performance data, pain-free intervals, remission time (or freedom from recurrence), laboratory values, histological findings or simply a quality of life score or an assessment of the ability to work. According to the AWMF (8th Newsletter, 2003), outcome is to be understood as a „construct of different outcome measures, different endpoints with a disease-specific weighting, which reflects the needs of the individual patient and society.“
Outward rotation / external rotation (shoulder blade)
Movement of the scapula in the plane in which it mainly extends, with the inferior angulus (lower tip) pointing outwards and upwards, which is a prerequisite for raising the arm above 90°. These muscles rotate the shoulder blade outwards. In the yogabook, for the shoulder blade the term outward rotation is preferred to easily distinguish this movement of the shoulder blade from that of the external rotation of the humerus in the glenohumeral joint.
Outward rotators / external rotators (shoulder blade)
Muscles that turn the shoulder blade outwards at the bottom, i.e. into outward rotation:
Overcrossing
The foot is placed beyond the median line on the contralateral side of the body. This can be caused by:
- Muscular imbalance, particularly weaknesses in the hip muscles, especially the abductors, hypertension of the adductors
- Functional leg length discrepancies: predispose to overcrossing, especially of the longer leg
Overcrossing leads to overpronation, ITBS (runner’s knee), shin splints and knee pain.
Overhand grip
The overhand grip refers to gripping an object, often a piece of sports equipment such as a dumbbell, with the back of the hand facing upwards and the object or its handle gripped from above by the palm of the hand. In contrast to the underhand grip, all muscles with a dorsiflexor effect in the wrist, i.e. the finger extensors and the pure dorsiflexors of the wrist, are required in addition to the finger flexors, which have to secure the grip. In contrast to the underhand grip, the forearm is in pronation here and the arm biceps can work less well, so that the brachialis provides a higher proportion of the force exerted and the maximum force that can be achieved is lower.
Overpronation / Hyperpronation
see movement physiology/hyperpronation.
Overstriding
Placing the foot too far in front of the body. Overstriding slows you down and leads to rearfoot running with a loss of efficiency and additional strain on the joints, especially the ankle joints, as well as overloading the tendons of the pronator fibularis longus and fibularis brevis and PFPS (jumpers knee, patellar tendinopathy). Weakness of the gluteus maximus is often a contributing cause.
Oversupination / hypersupination
see hypersupination.
Overtraining
Overtraining can refer to two different things:
- overreaching (also known as functional overreaching), which leads to a short-term drop in performance in the days following training. The effects are short-term, there are hardly any psychological symptoms and after a few days and completed regeneration, training can be continued at a slightly higher level (supercompensation). Depending on the severity of the training, regeneration should be completed within 96 hours at the latest, after which a window of supercompensation of limited duration begins.
- The chronic training-related overload situation known as overtraining syndrome (OTS) with a sustained drop in performance that cannot be explained in any other way for several weeks, usually accompanied by psychological symptoms. The minimum duration of the drop in performance for a diagnosis of OTS is 2-3 weeks.
OTS occurs when frequent training is carried out without sufficient regeneration. With each training session, the body does not return to the original performance level or higher, let alone to the desired level of maximum supercompensation, but to a level below the level at the start of the last training session. Overtraining is characterised by the following possible symptoms:
- Decreasing (instead of increasing) performance (main symptom)
- Possible loss of motivation or concentration
- Increased susceptibility to injury and infection
- Increased resting and working heart rate or exercise heart rate, reduced recovery heart rate (only sympathetic overtraining)
- possibly headaches
- Sleep disorders (only sympathetic overtraining)
- Triggering of depression
If some of these symptoms are identified and overtraining is assumed to be the cause, this has the status of a disease.
However, these symptoms are not very specific and are only some of around 200 symptoms that have been described in connection with OTS to date, including symptoms such as heavy legs, muscle pain, joint pain, so that overtraining has more the character of a diagnosis of exclusion. There are various hypotheses regarding the triggers of the somatic and physiological disorder: cause-related, clinic-related and pathophysiological. If overtraining is detected, a break from exercise is obligatory, and sports medical supervision may be necessary. Doping or medication abuse is by no means a suitable way of dealing with the disorder. In severe cases, therapy can be lengthy and difficult. It is best to be alert to the possibility of overtraining when organising training. In contrast to functional overtraining, which leads to an (albeit small) increase in performance,
nonfunctional overtraining does not lead to an increase in performance. Repeated non-functional overtraining can then lead to OTS.
Various factors can lead to OTS, and there are often several of them:
- Training errors
- Excessively intensive training over a longer period of time
- Greater expansion of the training ranges in a short period of time
- long monotonous training sessions
- too many competitions
There are often accompanying aggravating factors such as
- Conflicts in or outside of sport
- Changes in life circumstances
- Organisational deficiencies
- Shortcomings in time management
- upcoming exams
- Personal losses and setbacks
- Dietary deficiencies, lack of nutrients
- Pressure to perform
- Change of time zone, climate zone, lack of altitude adaptation
- Insufficient rest after injury or illness
The decrease in heart rate variability HRV can be seen as a rather early indicator. With further overtraining, the resting heart rate (RHR) would then also increase. Mental status can be assessed using various methods: Recovery-Stress Questionnaire for Athletes (RESTQ), BFS mood scales, Profile of Mood State (POMS), Nitsch’s scale of wellbeing. In the OTS, reduced levels of the stress hormones cortisol, adrenaline and noradrenaline can be detected at peak load compared to the individual baseline values, which must be known for this purpose; the same applies to the 24-hour urine collection. Conversely, a reduction in known levels can also be used for early detection.
A distinction must be made between sympathetic overtraining, which can occur primarily in strength and speed disciplines, and parasympathetic overtraining, which occurs primarily in excessive endurance sports with not necessarily very high performance development. Both forms have four main symptoms in common:
- A drop in performance, usually between 3%-6% in top athletes
- Reduced capacity (training volume)
- Heavy, exhausted muscles
- Delayed regeneration
Based on the symptoms and the activity causing it, these two forms can be distinguished quite easily. It is also debated whether
sympathetic overtraining and parasympathetic overtraining are not so much two different forms of overtraining, than two successive phases in which parasympathetic overtraining follows sympathetic overtraining with a delay of a few weeks if no intervention has been made. There is also the view that functional overtraining, sympathetic overtraining and parasympathetic overtraining represent three stages.
When overtraining is mentioned and not specified in more detail, it is usually sympathetic overtraining that is meant.
Sympathetic overtraining
Sympathetic overtraining is a phenomenon that occurs primarily in sports with rather short but very high peak loads. Excessive training in weight training or sprinting disciplines can lead to this. Increased resting heart rate and increased resting heart rate and increased resting blood pressure as well as decreased recovery heart rate (increased afterload heart rate) and increased afterload blood pressure. Other symptoms are
- Increased resting heart rate
- increased resting blood pressure
- Decreased recovery pulse (increased post-exercise pulse)
- Increased post-exercise blood pressure
- reduced performance
- reduced appetite
- unwanted weight loss
- Delayed regeneration
- perceived lack of energy
- impaired sleep
- night sweats
- Psychological symptoms such as irritability
- emotional instability,
- indifference
- restlessness
- Reduced desire for training and competition
- disturbed cognitive processes
Parasympathetic overtraining
In contrast to sympathetic overtraining, parasympathetic overtraining does not occur during strength or speed disciplines, but during excessive endurance sports, such as long-distance running (running). Performance is also reduced here, but there is a noticeable „runner’s bradycardia“. Body weight and appetite are not affected, sleep disturbances are also rare, but a certain sluggishness or phlegm occurs, as well as a rather depressive mood. After exercise, the recovery pulse is quite pronounced. Fatigue and lack of motivation prevail. Above all, frequent hours of low-intensity exercise can induce parasympathetic overtraining.
Overuse
Overuse means overloading and refers to a load that exceeds the load-bearing capacity of a structure. The causative factors and the affected structures can be diverse. The bradytrophic tissues are frequently affected by overuse syndrome: tendons (tendinitis, tendinosis, tendinopathy) and their tendon sheaths (tendovaginitis, together with tendinitis also known as tendosynovitis), ligaments, capsules, cartilage, bones and the bursae that cover the muscles or their tendons (bursitis). Cartilage with a turn over beyond the lifespan is frequently affected by overuse. One of the most common examples, apart from the all too familiar meniscus of the knee, is the disc in the ACG joint (acromioclavicular joint). These are often already massively damaged by arthritis in the fourth decade of life and are often no longer detectable in the fifth decade of life. The muscle itself can also get into a position in which it can no longer withstand the strain, in which case it reacts with a tendency to spasm, strain, hypertonus, loss of performance, overuse, for example. As the muscle is designed for rapid, extensive metabolism, it is less affected. Overuse can occur in sport, but also in non-sporting professional activities, e.g. as RSI syndrome in secretaries or as golfer’s elbow in road workers who frequently work with a shovel. In sport, overuse is often associated with inadequate increases in performance or inadequate performance requirements for the level of training. Those who take up sports training (for the first time) are usually confronted with the necessity that various parts of their body, not only their musculoskeletal system, do not adapt to the required performance or strength demands quickly enough. The body adapts most quickly to strength and cardiopulmonary endurance demands. The bradytrophic tissues of the musculoskeletal system adapt with a significant delay due to their sometimes far greater turn over (renewal time), so that, depending on the demand, they cannot provide adequate resilience to the increased performance. They are then unable to regenerate sufficiently from one demand to the next and adapt even less, so that degeneration symptoms are often the result.
P
Pain
see movement physiology – nervous system/pain.
Pain anamnesis / history
see movement physiology – nervous system/pain anamnesis.
pain at motion
see movement physiology – nervous system/pain at motion.
Pain at rest / rest pain
see movement physiology – nervous system/pain at rest.
Pain in motion
see movement physiology – nervous system/pain at motion.
Pain localization
see movement physiology – nervous system/pain localization.
Pain modality
see movement physiology – nervous system/pain modality.
pain on initial movement
see movement physiology – nervous system/pain on initial movement.
pain on percussion
see movement physiology – nervous system/pain on percussion.
Pain quality
see movement physiology – nervous system/pain quality.
painfulness at motion
see movement physiology – nervous system/painfulness at motion.
Painfulness in motion
The ability of a part of the musculoskeletal system (rarely: internal organs) to cause pain on movement through active or passive movement, even without load.
Palmar aponeurosis
The aponeurosis palmaris is the tendon plate of the palm and consists of multiple longitudinal and transverse fibers in different layers. A final layer of connective tissue lies above this. Depending on the author, only the latter or the whole is referred to as palmar fascia. Laterally, the palmar aponeurosis merges into the fascia of the thenar and hypothenar muscles.
Palmar fascia
The aponeurosis palmaris is the tendon plate of the palm and consists of multiple longitudinal and transverse fibers in different layers with a superficial connective tissue layer. Some authors refer exclusively to this as the palmar fascia, but do not include the aponeurosis.
Palmar flexion / palmar flexion (hand)
Increase in the dorsal (back of the hand) angle of the hand to the forearm at the wrist, i.e. movement of the palm of the hand towards the forearm, i.e. the back of the hand away from the forearm.
Palmar flexors
Group of muscles that perform palmar flexion, i.e. bring the palm of the hand closer to the forearm
Palmare plate
Synonym for the palmar ligament, which covers each metacarpophalangeal joint and the interphalangeal joints on the palmar side and protects against hyperextension.
Palpation
Pannus
Connective tissue proliferation (fibrous granulation tissue) of the synovium that occurs as part of chronic inflammatory conditions such as RA or septic arthritis. This hyperplasia can grow into the joint space and impair the function of the joint to the point of complete loss of function. The spectrum ranges from deformities of the articulating bones to instability of the joint to ankylosis. Pannus tends to destroy cartilage and bone, with pro-inflammatory cytokines of the cartilage also playing a role.
Paraesthesia
see movement physiology – nervous system/paraesthesia.
Parasympathetic / Parasympathetic nercous system / parasympathicotone
see movement physiology – nervous system/parasympathetic nervous system.
Partial body weight
the weight that is supported and is not itself part of the supporting body parts (usually extremities). In the example of handstand, this is the total body weight minus that of both arms, in the case of ardha chandrasana the total body weight minus that of the standing leg. The partial body weight is an important factor in the moments that occur in the supporting extremity or extremities or their joints, but ultimately their amount also depends on the lever arm (distance from the center of rotation of the joint to the center of gravity of the partial body) and the sine of the angle to the direction of gravity.
Passive mobility
The range of motion in a joint that an examiner can measure. Physiologically, this is not significantly greater than the active range of motion, but the two can differ considerably if there are changes in the joints or muscles. A good example of the difference is the biceps femoris, which can flex the knee joint about 150° in the prone position before it becomes actively insufficient, while the knee joint can be passively flexed much further if the flexibility of the antagonistic quadriceps allows it.
Passive insufficiency
see movement physiology – muscle/passive insufficiency.
Patellar dyskinesia
Patellar dyskinesia is the term used to describe incorrect movement of the patella in the femoropatellar sliding bearing. There are several possible reasons for this, such as unfavorable traction ratios of the quadriceps parts, usually too little traction of the vastus medialis or excessive traction of the rectus femoris or vastus lateralis. Incorrect movement of the patella can also occur during movement sequences, for example when in running, towards the end of the standing leg phase, i.e. when pushing off, the lower leg is turned out in the knee joint. The same applies if the lower leg rotates outwards in the knee joint during wide forward swing of the leg. In the first case, the biceps femoris may be disproportionately strong or under disproportionate strong tone compared to the inner hamstrings or the latter may be too weak; in the second case, the flexibility of the biceps femoris may be too low in relation to the inner hamstrings. Malformations of the patella, in particular a fin that is too weak, or a tibial tuberosity that is located too far laterally can also lead to patellar dyskinesia.
Patellar luxation
Dislocation of the patella. Patellar dislocations are painful and usually occur when the knee joint is largely or fully extended, usually the patella dislocates laterally. There are a number of reasons for this. As part of the physiological final rotation, the lower leg is turned out in the knee joint, which pulls the patellar ligament slightly laterally. In addition, the contact pressure of the patella in extension or hyperextension of the knee joint is minimal and the guidance of the dorsal fin of the patella in the intercondylar sulcus decreases with increasing extension of the knee joint. As a result, the intercondylar sulcus bends slightly laterally in the cranial region. If due to muscular imbalance (weakness of the inner hamstrings or the popliteus) the internally rotating torque is too low (regarding the externally rotated position in final rotation), the lateralization tendency of the patella is also increased. In cases with a tendency to patellar dislocation, the quadriceps as a whole, but especially the medial vastus and the inner hamstrings should be trained to reduce the tendency to dislocatate laterally, provided there is no other regional disorder. The vastus medialis can be very important here, as its caudal part (also known as the „vastus medialis obliquus„) runs obliquely to transversely and is primarily responsible for centering the patella. It is equipped with corresponding fiber types and receptors for this purpose. A knock-knee also leads to unphysiological guidance and incorrect traction on the patella, as it is pulled laterally. A laterally pulled patella regularly leads to an increased load on the lateral half of the femoropatellar sliding bearing and thus also on the lateral half of the retropatellar cartilage, which can lead to patellofemoral pain syndrom/chondropathia patellae (PFPS) and later to retropatellar arthrosis.
See also traumatic patella luxation and atraumatic patella luxation.
Patella alta
The patella alta is a patellar elevation towards the cranial, as occurs in a rupture of the patellar ligament. Physiologically, this ligament holds the caudal patellar pole at a fixed maximum distance from the tibial tuberosity. However, if it is teared, the tonus of the quadriceps pulls the patella towards the cranial, even if it is not consciously innervated. The patella alta is the opposite phenomenon to the patella baja, in which a tear of the tendon of the quadriceps (quadriceps tendon) proximal to the cranial patellar pole causes it to lack traction and the patella to slip inferiorly.
Patella baja
The patella baja is a patellar depression in the inferior direction, as occurs with a rupture of the quadriceps. Physiologically, the tonus of the quadriceps pulls the patella in a cranial direction, even if it is not consciously innervated. This traction is missing in this disorder, so that the patella slips to the inferior. The patella baja is the opposite phenomenon to the patella alta, in which a tear of the lig. patellae close to the caudal patellar pole, its traction is missing and the patella slips cranially.
pathognomonic
A symptom is called pathognomonic if it can only occur in a specific disease. Non-obligatory symptoms can also be pathognomonic. Examples of pathognomonic symptoms include:
- the Kayser-Fleischer ring for Wilsen’s disease
- the Bence-Jones proteins in multiple myeloma
- Patella patella alta symptoms with simultaneous ipsilateral patella baja symptoms (of the respective fragments) in the case of a transverse fracture or a comminuted fracture of the patella
- Erythema migrans in Lyme disease
Pelvis
The pelvis is generally understood to be the space occupied by the large pelvis plus the small pelvis. The large pelvis can be seen as part of the abdominal cavity, as some important organs of the abdominal cavity extend seamlessly into the large pelvis.
See also here.
– Pelvis, small
The lesser pelvis is the lower space between the iliac blades (ala ossis ilii) of the ilium, which is bounded cranially by the linea terminalis. This space contains, among other things, the urinary bladder, rectum and, in females, the uterus, ovaries, vagina and, in males, the prostate.
– Pelvis, large
The large pelvis is the upper space between the iliac blades (Ala ossis ilii) of the ilium, which borders caudally on the small pelvis and is delimited by the Linea terminalis. This space contains some abdominal organs, e.g. the ileum and the sigmoid.
Pelvis girdle (hip girdle, bony pelvis, pelvis arch)
The pelvic girdle is the bony structure that connects the spine to the lower extremity leg, i.e. the two hip bones and the sacrum between them. In contrast to the dorsally open shoulder girdle, the pelvic girdle is closed, the covered joints are the two ISG dorsally and the pubic symphysis ventrally.
Pelvic torsion
A pelvic torsion is defined by a hip bone tilted forward in standard anatomical position on one side compared to the other side. Typically, this twisting occurs dorsally in the two sacroiliac joints and ventrally in the pubic symphysis, so that the respective degree of nutation is unequal in both. It is often the result of laterally unequal tension of the hip extensors and hip flexors, especially the iliopsoas, rectus femoris as hip flexors and gluteus maximus as the strongest hip extensor, but also the hamstrings, which make a significant contribution to extension, especially at lower flexion angles in the hip joint and with less force exerted for extension.
Among the hip flexors, the iliopsoas is particularly noteworthy, as it is often at the edge of its ROM in standard anatomical position in less mobile people anyway. Pelvic torsion can be recognized on inspection, for example, by a ASIS that protrudes further on one side or a dorsally unevenly high PSIS. It can also be perceived in the supine position (e.g. savasana) by the fact that the two iliac crests are at an unequal distance from the floor. Often, especially when the flexibility of the hip flexors on one side is less than that of the other side, one knee joint flexes more than the other in savasana.
Pelvic obliquity
a pelvis tilted in standard anatomical position to one side in the frontal plane. Both hip joints and both ASIS are then unequal in height, or in other words, the vertical axis of the pelvis is not vertical. This can be caused by (functional or rarely also anatomical) leg length discrepancies, as well as subluxations in the ankle, knee or hip joints. An unequal pull of the adductors and abductors can also lead to pelvic obliquity: in standard anatomical position, the hip joints normally form an isosceles trapezoid with the heels. If one leg is inclined differently to the vertical than the other, it pulls the hip down with it and the pelvis is tilted.
A persistent pelvic obliquity usually causes a scoliosis of corresponding extent, in the full extent later on double S-shaped. The body corrects the static problem caused by a pelvic obliquity and thus a oblique sacrum in such a way that, with optimal compensation, the center of gravity of the large partial body weight above the pelvis runs centrally through the line connecting the two acetabuli.
Pelvic obliquity should not be confused with pelvic torsion, but can also occur together with it.
Pericardium
see movement physiology – circulation/pericardium.
Perineum
The area of the upper body delimited by the dorsal anus and genital area ventrally and laterally by the thighs. In standard anatomical position, this is the lowest area of the upper body.
Periosteum
see movement physiology – bone/periosteum.
Percussion
Phalange (phalanx)
Finger or toe phalanx. Like toes 2-5, fingers 2-5 have three phalanges, while the thumb (pollex) and big toe (hallux) each have two.
Physiological kyphosis (thoracic spine)
The kyphotic curvature measurement of a healthy thoracic spine in standard anatomical position or neutral zero.
Physiological lordosis (lumbar spine)
The lordotic curvature measurement of a healthy lumbar spine in standard anatomical position or neutral zero.
Pia mater
see movement physiology – nervous system/pia mater.
Pivot joint / rotary joint / trochoid joint
see movement physiology – joint shapes/pivot joint
Plane joint
see movement physiology – joint types/joint shapes
Plantar fascia
The aponeurosis plantaris or plantar aponeurosis is a tendon plate between the calcaneus on the one hand and the metatarsophalangeal joints on the other. It is mode superficial that the plantar ligaments such as the plantar long ligament. It covers the metatarsal bones and some tarsal bones. It thus protects the deeper structures (nerves, tendons, blood vessels) and secures the position of the fat pads of the foot. It is partly the insertion for
It is important as a passive part of the tension belt to prevent the longitudinal arch of the foot from collapsing and to limit the extension of the foot when unter load.
Plantar flexion (foot)
Increasing the dorsal (back of the foot) angle of the foot to the lower leg. This movement is performed by the plantar flexors, the most important of which is the triceps surae. Synonym: extension of the ankle.
Plantar flexors
All muscles that perform plantar flexion in the ankle joint (more precisely: the ankle joints), i.e. increase the dorsal (back of the foot) angle of the foot to the lower leg. These are M. triceps surae, M. fibularis longus, M. fibularis brevis, M. flexor digitorum longus, M. tibialis posterior, M. plantaris
Plantar plate
The plantar plate is a 2-5 mm thickened capsule (fibrocartilaginous cartilage) under the metatarsophalangeal joints of the toes. Overuse can damage the plantar plate, especially when wearing shoes with little flexibility or walking barefoot on hard floors. High heels also put strain on the plantar plate because they can multiply the load on it. Another risk factor is a long 2nd ray. Cracks in the plantar plate can lead to metatarsalgia. Hammer toes and claw toes can develop later, possibly with dislocation in the metatarsophalangeal joint (MTP) and the development of metatarsophalangeal joint arthrosis/osteoarthritis.
PNS (peripheral nervous system)
see movement physiology – nervous system/PNS (peripheral nervous system).
polyarticular
see movement physiology – muscle/polyarticular.
Polydactyly / Polydactylia
Polydactyly refers to an upwardly deviating number of fingers or toes, i.e. more than 5 per hand or foot in humans. Digitus 1 or 5 is usually affected, which is double. Polydactyly is usually inherited. The supernumerary digits are not necessarily fully developed. Polydactyly also occurs as part of various syndromes. Its incidence is about 1:1300 in the northern hemisphere and 1:300 in Africa. About 40% are bilateral.
Portal vein
see movement physiology – circulation/Portal vein.
Post-load pulse
The post-load pulse is the pulse that occurs after a defined period of time after stress and is therefore equal to the stress pulse minus the recovery pulse.
Post-strain pain / post-exertional pain
see movement physiology – nervous system/post-strain pain.
Post-stress-induced pain
If an exertion pain does not subside immediately after the end of the exertion, this is referred to as post-exertion pain, also known colloquially as a „reverberation“ of the pain.
Posture
see movement physiology – posture.
Posterior
denotes a direction and means „from or to the rear“ and is identical to the term dorsal. The conceptual opposite is anterior, which in turn corresponds to the term frontal or ventral.
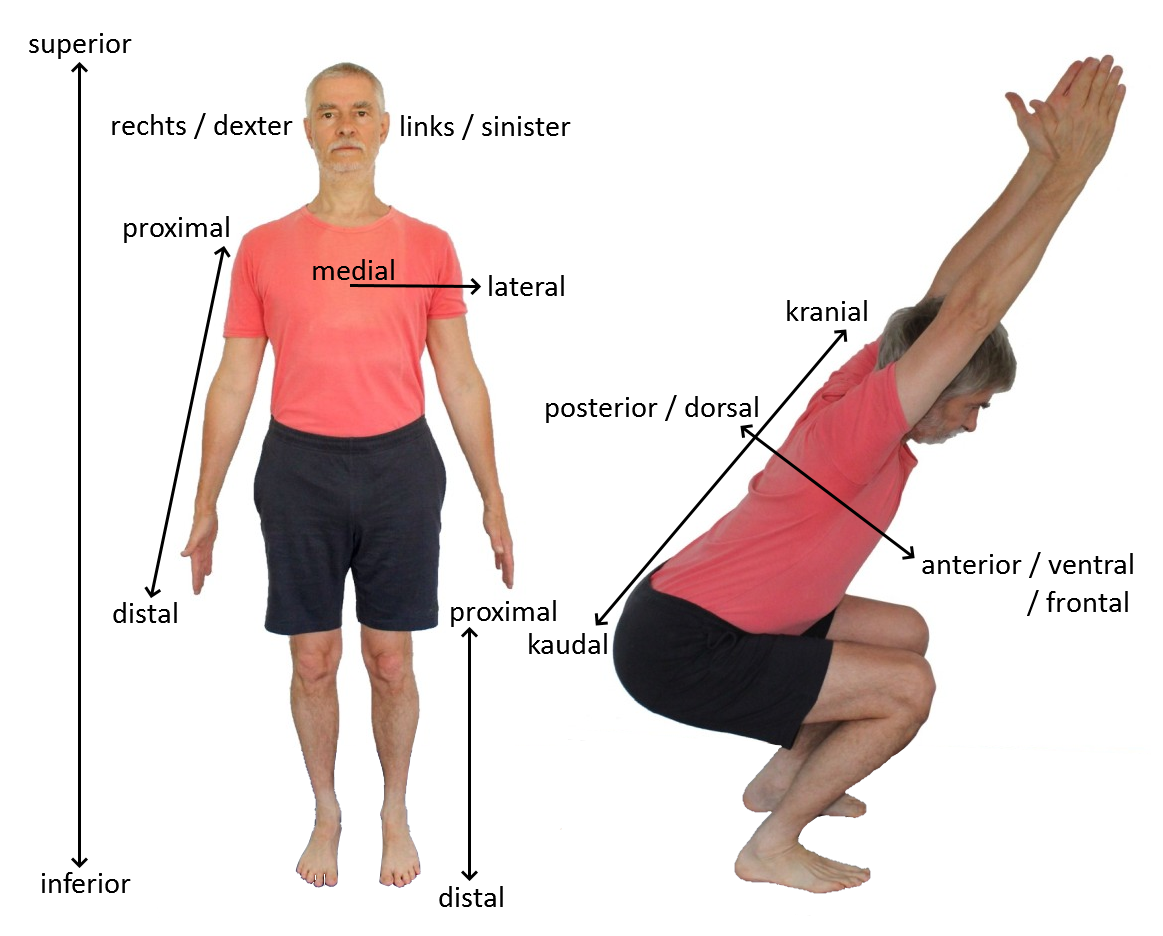
Posture
see movement physiology – posture.
Potential energy
The physical energy stored in the height of a body above the gravitational center of the gravitational source (in this case the earth), which begins to decrease when the body is released, as the body accelerates at 9.81 m/s² (in a vacuum) towards the center of the earth. If a body is moved further away from the center of the earth (i.e. upwards), this requires physical work and energy input.
Preactivation potentiation
see movement physiology – muscle/preactivation potentiation.
Prehabilitation
Prehabilitation refers to the personalised preoperative development of skills that precedes a more serious intervention such as an operation and improves the outcome or recovery time, for example. The approach to interventions on the musculoskeletal system is usually focussed on strengthening strength, mobility and aerobic endurance through exercise and sports therapy, and generally on aerobic endurance in particular. Prehabilitation is based on the realisation that a better pre-operative condition can reduce the complication rate (reductions of 30%-50% are being discussed) and reduce post-operative complaints, in some cases by half. Targeted prehabilitation is also expected to shorten the rehabilitation phase and reduce overall costs. Other important pillars of prehabilitation are
- A balanced diet rich in protein
- Improving psychosocial well-being and motivation
- Lifestyle-improving measures, including abstinence from alcohol and nicotine, minimisation of risk factors
Prehabilitation is usually started 4-8 weeks before the intervention. Although there are some promising studies on prehabilitation, this concept has not yet (2025) arrived in state healthcare. Nevertheless, it has found its way into the AWMF guideline on perioperative care.
Prestretching
see movement pyhsiology – muscle/prestretching.
Pressure
Pressure is force per area. If a person stands with both feet on the ground, the large effective partial body weight causes compression of the tissues under the foot bones, which we perceive as a very moderate level of pressure. If we only stand on the ball of the foot or the heel, the pressure (much smaller area with the same partial body weight) is significantly increased, which the pressoreceptors in the foot report to us as a subjectively higher pressure sensation. If we tried to stand on the extremely small area of a nail tip, the pressure would be so high that the skin would not be able to withstand it and the nail would dig into the foot and possibly even the ligaments between the bones of the foot would not be able to withstand the pressure. We see an important feature of pressure when we leave the realm of solid-state physics: Pascal’s principle. In liquids (at a certain level, i.e. a certain water column above it) and gases (here the level is practically irrelevant), the pressure is the same at every point of the same level and undirected, i.e. „the same in every direction“ at a certain point. This is important, for example, for understanding the sensations conveyed by the pressoreceptors, as well as for understanding the intervertebral discs of the spine and the related pathomechanisms.
Pressure pain / palpation pain
see movement physiology – nervous system/pressure pain.
Prevalence
Prevalence refers to the relative (or sometimes absolute) frequency of an entity (or generally: cases or events) in a group, usually the population of a country, at a fixed point in time, for example the number of people suffering from osteoarthritis of the knee in Germany at a fixed point in time.
Prevention
Prevention is the endeavour to prevent illness. In some areas, the term prophylaxis is used synonymously. Prevention attempts to eliminate known risk factors for the development of diseases or to prevent them from developing in the first place. Psychology, sociology and education all play a part in prevention. On the one hand, prevention serves to improve people’s quality of life; on the other hand, it is an economically important measure that seeks to avoid absenteeism and treatment costs, among other things. A distinction is made between 4 levels of prevention:
- Primordial prevention: Measures taken to combat risk factors for the development of a disease
- Primary prevention: measures taken to prevent the development of a disease, i.e. before the onset of the disease
- Secondary prevention: measures taken in the early stages of a disease to prevent progression or chronification. Some diseases are still asymptomatic at this stage
- Tertiary prevention: Measures taken after the manifestation of a disease or after treatment for this disease. The aim is to prevent secondary damage and recurrences
- Quaternary prevention: measures to prevent unnecessary or excessive medication
A further distinction is made between behavioural prevention and proportional prevention, i.e. measures that reduce the risk by improving individual behaviour and those that improve the conditions in which a person lives.
PRICE-scheme
The PRICE scheme is a set of instructions for immediate intervention in the event of various traumas or injuries, especially in the area of sports:
- P – Protection: from further injury
- R – Rest: relativ or absolute rest as needed for healing, depending on the case
- I – Ice – meaning to cool, minimize the swelling. Use cruched ice or cool water, preferably in cycles of up to 10 to 15 minutes
- C – Compression, to minimize swelling
- E – Elevation, to minimize swelling by keeping the affected limb raised over heart level, if possible for 24 to 48 hours
progressive
Progressive, advancing. Progressive refers to a disease or process that advances in scope or stage.
Progression
Progression, advancement, of a disease. There are several reasons for progression, one is simply a negative balance between healing and damage, as is often the case with osteoarthritis/arthrosis, in other cases, regeneration is no longer possible at all, for example in the case of osteoarthritis/arthrosis: the turn over of the damaged cartilage is beyond the lifespan. Diseases that progress are referred to as progressive.
Proliferation / to proliferate
Proliferation refers to the accelerated mitotic division of cells in response to biological needs such as trauma or inflammation. Proliferation is triggered and controlled by the hormone somatropin or by growth factors such as the proliferation cytokines IL-4, IL-7, and IL-15. The area in which proliferation takes place is referred to as the proliferation zone.
Pronation (foot)
in standard anatomical position, the tilting movement of the foot around its longitudinal axis, which is caused by the lowering of the inner foot in relation to the outer foot.
Due to the shape of the joint, pronation is always associated with a certain degree of abduction of the foot, i.e. a lateral movement.
Pronation (forearm)
the „rotation“ of the forearm: turning the radius over the ulna. In standard anatomical position the palm points backwards, i.e. away from the biceps, see below.
Pronation (arm)
the overcrossing movement of the forearm, in which the radius is turned away from its parallel course to the ulna towards crossing it. With the arm extended in front of the boxy turned out in the shoulder joint, this corresponds to a downward-facing palm. Pronation is possible up to approx. 180° with good flexibility from max. supination. With a pronated forearm the palm away from the biceps.
Pronators (foot)
All muscles that pronate the foot in the ankle joint (more precisely: almost exclusively in the subtalar joint), i.e. raise the lateral edge of the foot or lower the medial edge of the foot. These are M. fibularis longus, M. fibularis brevis, M. fibularis tertius, M. extensor digitorum longus.
Pronators (forearm)
All muscles that pronate the forearm, i.e. pronator quadratus, pronator teres, flexor carpi radialis, brachioradialis from a supinated position only and extensor carpi radialis longus (weak when the arm is flexed). See also the elbow joint.
Proprioception
see movement physiology – nervous system/proprioception.
Proprioceptors
see movement physiology – nervous system/proprioceptors.
Proprioceptive reflex
see movement physiology – nervous system/Proprioceptive reflex.
Protraction (shoulder blade)
Movement of the shoulder blade sideways and ventrally, i.e. away from the spine. The muscles performing this movement are the protractors. The opposite movement is called retraction.
Protractors (shoulder blade)
Muscles that move the shoulder blade away from the spine and ventrally, i.e. outwards and forwards, towards the sternum:
proximal
refers to a position in an extremity close to or (in comparison) closer to its attachment to the trunk. The conceptual opposite is
distal.
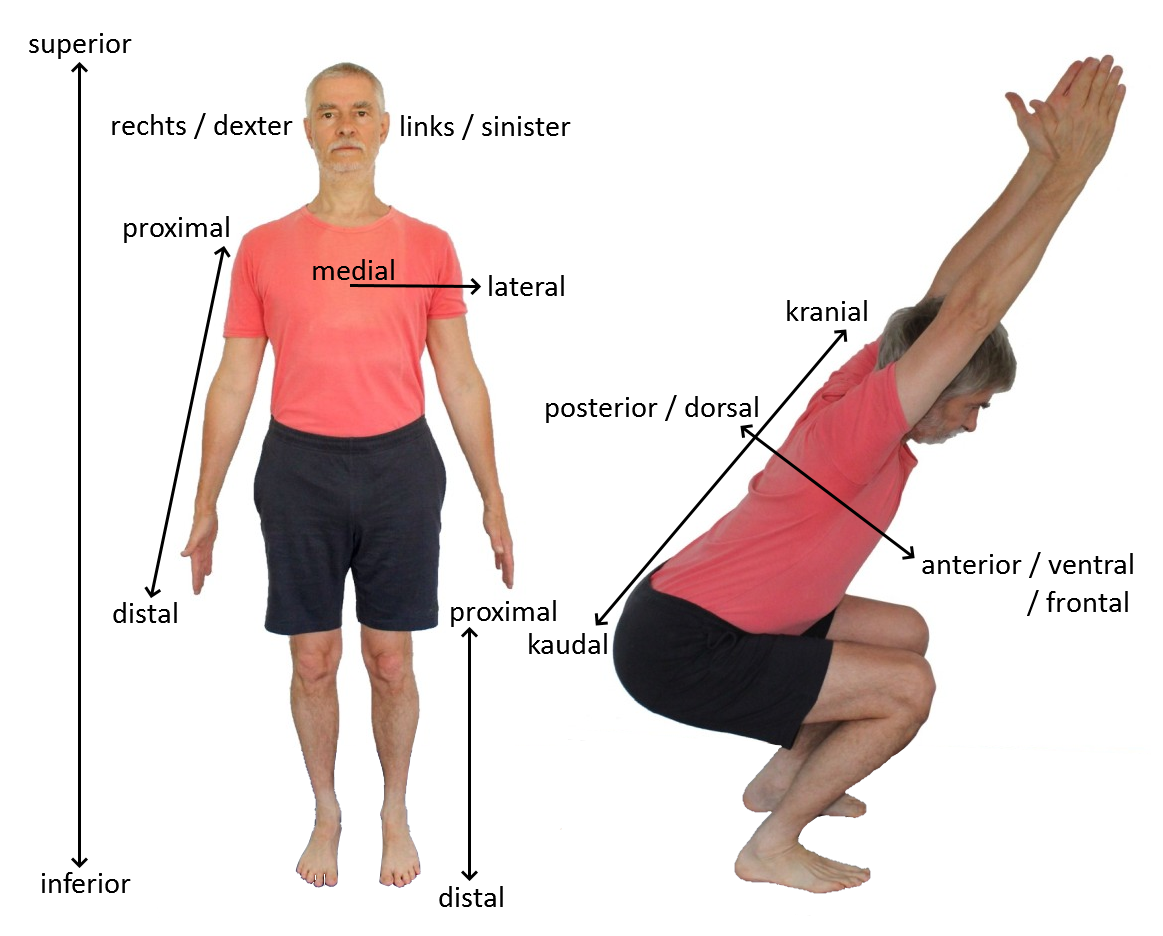
Pulley-complex
The pulley complex is the structure that holds the long biceps tendon in its course before it enters the sulcus intertubercularis (sulcus bicipitalis). This is formed from supraspinatus, subscapularis, supperior coracohumerale ligament and superior glenohumeral ligament. Damage to the pulley complex is referred to as a pulley lesion.
pulmonary circulation
see movement physiology – circulation/pulmonary circulation.
Pulse
see movement physiology – circulation/pulse.
Pulse deficit
see movement physiology – pulse deficit.
pulse-synchronous pain
see movement physiology – nervous system/pulse-synchronous pain.
Pulse Wave Velocity PWV
see movement physiolgy – circulation/Pulse Wave Velocity.
Punctum fixum
The punctum fixum is the part of the body that is fixed during a movement (e.g. standing on the floor). The opposite is the punctum mobile. Which part remains stationary and which part is moved depends on these two. Examples
- In uttanasana the legs are punctum fixum with regard to the work of the hip flexors, the pelvis with the upper body is moved.
- In parivrtta trikonasana the lower arm is punctum fixum with regard to the lateral adduction and retroversion in the shoulder joint
- In upface dog with stretched feet the arms are punctum fixum when the frontal adduction in the shoulder joint pulls the upper body and with it the pelvis forward.
The usual anatomical view of the attachment and origin of a muscle suggests that the more central origin is the fixed point from which the attachment is drawn. This assumption, which is often incorrect in sports science, is generalized by considering the moving part punctum mobile and the fixed part punctum fixum, even if this model is not yet general enough, as shown by poses such as navasana, in which the hip flexors bring the thighs and pelvis with the upper body halfway evenly closer together. Another counter-example is the downface dog, in which the deltoids mainly push the shoulder area towards the feet through their frontal abduction in the shoulder joint. Here too, neither the arms nor the upper body can be regarded as a puntum fixum, as the force applied moves both.
Punctum mobile
The relevant counterpart to the punctum fixum, see the derivation of the concept there. A moving part of the body is referred to as a punctum mobile when a muscle connected to it, whose origin or attachment is in the punctum fixum, exerts force on it.
Pyramidal tract
see movement physiology – nervous system/pyramidal tract.
Pyramidal sign
see movement physiology – nervous system/pyramidal sign.
Q
R
Racket sports (racket sports)
see movement-physiology – racket sports
Radial abduction (hand)
Swiveling the hand radially, i.e., radial abduction, in other words: reducing the distance and angle between the thumb side of the hand or the metacarpal bone 1 and the radius.
Radial adduction (hand)
Returning a radial abduction to the zero position, i.e., increasing the distance and angle of the
thumb side of the hand or the metacarpal bone 1 to the radius (spoke).
Range of motion ROM
see movement physiology – ROM.
Ray
The entirety of all phalanges of a finger or toe with its associated metacarpal or metatarsal bone.
Regeneration
see movement physiology – regeneration.
Reclination (neck)
Tilting of the head backwards towards the back, the term is synonymous with extension of the cervical spine.
Rectus sheath
The aponeurosis, which envelops the rectus abdominis superficially and profoundly. It emerges laterally from the tendons of the oblique abdominal muscles and the transversus abdominis and forms the linea alba between the two sides of the rectus abdominis. The anterior wall of the rectus sheath (lamina anterior) extends to the pubic bone, but the posterior wall ends at the linea acuata.
Recurrence
Recurrence of disease activity of a chronic relapsing disease.
Reflex
see movement physiology – nervous system/reflex.
Regeneration
see movement physiology – regeneration.
Rehabilitation
Rehabilitation generally means the restoration of physical or mental health. In particular, rehabilitation refers to those measures that go beyond the curative measures prescribed or carried out by a doctor and are carried out after these. Measures that are carried out before treatment in order to achieve a better outcome from the intervention are referred to as prehabilitation. An important aspect of rehabilitation is the complete or best possible restoration of full earning capacity and the avoidance of the need for care. There are various professional groups for rehabilitation measures, from occupational therapists to occupational therapists, physiotherapists and sports therapists. There are now rehabilitation protocols for many disorders, such as those published by Massachusetts General Hospital: https://www.massgeneral.org/orthopaedics/sports-medicine/physical-therapy/sports-rehab-protocols or the Royal National Orthopaedic Hospital.
Rein system
see movement physiology – rein system.
Remission
Partial abatement or complete cessation of disease activity and the associated symptoms of a chronic disease, without permanent damage that has already been acquired being reversed. Remission is therefore the opposite of relapse and, in the case of chronic progressive diseases, also excludes progression. Remission is therefore not a cure (restitutio ad integrum) but a resting phase of the disease activity.
Repetition
Term for a complete movement cycle of a cyclical movement that is not performed in a highly repetitive manner, such as running, but is performed in a much lower number of repetitions, such as in strength training. A sequence of repetitions performed without interruption is referred to as a set.
Repositionable / Resettable / Reducable
The ability of a malposition or incorrect position to be corrected (usually externally). This is generally understood to mean the ability of the malpositioned body part(s) to be brought into the correct position through manual intervention by the person themselves or an examiner (the process is called reduction). Anything that can be repositioned or repositions spontaneously is, by definition, reducable. For example, an acquired foot deformity that is not very old may be reducible, but may lose this property over time due to an accumulation of secondary changes in the foot. In many cases, repositionable deformities have a chance of conservative treatment success, whereas the opposite, contracted deformities, generally do not.
Repositioning / Resetting / Reduction
To bring back into the physiological position. The term refers to anything that can leave its physiological position and become malpositioned, bones in joints, organs, fracture ends in the case of a fracture.
Reserve extensor apparatus (of the knee joint)
The structures that maintain a residual stretching ability of the knee joint are referred to as the reserve extensor apparatus, if the patella is fractured, the lig. patellae is torn from the tuberositas tibiae, or the quadriceps tendon is torn from the patella, see knee joint/restorative extensor apparatus.
Residual volume
see movement physiology – circulation/residual volume.
Respiration / breathing
see movement physiology – circulation/respiration.
Respiratory muscles
see movement physiology – circulation/respiratory muscles.
neutral respiratory position
see movement physiology – circulation/neutral respiratory position.
respiratory volumes
see movement physiology – circulation/respiratory volumes.
Restriction of motion (of flexibility)
Restriction of flexibility refers to any lower ROM in a joint in one physiological dimension of movement or in a combined direction of dimensions than is given by the physiological hard-elastic or firm-elastic limit of movement, regardless of the cause. Restrictions in flexibility should therefore not be confused with physiological movement limits. In practice, almost all movements have a soft-elastic, muscular limit of movement. One well-known exception is the extension of the middle joints of the extremities, which, depending on the exact geometric configuration of the joints and the flexibility of the overlying biarticular muscles, are predominantly limited by hard-elastic (elbow joint) or firm-elastic (knee joint) limits: if, for example, asumed there is no soft-elastic limit of movement in the knee joint for extension without or with only slight hip flexion, this changes with further flexion in the hip joint when a soft-elastic limit of movement arises due to the restriction of flexibility of the hamstrings.
The term restriction of flexibility refers to a dimension of movement or a direction of movement that is a combination of movement dimensions. In practice, most flexibility restrictions are acquired losses of muscular flexibility, which are mainly due to regular non-utilization of parts of the ROM that is basically possible according to the hard-elastic and fixed-elastic movement limits and the corresponding adaptation of the muscles. See also the corresponding graph for the ankle joint, which shows the statistical decrease in flexibility in the ankle joint in the two movement dimensions of plantar flexion / dorsiflexion and pronation / supination.
The remaining range of motion (also: „range of motion“) must be determined actively and passively, as the two can differ: in the event of a rupture of the only executing tendon (e.g. quadriceps tendon for knee extension), the corresponding movement (in this case knee extension) can no longer be performed actively, but can be performed by an examiner, i.e. it is greater passively than actively.
Another example is the flexion of the knee joint, which its flexors can perform up to approx. 150 before active insufficiency or passive insufficiency occurs. The examiner, on the other hand, can usually bend the knee joint noticeably further.
The range of motion of most joints can be represented as one-, two- or three-dimensional with a corresponding number of independent movement dimensions. In practice, the movements in the central area of the ROM are independent without any restriction, but towards the edges of the ROM the course of the muscles and their restricted flexibility often have an effect on another dimension when one movement in a special dimension is intended, so that independence appears to be disturbed.
Resting Heart rate
see movement physiology – resting Heart rate.
Restrictive
see movement physiology – circulation/restriktive.
Retinaculum
Restraining ligament that holds tendons in an area close to the joint and prevents the tendons and the associated muscles from fulfilling their physical tendency to stretch from origin to attachment by the shortest route when contracting, which in the case of the superficial finger flexors and profound finger flexors originating from the medial epicondyle of the humerus, for example, would be extremely obstructive in many tasks, would make them extremely susceptible to injury and would certainly have had at least a massive negative impact on the development of the species.
Retraction (shoulder blade)
Retraction of the shoulder blade towards the spine. The muscles that cause this are the retractor muscles. The counter-movement is called protraction.
Retractors (shoulder blade)
Muscles that pull the shoulder blade dorsally and medially towards the spine. These are
The rhomboids also cancel out the outward rotation of the shoulder blade.
Retroversion (arm / shoulder joint)
Movement of the arm in the glenohumeral joint in a dorsal direction, i.e. beyond standard anatomical position. Retroversion can also be referred to as dorsal abduction in the shoulder joint and as a continuation of frontal adduction in the shoulder joint. The countermovement ist called canceling out the retroversion or dorsal adduction.
Retroverters (arm / shoulder joint)
the muscles that perform retroversion in the shoulder joint: teres major, latissimus dorsi (to a certain point only), triceps (caput longum), deltoid (pars spinalis, pars acromialis partial).
Rhomboids
important retractors of the shoulder blade, see M. rhomboideus minor and M. rhomboideus major.
ROM (Range of motion)
see movement physiology – ROM.
Rotary joint / pivot joint / trochoid joint
see movement physiology – joint shapes/rotary joint
Rotation (head)
Rotation of the head around its longitudinal axis (in standard anatomical position: to the left or right), see also: rotation of the spine.
Rotation (shoulder blade)
Movement of the scapula in the plane in which it mainly expands, i.e. with the inferior angulus (lower tip) outwards and upwards (called outward rotation) or back again inwards and downwards (called inward rotation). The rotation of the angulus inferior outwards and upwards (outward rotation) is a prerequisite for raising the arm above 90°
Rotation (spine)
Rotation of parts of the spine around its longitudinal axis. The individual vertebral segments, consisting of two adjacent vertebrae and the intervertebral disc between them (as well as the spanning muscles and ligaments), allow the upper vertebral body to rotate to varying degrees in relation to the lower vertebral body. This is typically caused by the autochthonous back muscles, by other trunk muscles such as the oblique abdominal muscles, or by forces acting on the trunk via the extremities. Within the autochthonous back muscles, the oblique system causes rotation, which simultaneously generates extensor moments as well as rotational moments. In addition to extension/flexion and lateral flexion, rotation is one of the three dimensions of spinal flexibility and, like the other two, only occurs in large areas, essentially the cervical spine, the thoracic spine or the lumbar spine or more than one of them at a time.
Rotation axis / axis of rotation
the axis around which a one-dimensional movement takes place. This is, for example, a line through a condyle of a moving bone. If the elbow joint is considered only in terms of the humeroulnar joint (the joint between the humerus and ulna: articulatio humeroulnaris), it is a pure hinge joint in which the forearm rotates about an axis across the ulna forearm bone between the shaft and olecranon, thus enabling flexion and extension of the elbow joint. If the range of motion is more than one-dimensional, there is a center of rotation.
Rotation center / center of rotation
the point around which a multidimensional movement takes place. This is usually a point in a condyle of a moving bone. If the acetabulum is idealized as part of a spherical surface, it is the center of the sphere in which the three-dimensional movement in the hip joint takes place: abduction/adduction, flexion/extension and exorotation/endorotation. If only a one-dimensional movement takes place, this is referred to as an axis of rotation.
Rotational torque
Torque acting on a joint in the direction of rotation.
Rotator cuff
Term for a group of muscles, including:
- Teres minor (external rotator and adductor)
- Supraspinatus (external rotator and initial lateral abductor)
- Infraspinatus (strongest external rotator)
- Subscapularis (adductor muscle and most important internal rotator)
Together with the coracohumeral ligament, they form a tendon cap around the humeral head and the glenohumeral joint. Together they fix the humeral head in the glenoid. Some authors consider the term to be outdated.
The following image shows the attachments of the four muscles at the humeral head.
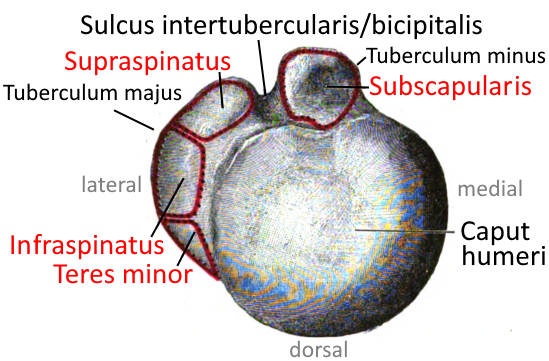
Rearfoot running (heel running)
The most common running style in recreational sports and over long distances. The foot touches down with the heel, with the touchdown point clearly in front of the body’s center of gravity. On landing, the knee must be slightly bent in order to absorb the impact muscularly. In the standing leg phase, the knee joint is bent by up to 40° and the pelvis tilts forward significantly, especially if the gluteal muscles are weaker. In the push-off phase, the hip joint is only extended to around 0°, meaning that the leg is just in extension of the upper body. The pelvis remains more or less tilted forward.
Advantages: easy to learn as it is easier to derive from your usual walking, less effort required than forefoot running. Rearfoot running is easy to learn, reasonably energy-efficient, although not as much as forefoot running and not as demanding in terms of coordination.
Disadvantages: higher joint stress (ankle, knee joint, hip joint) when landing than with forefoot running, deceleration of propulsion on landing with loss of energy, tendency to Achillodynia, heel spurs, greater tendency to meniscus damage (outer menisci with knock knees, inner menisci with bow legs ), greater tendency to patellar lateralization. However, the effect of the impact is actually less than often assumed in the past. More recent findings show that the foot adapts to the running technique and the hardness of the surface.
Resting heart rate / Resting heart rate / Resting heart rate
see movement physiology – resting heart rate.
Rotary joint / pivot joint / trochoid joint
see movement physiology – joint shapes/pivot joint.
Rowing
see movement physiology – rowing.
Running
see movement physiology – running.
S
Sacrospinal system
the muscles that run between the iliac crest and spinous processes of the vertebrae and belong to the lateral tract of the autochthonous back muscles: longissimus: (thoracis, cervicis, capitis) and iliocostales (lumborum, thoracis, cervicis), which, unilaterally innervated, flex the spine laterally and extend it innervated on both sides.
Saddle joint
see movement physiology – joint shapes/saddle joint.
Sagittal
Direction from anterior to posterior, i.e. vertically, in a vertical plane through a person standing in standard anatomical position, i.e. the plane in which an arrow shot at the person from the front flies. See also sagittal plane.
Sagittal plane
A vertical plane through a person standing in standard anatomical position from ventral to dorsal, i.e. – eponymously – the plane in which an arrow shot at the person from the front flies. The central sagittal plane through the symphysis, linea alba, midline of the sternum and the nose is called median plane.
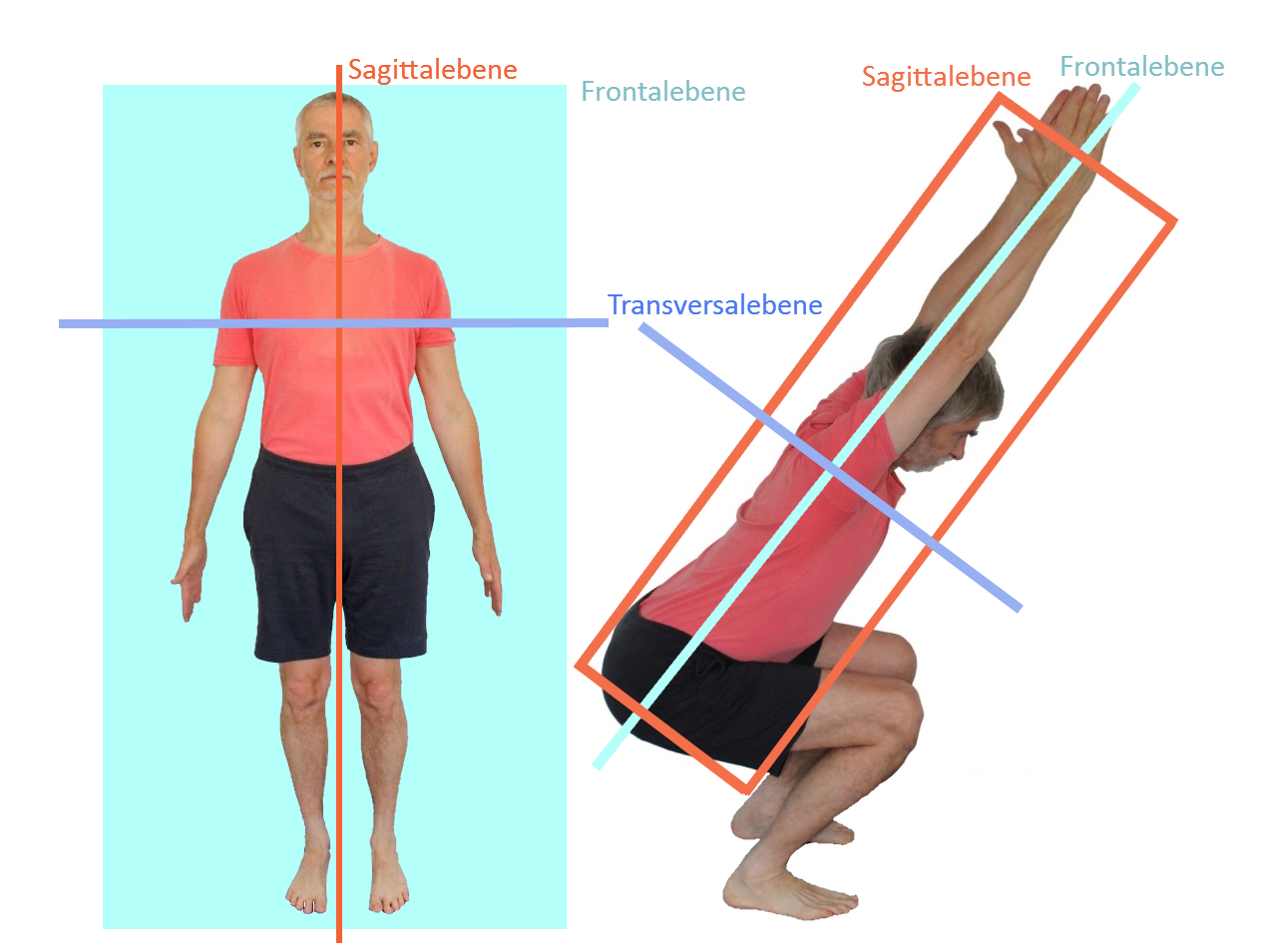
Sarcomere
see movement physiology – muscle/sarcomere.
Sarcomere length
see movement physiology – muscle/sarcomere length.
Sarcopenia
see movement physiology – muscle/sarcopenia.
Inclined system
the part of the autochthonous back musculature that laterally flexes the spine, a list can be found there.
Scalable
scalable means adaptable to requirements, variable, without having to make categorical changes. A simple example is the combustion engine as a heat engine. If more power is required, e.g. for greater acceleration or a higher speed (the nesessary work increases disproportionately against the air resistance with velocity), it is sufficient (simplified) to supply it with more fuel (air mixture) to a corresponding, but not necessarily exactly proportional extent. This is only natural, as power over a fixed time is equivalent to the energy content of the fuel used. In yoga poses, many factors are not scalable if the effect is based purely on the gravitational force of a partial body weight. For example, the degree of contraction of the deltoid in warrior 2 pose (if there are no lateral adductors of the shoulder joint in action) is mainly dependent on its maximum force and the gravity of the arm itself, and of course also on its length in the sense of the lever law. The stretching effect in the hamstrings in uttanasana is also not scalable if neither the lower legs are pulled with the arms nor the hip flexors are used to promote hip flexion beyond the degree induced by the partial body weight. If, on the other hand, one of these methods is used in addition, the pose is generally well scalable. In the same way, the strengthening of the pectoralis major and triceps related to a fixed time interval in staff pose is restricted for a given position of the hands because the partial body weight held is not variable but fixed. The staff pose only becomes scalable by changing the duration or the lever arm at which the muscles mentioned have to hold the upper body, i.e. when the hands are placed closer to the pelvis.
scalene gap / posterior scalene gap
If the term scalene gap is used without a suffix, it usually refers to the posterior scalene gap, the passage between the first rib, scalenus anterior and scalenus medius. The passage between scalenus anterior and sternocleidomastoid is referred to as the anterior scalene gap, through which the V.
The posterior scalene gap is an important passageway for blood vessels and nerves, especially the nerves of the brachial plexus and the subclavian artery. An inconstant scalenus minimus may divide the scalene gap again. A narrowing of the scalene gap can lead to thoracic outlet syndrome.
Scalene gap, anterior
The passage between scalenus anterior and sternocleidomastoid is known as the anterior scalene gap. The subclavian vein runs through it. If the term scalene gap is used without the adjective „anterior“, it generally refers to the posterior scalene gap.
Segment (spinal column)
Two vertebrae with the intervertebral discs in between and the connecting ligaments. The segment is the unit in which the movements take place and therefore corresponds to a „vertebral joint“.
Segment indicating muscle
see movement physiology – nervous system/segment indicating muscle.
Sensitivity
The sensitivity of a test refers to the probability that patients are recognised as such by this test. A low sensitivity therefore means a high false negative rate.
Sesamoid bone
A small bone embedded in or superimposed on a tendon to protect the tendon or underlying structure or to increase the lever arm of the tendon so that the executing muscle can achieve a greater moment. The sesamoid bone is therefore a hypomochlion.
Set
A sequence of repetitions performed essentially without interruption. Usually several sets are performed in succession in training sessions, often with increasing resistance (such as a weight) and decreasing numbers of repetitions. Depending on the ambition and level of training, it is not uncommon to end up with sets with only around 4 repetitions, which already corresponds to around 89% of the 1RM.
Shoulder girdle
The shoulder girdle consists bony of the two scapulae and the two clavicles, which are connected ventrally to the sternum, which is not part of the shoulder girdle. In contrast to the closed pelvic girdle, the shoulder girdle is open dorsally. The musculature of the shoulder area consists of four groups:
- scapulohumeral muscles: supraspinatus, infraspinatus, teres major, teres minor, triceps (caput longum), biceps, subscapularis, deltoids, coracobrachialis
- truncohomeral muscles: pectoralis major, latissimus dorsi
- truncoscapular muscles: rhomboid major, rhomboid minor, levator scapulae, pectoralis minor, serratus anterior, subclavius, trapezius
- craniozingular muscles: sternocleidomastoideus
Shrug
Shrugging is the colloquial term for moving the shoulder blades, including the arms attached to them, upwards, i.e. cranially. Anatomically, this corresponds to their elevation and is achieved, among other things, by the contraction of the trapezius (pars descendens) and the levator scapulae. In everyday life, the arms usually rest against the body. In yoga poses, elevation, i.e. „the state of the shrugged shoulders“, is often found in poses with 180° frontal abduction in the shoulder joints (glenohumeral joints) such as downface head or handstand.
Sick scapula / scapula dyskinesia
see movement physiology/scapula dyskinesia.
Side discrepance / inequality
As a rule, a side discrepance refers to a muscular imbalance in which one or often consecutively several muscles contralaterally have a different tone (and often also a different flexibility) than ipsilaterally. side discrepancies are therefore more or less pathogenic, depending on the extent and the muscles affected. For example, a side discrepance in the hip flexors and hip extensors can result in pelvic torsion and a consecutive disorder of the SI joint, or a lateral difference in the adductors and abductors of the hip joint can result in pelvic obliquity and a consecutive scoliosis. The extent of the disorder depends on many factors, including on the one hand the extent of the side discrepance, but on the other hand also the level of flexibility at which it occurs and thus also the extent of the influence on daily posts held for longer periods.
Side-by-side comparison
In some situations, due to the individual fluctuation of the parameters of the musculoskeletal system, a comparison between the two sides of the body is much more meaningful than a comparison of this parameter with other people or with a reference range to be read off. In particular, side discrepancies, even if the values on both sides lie within a reference range, tend to have an effect in other areas of the body and cause consequences there, and are often pathogenic.
Sitting giant
A sitting giant is a person whose upper body is particularly long compared to their legs. In most cases, the other limb is also longer in relation to the upper body: the arms. The arm-upper body ratio can be tested very easily: if the wrists are clearly above or at the greater trochanter of the femur in standard anatomical position, we see a sitting giant and wrists significantly below the greater trochanter, we see normal proportions or even a sitting dwarf. See also the exploration: sitting giant.
Sitting dwarf
The opposite of a seating giant, see there.
Scapulohumeral muscles
Muscles that pull from the shoulder blade (scapula) to the upper arm bone (humerus) to move the arm:
- Supraspinatus
- Infraspinatus
- Teres major
- Teres minor
- Trizeps (Caput longum)
- Bizeps
- Subscapularis
- Deltoideus
- Coracobrachialis
sciatic nerve
see movement physiology – nervous system/sciatic nerve.
smooth musculature
see movement physiology – muscle/smooth musculature.
SNS (somatisches Nervensystem)
see movement physiology – nervous system/SNS (somatic nervous system).
Soft-elastic
see movement physiology – joint/soft-elastic.
Sore muscles
see movement physiology – muscle/sore muscles.
Specificity
The specificity of a test refers to the probability that healthy people who do not suffer from the disease being tested for will actually have a negative test result. A low specificity therefore means a high false positive rate.
Spheroidal joint
see movement physiology – joint types/spheroidal joint.
Spinal canal
see movement physiology – nervous system/spinal canal.
Spinal marrow
see movement physiology – nervous system/spinal marrow.
Spinalnerv
see movement physiology – nervous system/spinal nerve.
Spinotransversal system
the muscles belonging to the lateral tract of the autochthonous back muscles that run between the spinous processes and the transverse processes of various vertebrae further cranially: splenius with cervicis and capitis parts, which rotate the cervical spine innervated on one side and lateral flex it innervated on both sides.
Spondylodesis
Arthrodesis of one or more segments of the spine.
Spondylophyte
Osteophyte occurring at the vertebrae, i.e. at the facet joints or at the edges of the upper and lower plates of the vertebral bodies.
Spondylosis
Formation of osteophytes on the facet joints of the spine (spondylophytes). Spondylophytes and osteophytes in general are sometimes interpreted as an attempt by the body to enlarge the joint surface and thus relieve osteoarthritic/arthrotic or chondrotic areas. Atiologically, however, it is simply a matter of cartilage material being moved out of the contact surfaces of the joint and calcified there.
Spongy bone / trabecular bone
see movement physiology – bone/spongy bone.
Sport in growth
see movenet physiology – sport in growth
Sprinting
see movement physiology – sprinting.
Standard anatomical position
Upright posture in which the feet are parallel and closed, the knees are stretched, the pelvis is upright, the upper body including the cervical spine is stretched and the arms rest against the body in such a way that the inner elbows and palms – in contrast to Neutral zero – point forwards. This means that Standard anatomical position corresponds approximately (!) to a savasana tilted 90° upright. Standard anatomical position is likely to have originated from the position in which most dissections were (and still are) performed in medical history in order to explore the human body.
Standing leg
The term standing leg refers to the one of the two legs that carries the body weight alone or carries a larger part of the body weight. The other leg is referred to as the free leg. This definition shows that the transition of a leg from the status of the standing leg to the status of the free leg can be fluid. In sports with a flight phase, such as running, no smooth transition is possible, but the standing leg and free leg alternate constantly (cyclical movement). Depending on the movement sequence, the standing leg not only carries the partial body weight (in this case the entire body weight minus that of the leg) but also kinetic (dynamic) loads, which can be many times the body weight, for example when landing from a jump, up to 7 times the body weight, for example in a block jump in volleyball.
Start-up pain (running-in pain, starting pain)
Pain that occurs at the start of an activity, movement or task and subsides as it progresses. This type of pain is typical of osteoarthritis/arthrosis and arthritis, but also other degenerative joint changes, especially in the hip joint and knee joint. In the case of osteoarthritis/arthrosis, the disease progresses over the years and the initial start-up pain often turns into continuous pain on exertion and later also pain at rest. In osteoarthritis/arthrosis, both are particularly pronounced in arthritic episodes.
Steep position
A steep position is usually defined as the loss of the physiological lordosis of the lumbar or cervical spine or the loss of the physiological kyphosis of the thoracic spine with transition of that area to a flat position. The steep position results in a change in the statics and the loss of the spring function of the area. The body must counteract the altered statics with compensation in distal and/or proximal areas so that the center of gravity of the partial body weight of the upper body, head and arms does not change too much, which would lead to a permanently increased muscular demand on the postural apparatus. In addition, the term steep position is also used for other parts of the musculoskeletal system that are physiologically inclined at a certain angle to the longitudinal axis of the body, such as the tarsal bones or the sacrum.
Strength and conditional training
Strength and conditional training, not to be confused with athletic training, is not yet a recognised term in international sports science. Strength and conditional training is usually understood to mean accompanying training for athletes that cannot be categorised as sport-specific training such as technique training or coordination training. As Strength and conditional training geared towards a specific sport, it contains a different composition of core athletic components for each sport and should also take into account the specific weaknesses of the athletes, i.e. be individualised. This is where Strength and conditional training can overlap with rehabilitation after injuries. Strength and conditional training includes strength training in the three areas of maximum strength training, strength endurance training, speed strength training, and possibly also hypertrophy training, as well as coordination training, endurance training and mobility training. This definition therefore contains exactly the components of the classic definition of fitness. Strength and conditional training not only increases the performance of athletes in a way that would not be possible with purely sport-specific training, it can also reduce the risk and severity of side effects of the sport and sport-specific injuries. On the one hand, athletic training could help to reduce the risk of sports injuries, but on the other hand, the sport will usually only minimise its side effects at a higher performance level due to the athlete’s increased performance.
Sport-specific strength and conditional training has become an integral part of professional sport and the higher amateur leagues, but is also firmly established among many ambitious recreational athletes.
In addition to sport-specific strength and conditional training, there is also general strength and conditional training, which does not prepare athletes for a specific sport or support their performance, but rather puts the athlete in a generally good state of performance that would enable them to achieve a respectable performance when learning a sport, similar to what is experienced in professional sport when switching between two sports. Some authors also refer to general strength and conditional training as functional training.
Strength endurance
see movement physiology – muscle/strength endurance.
Stretching
see movement physiology – muscle/stretching.
Stretching pain
See movement physiology – nervous system/stretching sensation.
Stretching painfulness
See movement physiology – nervous system/stretching painfulness.
Stress-induced pain
see movement physiology – nervous system/stress induced pain.
Stress-induced painfulness
see movement physiology – nervous system/stress-induced painfulness.
striated muscles
see movement physiology – muscle/striated muscles.
Stroke volume
see movement physiology – circulation/stroke volume.
structural pain
see movement physiology – nervous system/structural pain.
Suboccipital system
the muscles running from the vertebrae to the occiput:
- M. rectus capitis posterior major
- M. rectus capitis posterior minor
- M. obliquus capitis inferior
- M. obliquus capitis superior
Support base (physical support base, also: PSB)
Convex envelope of the set of load-bearing points of a body in the plane, regardless of whether the plane is horizontal. In the case of a square table, this is the smallest rectangle that encloses the table leg contact surfaces with the floor.
Supercompensation
see movement physiology – muscle/supercompensation.
Superior
refers to a position close or (in comparison) closer to the head. The conceptual opposite is inferior.
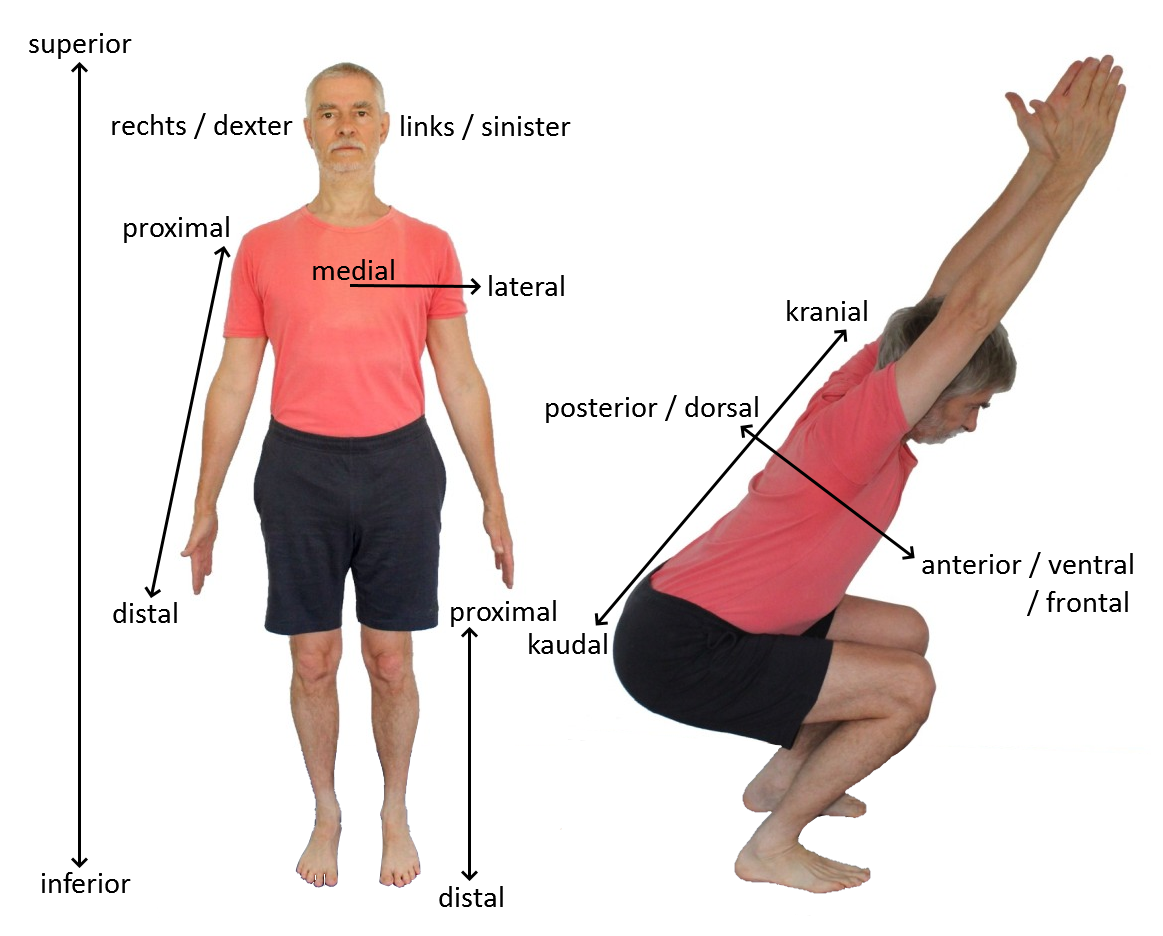
Supination (foot)
in standard anatomical position, the tilting movement of the foot around its longitudinal axis (in the sublatar joint), which is caused by lifting the inner foot in relation to the outer foot.
Die Supination ist wegen der Form des Gelenks immer mit einem gewissen Maß an Adduktion des Fußes verbunden, also einer Bewegung nach medial.
Supination (forearm)
the rotational movement (reversal of the overturning movement) of the radius over the ulna, which brings the two forearm bones (ulna and radius) closer to their parallel course as it corresponds to standard anatomical position with the palms facing forwards. With the arm extended forwards and turned out at the shoulder joint, this corresponds to an upward-facing palm, in other terms, with a bent arm, the palm point towards the biceps.
Supinators (foot)
All muscles that supinate the foot, i.e. lift the medial edge of the foot. These are: M. triceps surae, M. tibialis posterior, M. flexor digitorum longus, M. flexor hallucis longus, M. tibialis anterior.
Supinators (forearm)
All muscles that supinate the forearm, i.e. the biceps, which supinates the forearm a little from a pronated position, the brachioradialis, supinator, extensor carpi radialis longus, extensor pollicis longus, extensor pollicis brevis, extensor indicis. See also: elbow joint.
Survival Time
Survival time indicates how long a person survives on average after an intervention. It is therefore a kind of reversal of all-cause mortality, applied to a treatment option. In principle, survival time can also be specified for a certain age, without any intervention. However, it is usually used to evaluate treatment options or compare treatment methods.
Swelling of the lymph nodes
see movement physiology – circulation/swelling of the lymph nodes.
Swimming
see movement physiology – swimming.
Sympathetic nervous system / sympathetic / sympathicotone
see movement physiology – nervous system/sympathetic nervous system.
Symphysis (pubic symphysis)
The pubic symphysis (symphysis pubica) between the left and right pubic bone. It plays a role during pregnancy because it widens under hormonal control, see also symphysis. The small movements possible here also play a role in many movements.
Symphysis (in general)
Symphyses in the actual sense are connections of bones through fibrocartilage, and therefore belong to the articulationes cartilagineae like the synchondroses. The best-known symphysis is the pubic symphysis (symphysis pubica) between the left and right pubic bone. An intervertebral disc (interpubic disc) lies in the symphysis, which keeps the joint mobile. This flexibility can be felt in various poses and used as a marginal effect, for example by stretching in the ischial joint in forward bends. The connection between two vertebrae (intervertebral symphysis) is also a symphysis. The connected bones form a symphysis with the intervertebral discs (and accompanying ligaments).
Synapse
see movement physiology – nervous system/synapse.
Synchondrosis
A synchondrosis is a cartilaginous connection between two bones. It is therefore not a true joint but belongs to the articulationes cartilagineae. Normally, hyaline cartilage connects the bones. If it is fibrocartilage instead, it is referred to as a symphysis. Examples include the cartilage between ribs 1, 6 and 7 and the sternum (synchondroses costosternales), between the sphenoid bone and the occipital bone (synchondrosis sphenooccipitalis) or between the sphenoid bone and the petrous bone (synchondrosis sphenopetrosa). The cartilage connection between the three parts of the sternum (synchondroses sternales) are symphyses.
Syndactyly
Syndactyly refers to the adhesion of fingers or toes. This can occur as simple syndactyly if the two digits are only connected by soft tissue. If the digits are connected by bone, this is known as complex syndactyly. This can be partial or complete, i.e. only proximal phalanges or all phalanges can be affected. Syndactyly also occurs as part of various syndromes. It is genetically determined or caused by alcohol consumption during pregnancy.
Syndesmosis
A syndesmosis is a connective tissue (collagen or elastic) connection between two bones. It is therefore not a true joint, but belongs to the articulationes fibrosae. The connecting membrane is usually also the attachment area for muscles. In contrast to the synchondroses, which are mainly subjected to pressure, syndesmoses are mainly subjected to tension. The presence of syndesmoses does not mean that the articulating bones have no real joints with each other. Important counterexamples are the syndesmoses between the ulna and radius (interosseous membrane antebrachii) or between the tibia and fibula (interosseous membrane cruris).
Synergist
most often: muscular co-actor that (at least partially) performs the same movement, i.e. supports the agonist. In many cases, muscles are only partially synergistic because most muscles serve several dimensions of movement simultaneously. The term is also used in other fields such as neurology or endocrinology for nerves or substances that have a reinforcing effect.
Synovia
Synovia refers to both the joint fluid, which contains the nutrients required by the cartilage coverings of the bones and to which the cartilage releases the metabolic end products under pressure, and the innermost layer of the joint capsule, which produces this fluid. The fluid is also commonly referred to as „synovial fluid“. In terms of low-molecular substances (less than 100,000 Daltons), the joint fluid is largely a dialysate of the blood serum, but has a different protein composition, for example the coagulation factors prothrombin, proaccelerin, proconvertin and fibrinogen are missing, so it is not capable of clotting. Physiologically, it contains hardly any blood cells, mainly lymphocytes. In addition to hyaluronic acid, fat droplets, 1.9% albumin and 0.9% globulin, glucose and glycosaminoglycans, a few leukocytes and detached cells of the synovial membrane, the main component is water (94%). It is enriched with mucins by the synovial B cells of the synovial layer, including above all hyaluronic acid, which belongs to the non-exchangeable phase of the synovia and whose content significantly determines the viscosity of the synovia. Cold changes the viscosity of the synovia adversely and the lubricating effect of hyaluronic acid decreases.
synovial joint
see movement physiology – joint/synovial joint.
Synovitis
Inflammation of the synovium, often caused by overuse; ergonomic or material deficiencies are a further risk factor, as is a lack of regeneration.
Synsarkosis
Synsarcosis is a non-genuine joint type in which there is (at least) one muscle between the articulating bones. In humans, this is only the scapulothoracic gliding bearing; in some animals, the clavicle is connected via the brachiocephalic muscle, which is not present in humans.
systemic circulation
see movement physiology – circulation/systemic circulation.
Systole
see movement physiology – circulation/systole.
Systolic
see movement physiology – circulation/systolic.
Systolic blood pressure
see movement physiology – circulation/systolic blood pressure.
T
Tachycardia
see movement physiology – circulation/tachycardia.
Tachypnoea
see movement physiology – circulation/tachypnoea.
Tachytrophic
Tachytrophic tissues are those with a fast metabolism and short turn over. These tissues renew themselves quickly, adapt quickly and heal quickly. They are rarely affected by overuse syndromes. The conceptual opposite of tachytrophic is bradytrophic.
Tarsal tunnel
Medial depression in the area of the tarsal bones between the talus, calcaneus and inner malleolus, through which the tibial nerve, the posterior tibial artery and the tendons of the posterior tibial muscle, the flexor digitorum longus and the flexor hallucis longus run. The tarsal tunnel is covered by a retaining ligament, the flexor retinaculum. Swelling of the tendon of the tibialis posterior muscle can lead to pressure on the nerve and thus to tarsal tunnel syndrome, a nerve compression syndrome.
Tenderness on palpation
see movement physiology – nervous system/tenderness on palpation.
Tendinitis
see movement physiology – tendon/tendinitis .
Tendon
see movement physiology – tendon.
Tendon damage
see movement physiology – tendon/tendon damage.
Tendon elasticity
see movement physiology – tendon/tendon elasticity.
Tendon force
see movement physiology – tendon/tendon force.
Tendon healing
see movement physiology – tendon/tendon healing.
Tendon sheath / vagina synovialis tendinis
see movement physiology – tendon/tendon sheath.
Tendopathy / Tendinopathy
Tendon disorders with no specified etiology, but usually of an inflammatory or degenerative nature. Overuse is a common cause, with ergonomic or material deficiencies being a risk factor, as is a lack of regeneration.
Tenodesis
see movement physiology – tendon/tenodesis.
Tension belt / strong rope
Anatomical principle for the relief of bone structures by soft tissue structures. Probably the best-known tension belt is that of the femur: the relief of the femur formed by the iliotibial tract, which absorbs the significant moment that occurs in particular in the angle between its shaft and neck (the CCD angle of physiological 120° in adults), but also in the long shaft of the bone as a bending moment. When the leg bears weight with the knee joint even slightly bent, the quadriceps and thus also its vastus lateralis tenses, therefore its volume or cross-section increases the effect of the tension belt.
Another tension belt is found in the foot: without the plantar fascia, the longitudinal arch of the foot would tend to collapse in a plantar direction under the static load of the body weight and the dynamic loads when walking and running. The tension belt provided by the plantar fascia absorbs this as a passive tension belt together with the muscles of the foot as an active tension belt. The tension belt is therefore twofold, on the one hand passive (plantar fascia and ligaments such as the plantar long ligament in particular) and active through some intrinsic foot muscles. The weakening of one component, for example the active component due to a lack of training stimuli or overloading, quickly leads to overloading and thus to weakening of the other component, in this case fallen arches result and later a flat foot.
Tension pain
see movement physiology – nervous system/tension pain.
Terminal
see movement physiology – joint/terminal.
Terminal rotation / screw home mechanism
The terminal rotation of the knee joint is an involuntary external rotation of the lower leg in the knee joint of approximately 5°-10°, caused by the tension of the anterior cruciate ligament in conjunction with that of the iliotibial tract. In the standing leg with the lower leg as punctum fixum, we perceive it as an inward rotation of the thigh in the knee joint and an internal rotation of the thigh in the hip joint, whereas in a free leg we see it as an external rotation of the lower leg in the knee joint.
The final rotation represents a type of „physiological subluxation“ that brings the extended, loaded joint into a more stable state. In order to be able to bend the knee joint again, the popliteus, a largely transverse muscle that mainly turn in the lower leg and flexes the knee joint a little, must reverse the final rotation. It is supported by the knee flexors in the inner hamstrings, i.e. the semimembranosus, the sartorius and the gracilis. The onset of the ternimal rotation can already be detected at 20°-30° flexion in the knee joint, which is why the discussions about the extent to which or how pronounced the terminal rotation takes place during normal walking have not yet been concluded. This is certainly also dependent on the individual gait pattern.
External rotation of the tibia is achieved by anterior shift of the femur on the medial tibial condyle, which is longer than the lateral condyle.
Thenar
The ball of the thumb, which contains important muscles for moving the thumb:
Thoracic breathing
see movement physiology – circulation/thoracic breathing.
Thoracic spine
The middle part of the spine, consisting of 12 vertebrae, which lies between the cervical and lumbar spine and thus encompasses the entire upper body and, together with the ribs and sternum, spans the rib cage.
Thorax / Ribcage
The ribcage is the part of the torso spanned by the ribs and located above the pelvic and abdominal cavities. It partially covers the latter due to its dome shape. The rib cage is spanned by the ribs, which are attached to the thoracic vertebrae by two joints on the dorsal side and to the sternum by cartilage on the ventral side. This gives it a certain flexibility so that it can draw air into the lungs when inhaling. To do this, the costal arches are mainly pulled forward and upward, which increases the three-dimensional volume of the ribcage. This movement is caused by the inspiratory muscles, especially the scaleni and intercostal muscles. On the other hand, exhalation can occur passively when the rib cage contracts again due to the retraction forces of the lung tissue and, in an upright position, also by gravity of the ribcage. In addition to the lungs, it contains another highly vital organ, the heart. It serves as bony protection for both. In the middle of the chest between the two lungs lies the mediastinum, which contains the heart as well as large vessels and nerves. The thymus gland is also located in the mediastinum.
Tidal volume
see movement physiology-circulation/tidal volume.
Tiffenau Index
the focussed expiratory volume FEV1 that can be exhaled in one second, should be 70% of the forced vital capacity (VC ), i.e. the maximum forced inhalable volume. The Tiffeneau index of FEV1 / FVC should therefore be at least 0.7. On average, the index is 0.75 (75%), in healthy older patients it is closer to 0.7 (or 70%). The Tiffenau index is determined using the Tiffenau test.
Tilting moment
The tilting moment is the smallest moment that causes a body to tip over along the edge of its PSB in accordance with gravity. The tilting moment is therefore dependent on the PSB and the center of gravity.
Tissue repair / wound healing
Wound healing takes place in three phases, which are not strictly separated from one another, but whose processes merge into one another:
The phases in detail:
inflammatory phase
In the event of injury, vasoconstriction occurs immediately in order to minimise bleeding into the tissue. Platelets should have sealed the vessel within 5 minutes. As a result, the vessels are dilated in order to promote the healing process and the necessary supply through increased blood flow. The improved blood circulation leads to an increased temperature of the tissue, which should still be measurable on the surface of the skin depending on the location of the affected tissue. The temperature on the surface of the skin can allow a relatively accurate assessment of the reaction situation in the affected tissue. The location of the maximum temperature increase can be used to draw conclusions about the location of the event. Physiological hyperthermia can last for quite a long time; in the case of various pathologies of the knee joint, for example, it can last for three to six months. In the case of surgical procedures for cruciate ligament reconstruction or endoprostheses, the duration is also often 9 months, or the temperature remains permanently elevated. If the temperature is elevated by more than 1.5 degrees compared to the uninjured contralateral side, an excessive inflammatory reaction must be assumed. Acute injuries can also result in a temperature increase of two to four degrees compared to the contralateral side, and in the case of infectious injuries even more than 5 degrees. Thermography therefore allows the healing process to be observed. As far as the supplying vessels are concerned, they are not only widened (vasodilatation), but their membrane pores are also widened so that relevant cells can migrate into the affected tissue.
In addition to the primary injury, a secondary injury occurs when the affected area is extensively cleansed with collagenases, among other things. In most cases, supplying vessels have also been affected so that parts of the tissue have perished due to hypoxia. By generously cleaning up an affected area, a seamless connection between the tissue to be regenerated and the healthy tissue can be ensured.
Inflammatory transmitters locally cause a lowering of the stimulus threshold, resulting in allodynia and an exaggerated reaction to normal stimuli, i.e. peripheral hyperalgesia. These transmitters also travel towards the CNS and activate so-called dormant synapses, which are not normally actively involved in the transmission of information. This can lead to the phenomenon that stimuli are transmitted via a neighbouring spinal nerve, for example further cranially, so that misperceptions can arise and the usual proprioception is disturbed, which can result in movement insecurity as well as restricted innervation of muscles.
If infrared thermography is used to monitor the progression of inflammation, it is primarily the side-by-side comparison that must be assessed rather than the absolute value. It is important that there are no interfering influences, such as crossed legs, tight clothing or heat radiation, for example from the sun. If such influences were present, they should have disappeared after 8 minutes. In normal healing processes, the temperature difference to the opposite side is no more than 2 degrees and increases by a maximum of one degree during physical exertion. A reduction in the temperature increase should be recognisable within the first week. The rest pain should gradually change to exertion pain. Automobile movements are permitted as long as they are largely pain-free. If this cannot be parameterised, immobilisation can also be performed in the short term. Adverse endocrinological and neurological influences, such as those caused by stress, should be excluded as far as possible. If the above-mentioned parameters of the physiological inflammatory response are violated, e.g. if there is a temperature difference of more than 2 degrees compared to the contralateral or a temperature increase of more than one degree after stress, cold can be applied. The normal temperature of a joint is around 32.8 degrees compared to around 35.9 degrees for inflammation. With endoprostheses, with their increased friction, it can rise to over 43 degrees. However, the activity of catabolic enzymes, which is significant in the inflammatory phase, increases with the temperature, so that the temperature increase should be reduced externally by cooling. To date, there are no standardised and reliable recommendations for the extent of cooling, but it is certain that the skin temperature should not be lowered below 13°. Medication with corticosteroids or NSAIDs should be carefully considered, as these substances impair matrix synthesis. This has been proven in animal experiments for tendon, ligament and bone tissue. The effect can lead to the repaired tissue being less tear-resistant or stable. If the inhibition of excessive inflammation is desired, natural anti-inflammatory agents found in food should be used.
proliferation phase
The proliferation phase does not begin after the end of the inflammation phase, but with a short time delay immediately after the triggering event, whereby the inflammation event is predominant in the first few days. One process therefore creeps out while the other creeps in. Indications of the transition to the predominant proliferation phase can be found in the decrease in the temperature difference and the disappearance of rest pain. Only exertional pain should still be triggerable. While the inflammation phase is often given as one week, the proliferation phase is given by most authors as 21 days, i.e. three weeks. However, this information is only partially accurate, as a distinction must be made between bradytrophic and tachytrophic tissues. Systemic diseases, nutritional deficiencies or stress can also have an influence on the length of the proliferation phase. In this phase, mesenchymal stem cells migrate from the bone marrow or the vascular walls to the site of action and proliferate through mitosis. The cells develop their organelles, whereby the endoplasmic reticulum and the ribosomes are particularly important due to protein and matrix synthesis. Collagen is first formed by the less stable type 3 and later, depending on the tissue, by the other types: where mainly compression and shear forces are present: type 2, where mainly tensile stresses prevail: type 1. The conversion from type 3 to type 1 and 2 continues in the remodelling phase.
During wound healing of the connective tissue, myofibroblasts are also formed which, in addition to the normal production of ground substance and collagenous fibres, have a contractile cytoskeleton with which they hold on to their exterior via tentacle-like projections and pull the edges of the wound together. From the proliferation phase, it is important to familiarise the growing tissue with the tasks that it will later be able to perform through training. This is known as automobilisation exercises. The tendons and ligaments require pulling stimuli and cartilage tissue compression and shearing forces. These movements must be carried out in a pain-free area; aggressive stretching should be avoided. In relation to the load deformation curve, the foot region should not be left. At the beginning of the proliferation phase, the stability of the new tissue is only around 15 to 20% of the healthy tissue. Stretching beyond the foot phase would lead to re-traumatisation. The mobilisation exercises should be carried out repeatedly throughout the day. If no irritation occurs, the number of repetitions can be increased from 10 to 40. Any intensity that exceeds 30% of the 1RM is contraindicated in this phase. Anything that could cause local acidosis must be avoided, as this would disrupt wound healing. In addition to the mobilisation exercises, only basic endurance and local muscle endurance exercises are indicated, also because they generally provide sufficient support for revascularisation of the affected area. Coordination training of the local stabilisers is also permitted.
remodeling phase
Situations that are difficult for the articular cartilage such as high speeds, high compression forces and high shear forces should, if at all necessary, only be introduced in the remodelling phase. The extent of the strain should be confirmed by clinical tests. It is not normally possible to take up strenuous sports before 9 months have passed. The ROM is only temporarily limited if there is a risk of retraumatisation.This can lead to signs of degeneration after just three to six months. As haemorrhage into the joint space is conducive to cartilage healing, procedures such as drilling, shaving and microfracturing of the subchondral bone have been invented. This results in a healing behaviour that is comparable to the full thickness defect. After 6 months, a relatively stable fibrocartilage should have formed. Of these procedures, however, only microfracturing can be assessed as positive in the long term; the other two procedures show only 50% patient satisfaction after five years. In the case of microfactorisation, the result is good in 80% of cases even after a four-and-a-half to 11-year follow-up, but a long-term moderate deterioration must be assumed. Autologous chondrocyte transplantation (ACT) is another procedure that is no longer performed by covering the affected area with a periosteal flap, as this is more likely to hypertrophy, which required treatment in 25% of cases. Today, matrix-coupled ACT is more common, whereby the cells are transferred to the defect on a collagenous carrier matrix. A further improvement in the third generation of ACT is that the procedure is performed arthroscopically. This creates a mixed cartilage tissue consisting of fibrocartilage components in the inserted hyaline cartilage. It does not seem possible to estimate the proportion. Here, too, a three-month proliferation phase is assumed, but the damage can be filled with matrix after just six weeks. The remodelling phase is given as 6 months. However, the repair tissue is only likely to be fully integrated after years. In a further step, a reservable collagen scaffold is created, which contains growth factors and blood serum so that the cells can largely form the collagen themselves with their matrix production. To date, however, it has never been possible to restore homogeneous hyaline cartilage, resulting in reduced resilience. Another option for cartilage repair is osteochondral transplantation, whereby cartilage bone substance is punched out from other donors, i.e. allograft, or from the patient’s own, non-stressed cartilage areas, i.e. autograft, and placed in the defect. The thickness of the graft is very important to ensure that the joint surfaces remain congruent or retain their natural degree of congruence. The trials to date have been promising. Bentley et al. prescribed only 48 hours of off-loading post-operatively and then started partial weight-bearing up to full weight-bearing, with normal weight-bearing and ability to work after six weeks. Manulopoulos parametrised similarly and came to the conclusion that areas subjected to more stress were more likely to heal hyaline than areas subjected to less stress. Both results indicate that after 48 hours, work should be carried out with ever-increasing weight-bearing up to full weight-bearing, with weight-bearing being controlled by clinical tests. After three months, the patient should have regained full weight-bearing capacity and the ability to work. When controlling the load, it should not be forgotten that the main load on the cartilage results from the tension of the muscles and not from the gravity of the body. The transition from the proliferation phase to the remodeling phase is also fluid and cannot be easily determined clinically. Changes in the metabolism of the affected tissue can still be detected years later, so it is assumed that the remodelling phase lasts for a year in any case. An important factor in this phase is the remodelling of collagen type 3 into collagen type 1 or type 2, depending on requirements, and the corresponding crosslinking, whereby the resilience of the tissue correlates with the extent and structure of the crosslinking. In this phase, the fibres must also be aligned according to the acting force, if this has not already been done. Restrictions in mobility must now be removed with appropriate stretching, whereby final stretching pain can naturally occur. A reverberation (post-stress pain) should not occur. The intensity of the stretch now goes beyond the foot phase into the linear range. If any discomfort remains after leaving the final position, the cause lies elsewhere; the pain would then be transmitted via C nerve fibres that release inflammatory mediators, which should be avoided. Automobilisation exercises are now held for much longer and intensified beyond the foot phase. The loads corresponding to the main motor skills and the type of sport practised are now slowly increased to the required level. In the case of extremely bradytrophic cartilage, restitutio ad integrum is generally not to be expected. A distinction is made here between partial thickness defects and full thickness defects. The former do not extend to the subchondral bone and do not cause haemorrhage, which also means that only limited healing is possible. It is assumed that only small defects with a maximum size of three or 5 mm² can heal completely, which should take around 9 months. In the case of larger defects, chondrocytes at the wound edges become active after just one day by proliferating and producing more matrix material. In addition, turnover is promoted by growth factors. However, the increased activity only lasts for one to two weeks and then returns to the initial level. The tissue produced is removed again during the subsequent remodelling phase, leaving a defect. These defects may or may not lead to further erosion. Clinically, the situation can remain stable, which is usually assumed if the injury does not exceed 2 mm². All injuries that exceed 10 mm² inevitably lead to increased compression stress, which also affects deeper layers of cartilage. If, for example, haemorrhage occurs during a rupture of the anterior cruciate ligament, this provides the necessary cell material and growth factors, which allows cartilage damage to heal better. The situation is different with full thickness defects. As the well-innervated and vascularised subchondral bone is also affected, normal healing occurs. The haemorrhage transports undifferentiated stem cells, nutrients and other factors into the affected area, where producing fibroblasts and fibrochondroblasts differentiate and begin to produce matrix. The end of the proliferation phase can be expected after three months. However, there is no restitutio ad integrum because no hyaline articular cartilage is produced, but a similar cartilage that is later remodelled into fibrocartilage in the remodelling phase, whose mechanical resilience is lower.
Titin
see movement physiology – muscle/titin.
Tonus (muscle tone)
Basic tension of the muscles. Force (measured at the attachment or origin) with which the muscles pull the origin and attachment towards each other. Generates a basic (rotational) moment in most joints of the musculoskeletal system.
Torsional moment
Torque acting on a body in the direction of torsion.
Torque
the rotational effect of a force acting on a lever arm on a solid body rotating around an axis. The torque is the product of the force (F in N Newtons) and the distance, i.e. the length of the lever r in m meters, and is therefore measured in Nm. In the case of a circular movement, the torque acts on a tangent to the arc of the circle at the point where the force is applied.
Total lung capacity
see movement physiology – circulation/total lung capacity.
Total endoprosthesis (TEP)
A total endoprosthesis is a complete, often limited functional replacement of a joint. For information on the limitations and possible complications, see also pathology: status after endoprosthesis.
TPR (total peripheral resistance)
see movement physiology – circulation/TPR.
Trabeculae
see movement physiology – bone/trabeculae.
Trabecular bone / spongy bone
see movement physiology – bone/spongy bone.
Trachea
see movement physiology – circulation/trachea.
Traction
In physiotherapy, traction is a passive measure that pulls the articulating partners of a joint away from each other. This can serve to relieve cartilage or intervertebral discs, reduce muscle tone, stretch ligaments if necessary or reduce pressure on the nerves accompanying the joint. Traction is intended to stimulate the production of synovial fluid (joint fluid), which improves joint lubrication. Traction can be applied manually by the therapist (manual therapy) or with weights. Particular care must be taken if there is a risk of dislocation or hypermobility.
Traction osteophyte
A traction osteophyte is a change in a bone that is caused by repeated strong traction of a tendon or ligament on a bone so that the bone grows against the pulling structure. The traction osteophyte therefore has little in common with the classic osteoarthritic osteophyte, which presumably occurs when cartilage tissue is expelled from the joint space and ossifies. While the traction osteophyte itself usually remains asymptomatic, it can lead to secondary disorders such as impingement, for example in ischiofemoral impingement, in which the trochanter minor grows and restricts the quadratus femoris space.
There are other disorders with the formation of traction osteophytes: the plantar fasciitis that forms in plantar heel spur, the dorsal heel spur (posterior calcaneal spur) that forms in the Achilles tendon. Traction osteophytes can form on the coracoacromial ligament during frequent overhead activities or sports, as well as on the acromion for the same reason. The olecranon can also develop traction osteophytes in triceps tendon insertion tendopathies. In spondylosis deformans spinal changes with intervertebral disc disease), the pressure of the displaced intervertebral discs against the lig. flavum leads to traction osteophytes at the edges of the vertebral body.
Training zones
see movement physiology – muscle/training zones.
Translation
Translation is a rotation-free movement of two joint bodies against each other. In flat joints, this can be a physiological movement, as a further (up to two) movement dimension(s) in addition to axial rotation. Translation is often referred to in connection with non-physiological movements in cases of joint instability. Pathological translations are therefore the unintended shifts of the bones in a joint, in the case of the knee joint, for example, lateral/medial and frontal/dorsal. Compression (the compression of a joint) and traction (the pulling apart of the traction (the pulling apart of the bones in the joint, as in physiotherapy, for example) is also a translation, even if the term is used far less frequently in this context.
Transverse / transversal
direction from lateral to medial or further to counterlateral, in other words a transversal direction is a vector in the line of intersection between the frontal plane and transversal plane through the person standing in standard anatomical position, or in short, from left to right or vice versa.
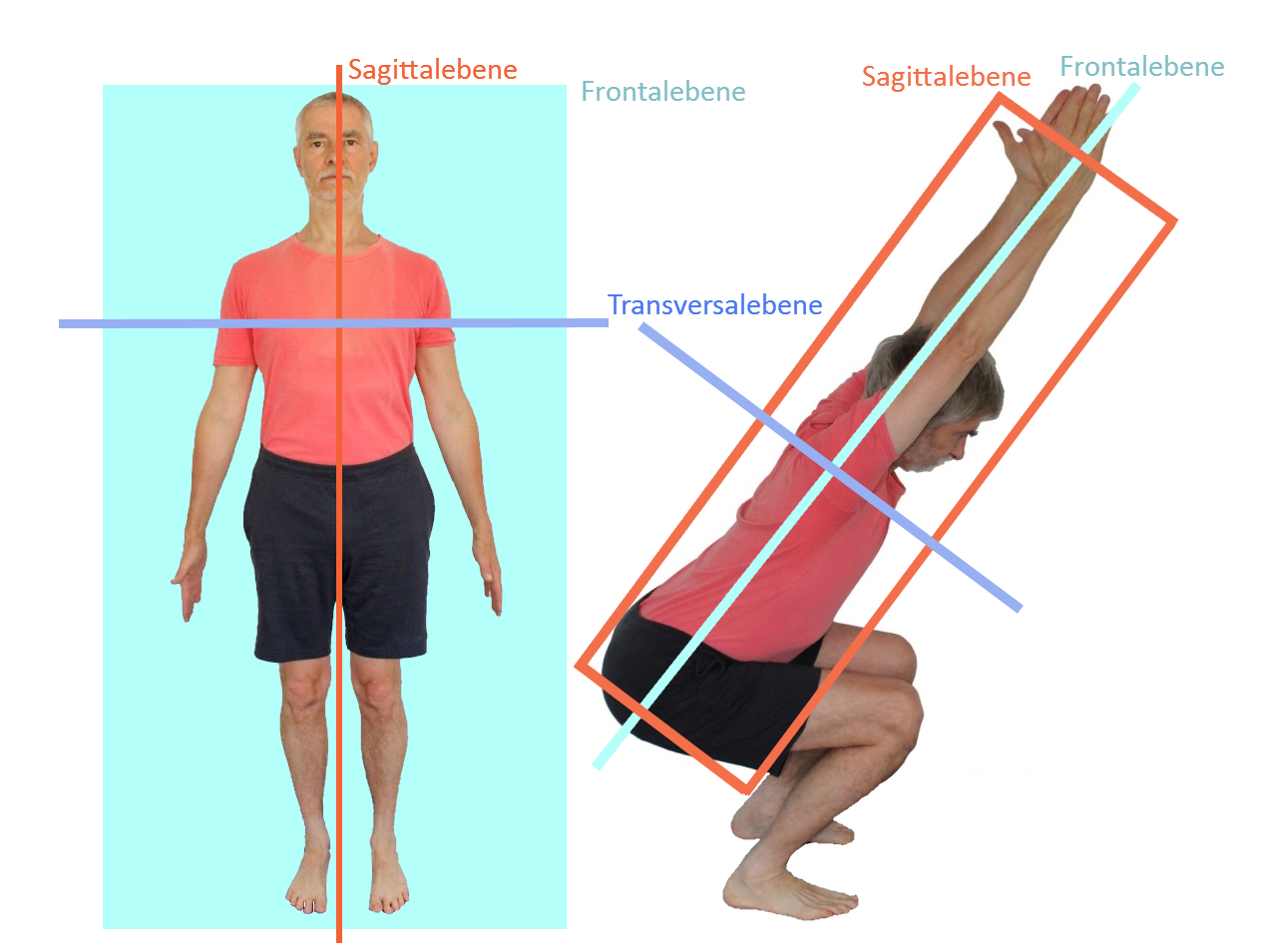
Transverse abduction (shoulder joint)
Horizontal abduction (in the transverse plane) while maintaining the degree of frontal abduction(anteversion). To a certain extent, this movement is possible without moving the scapula; beyond this, it forces further retraction.
Transverse adduction (shoulder joint)
Horizontal adduction (in the transverse plane) while maintaining the degree of frontal abduction (anteversion) To a certain extent, this movement is possible without moving the shoulder blade; beyond this, it forces further protraction.
Transverse abduction (hip joint)
Horizontal abduction (in the transverse plane) while maintaining flexion in the hip joint. How far the leg can be abducted transversely depends on its rotation and the flexion in the hip joint.
Transverse adduction (hip joint)
Horizontal adduction (in the transverse plane) while maintaining flexion in the hip joint.
Transverse abductors (shoulder joint)
the muscles that perform transverse abduction, i.e. horizontal abduction (in the transverse plane) while maintaining frontal abduction (anteversion). To a certain extent, this movement is possible without moving the shoulder blade, beyond which it forces a further retraction. Pure movement in the shoulder joint is performed by the deltoid pars spinalis, as well as the infraspinatus and Teres minor, and, depending on the position of the arm, the supraspinatus. The retraction of the shoulder blade is the task of the rhomboids and the trapezius.
Transverse adductors (shoulder joint)
the muscles that perform transverse adduction, i.e. horizontal adduction (in the transverse plane) while maintaining frontal abduction (anteversion). To a certain extent, this movement is possible without moving the shoulder blade, beyond which it forces a further protraction. The pure movement in the shoulder joint is performed by the deltoid pars clavicularis, pectoralis major and coracobrachialis, also from the biceps and to a lesser extent from further transverse abduction from the Teres major. The protraction of the shoulder blade is the task of the serratus anterior and, to a lesser extent, the pectoralis minor.
Transverse plane
a horizontal sectional plane through the person standing in standard anatomical position.
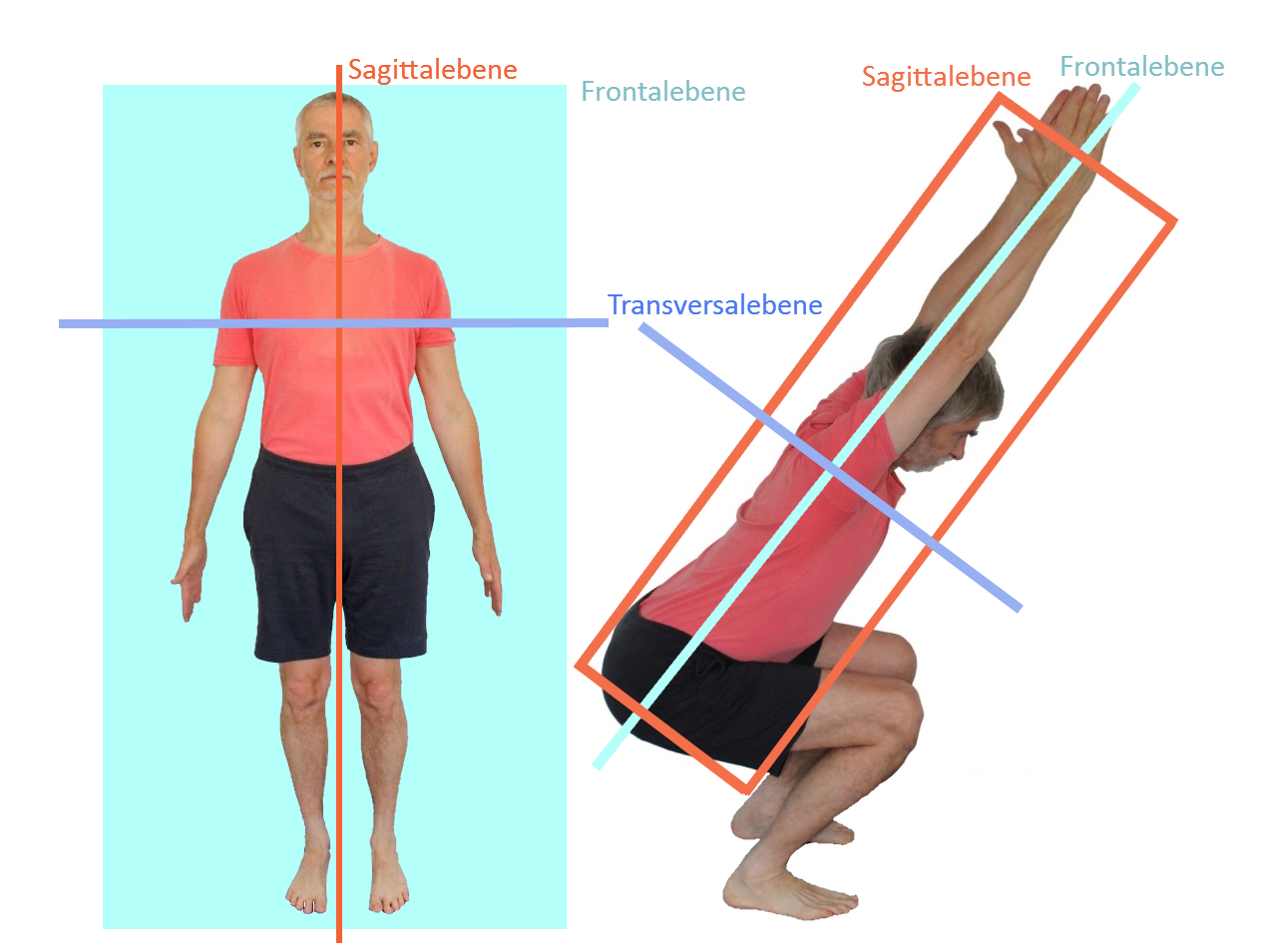
Transversospinal System
Muscles that run between transverse processes and spinal processes of various vertebrae belonging to the medial tract of the autochthonous back muscles: Rotatores breves et longi (lumborum, thoracis et cervicis), Multifidi (lumbales, thoracici, cervicis), Semispinalis (thoracis, cervicis, capitis).
Trapezius line
In the area between the acromion and the neck, the trapezius forms the most cranial part of the body and thus part of the silhouette, still above the clavicle. If this area is viewed dorsally or ventrally, the trapezius rises from lateral to medial in standard anatomical position, i.e. with depressed shoulder blades; this part of the silhouette is referred to as the trapezius line. From a certain degree of elevation of the shoulder blades, the described rise from lateral to medial is lost. A trapezius line that does not rise medially can therefore be interpreted as a sign that the shoulder blades are not fully depressed. With fully elevated scapulae, the course of the trapezius line should be reversed: descending from lateral to medial. However, the extent of the possible elevation and thus this phenomenon depends on restrictions in the flexibility of the depressors of the scapula and the lateral and, above all, frontal adductors of the shoulder joint, which are indirect depressors of the scapula, especially with the arm raised.
Triceps coxae
Triceps coxae is the name for the three muscles that pull from the caudal-medial (gemellus superior of the ischium), medial (gemellus inferior of the ischium) and cranial (Obturatorius internus of the ilium) to the trochanteric fossa of the posterior femur and turn out the thigh in the hip joint. The external obturator muscle is not included, as it attaches ventrally to the ischium and but also turnes out the thigh in the hip joint.
Trochoid joint / rotary joint / pivot joint
see movement physiology – joint shapes/pivot joint
Truncohomeral muscles
Muscles that pull from the trunk to the upper arm bone (humerus) to move the upper arm:
truncoscapular muscles
Muscles that pull from the trunk to the shoulder blade to move it:
- Rhomboideus major
- Rhomboideus minor
- Levator scapulae
- Pectoralis minor
- Serratus anterior
- Subclavius
- Trapezius
Tubercle
see movement physiology – bone/tubercle.
Tubular bone / long bone
see movement physiology – bone/long bone.
Turn over, cell moulting, cell replacement
The time in which a tissue is completely renewed, or more precisely, in which differentiated cells of a tissue are replaced. In physiology, a distinction is made between bradytrophic and tachytrophic, i.e. slow and fast metabolizing tissues. The bradytrophic tissues include most tissues without (or with very little) their own arterial supply, i.e. most cartilage, ligaments and tendons. In contrast, cells in contact with the outside world generally have a higher metabolic rate; both the skin and mucous membrane cells that are obviously part of the human exterior and those of the mucous membranes of the digestive and respiratory tracts are tachytrophic. The parts of the CNS, on the other hand, do not renew themselves. On average, the skeleton renews itself every 10 years, the liver renews itself in 300 to 500 days. The renewal times of various tissues and organs calculated by Jonas Frisen (Karoslinska Institute):
- Small intestinal epithelium: 2-4 days
- Gastric mucosa: 2-9 days
- Cervix: 6 days
- Synovia (joint fluid): 7-14 days
- Alveoli: 8 days
- Taste buds: 10 days
- Thrombocytes: 10 days
- Osteoclasts: 2 weeks
- Intervertebral disc (gelatinous nucleus): 2 – 3 weeks
- Epidermal cells: 10-30 days
- Muscle tissue: 3 – 4 weeks
- Bone tissue: 4 – 6 weeks
- Lymph vessel tissue: 4 – 6 weeks
- Trachea: 1-2 months
- Sperm: 2 months
- Osteoblasts: 3 months
- Erythrocytes: 4 months
- Hepatocytes: 0.5-1 year
- Intervertebral disc (fibrous ring): 1 – 1.5 years
- Tendon tissue: 1 – 1.5 years
- Joint capsule tissue: 1 – 1.5 years
- Tape fabric: 1 – 1.5 years
- bones (spongiosa): 4 Jahre
- bones (corticalis): 35-50 Jahre
- Fat cells: 8 years
- Skeleton: 10 years
- Heart: 100 years (increasing with age)
- Cartilage tissue: 200 – 400 years
These figures also result in different times for the healing of injuries: while mucous membranes and skin heal quickly and even bones, other, passive parts of the musculoskeletal system take significantly longer or, in the case of cartilage, even have a turnover that is beyond the lifespan.
TUT (Time Under Tension)
TUT is the time during which a muscle is under load in a
repetition or a set.
U
Ulnar abduction (hand)
Swiveling the hand toward the ulna, in other words: reducing the distance and angle between the thumb or metacarpal bone 5 and the ulna.
Ulnar adduction (hand)
Returning the ulnar abduction to the zero position, i.e., increasing the distance and angle between the thumb or metacarpal bone 5 and the ulna.
UMN (Upper MotoNeuron)
see movement physiology – nervous system/UMN.
Underhand grip
An underhand grip is a grip on an object, often a piece of sports equipment such as a dumbbell, in which the back of the hand points downwards, the object rests in the palm of the hand and the object or its handle is enclosed by the fingers through the force of the finger flexors. In contrast to the overhand grip, the forearm is in supination and the palmar flexors together with the finger flexors hold the weight. In the underhand grip, the brachialis and arm biceps are also powerfully engaged.
Underuse
Underutilization of bodily functions leads to disorders. This term usually refers to the musculoskeletal system and means a quantitative lack of movement. If certain movement options are underutilized, however, this is narrowuse, defining a qualitative lack. In practice, underuse and narrowuse often occur together. A variety of effects can be observed here, from osteoporosis of the ageing, comfortable movement and exertion avoider to instabilities that develop in an underused musculoskeletal system due to a lack of training stimuli, through to the cartilage damage that can result from prolonged immobilization after injuries. Unintentional weight gain is well known as a symptom of a medium-term lack of exercise (and an inadequate calorie balance), but tests also show that massive underuse (a limit of a few hundred steps per day) leads to clearly demonstrable fatty degeneration of the liver and heart within 14 days. The decrease in cardiopulmonary resilience caused by underuse, the increase in the risk of heart attack, stroke, diabetes, obesity with its risk factors, arteriosclerosis and vascular dementia are also well known. But it is not only in anatomy and physiology that underuse has a pathological or pathogenic effect; the positive psychological effects of sufficient exercise behavior can also be demonstrated in the form of a reduced tendency to depression and better coping with everyday life, to name but a few.
unphysiological movement
unphysiological motion behaviour
see https://www.unphysiologisch.de/#unphysiological motion behaviour.
V
Vagus nerve
see movement physiology – nervous system/vagus nerve.
Valgus deformity / valgus position
Malalignment in which a part more distal deviates laterally compared to the physiolocigal case. In the case of the knee, for example, this would be knock-knees; in the case of the big toe, it would be a position too close to the second toe, i.e. hallux valgus.
Valgus stress
Force acting on a joint (at least) perpendicular to its physiological direction of movement, which results from the distal body part being pushed laterally in relation to the proximal body part. In the case of the knee, for example, this would be a force that pushes the intermediate knee inwards (medially) when the pelvis and foot are fixed or pushes the foot laterally when the thigh is fixed. In asanas, a certain amount of valgus stress occurs in upavista konasana, for example, especially when it is performed against the wall or as a partner exercise in which pressure is applied to the lower legs or feet. Valgus stress also occurs in the lying version of upavista konasana if the heels are placed too low on the wall. To avoid valgus stress in the finger joints (especially the proximal and distal ones), the palm of the hand is placed on the floor in the sitting twist instead of the fingers at more or less right angles to the direction of the force exerted, as is often the case. If, e.g. the fingers were pointing away from the pelvis, this would create valgus stress in fingers 2-5 and varus stress in the thumb. In the case of knock-knees, the knee joint is exposed to valgus stress when the leg is loaded, i.e. in standing leg situations.
Variety
An anatomical variety is a deviation from the norm without functional or clinical abnormality or limitation, although this distinction is difficult to make clearly. One variety is the cervical rib, a unilateral or bilateral additional zeroth rib (an atavisumus, i.e. a recurrence of evolutionary relicts), which occurs in 1% of cases, is attached to the C7 and has a cartilaginous or connective tissue connection to the sternum. The cervical rib is usually inconspicuous and goes unnoticed; at best, it is discovered as an incidental finding during imaging. In some cases, however, it can also cause thoracic outlet syndrome.
Varus deformity / valgus position
Malalignment in which the distal part of the body deviates medially compared to the physiolocical case. In the case of the knees, for example, this would be bow legs.
Varus stress
Force acting on a joint (at least partially) perpendicular to its physiological direction of movement, which results from the distal body part being pushed medially in relation to the proximal body part. In the case of the knee, for example, this would be a force that pushes the knee outwards (laterally) when the pelvis and foot are fixed or pushes the foot medially when the thigh is fixed. In the lying version of upavista konasana, varus stress occurs if the feet are placed too high on the wall. If they are placed too low, valgus stress occurs. To avoid varus stress in the thumb joints (especially the distal joint), in sitting twist the palm of the hand is placed on the floor instead of the fingers at a more or less right angle to the direction of the force exerted, as is often the case. If the fingers were pointing away from the pelvis, this would result in valgus stress in fingers 2-5 and varus stress in the thumb. In the case of bow legs, the knee joint is exposed to varus stress when the leg is loaded, i.e. in standing leg situations.
VNS (vegetative/autonomous nerve system)
see movement physiology – nervous system/VNS (vegetative nervous system).
Vene
see movement physiology – circulation/vene.
Venous valve
see movement physiology – circulation/venous valve.
Venole
see movement physiology – circulation/venole.
Ventral
denotes a direction and means „from or to the front“ and is identical to the term anterior or frontal. The conceptual opposite is dorsal, which in turn corresponds to the term posterior.
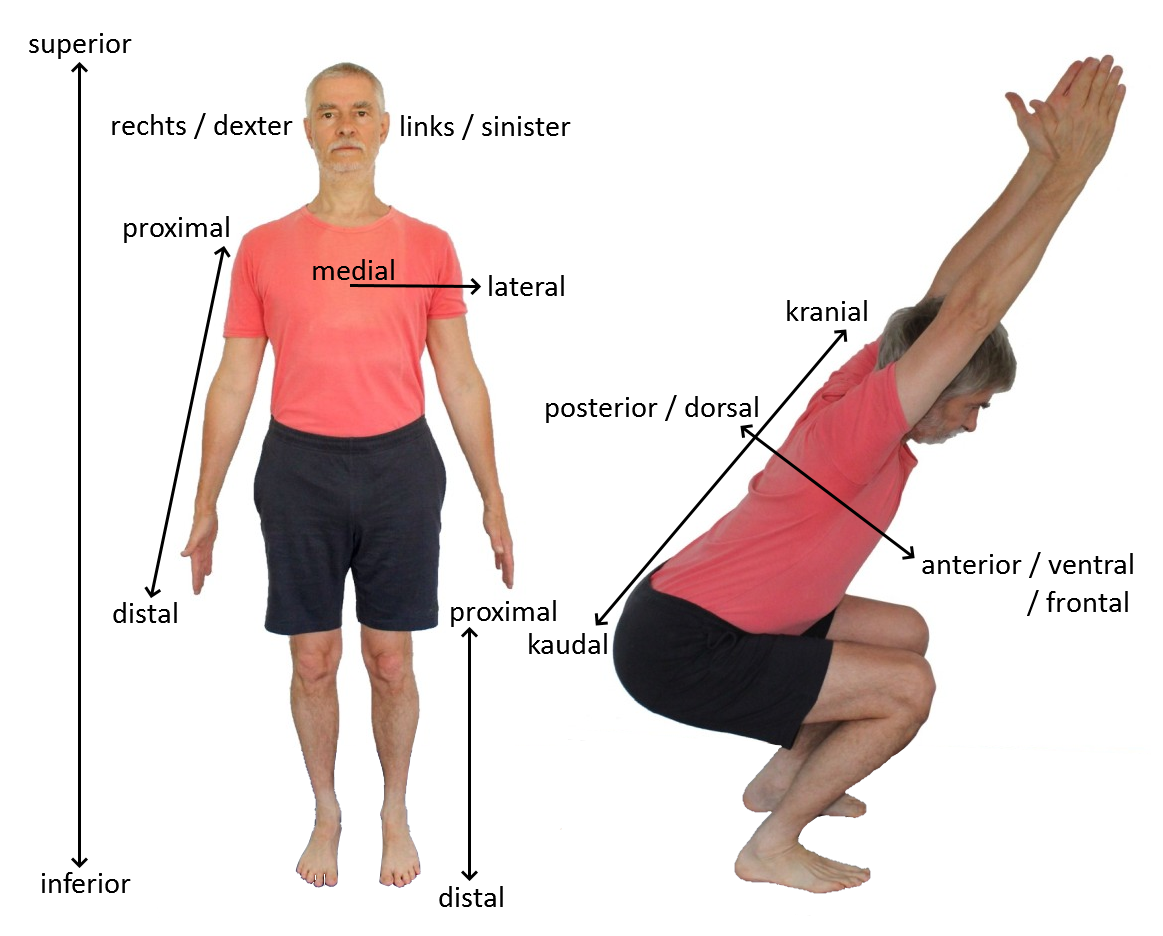
Vicious circle (circulus vitiosus)
A vicious circle is a pathophysiological loop of adverse effects (or dysfunctions) involving at least two factors. A simple example would be knee pain leading to decreased movement, which in turn worsens the situation of the knee joint and its muscles, leading to even less movement, and so on. In pathology, several of these vicious circles are known. In logic, on the other hand, a circular argument is called a vicious circle.
Vital capacity
see movement physiology – circulation/vital capacity.
W
Waist to Height Ratio (WHTR)
The Waist to Height Ratio (WHtR) sets the waist circumference in relation to body height and is therefore a much more useful measure than the still frequently used BMI. The critical abdominal fat in particular is clearly included in the WHtR; and in addition, the muscular make-up of the person in the measured area at the waist is very little affected, so that hardly any false positives are to be expected here. The assessment is slightly age-dependent:
- up to 40 years: threshold value for moderately increased risk is 0.5
- 40-50 years: threshold value for moderately increased risk is 0.5 + 0.01 * (age – 40)
- from the age of 50: threshold value for moderately increased risk is 0.6
and classified as
- optimal: 0.4 to 0.499
- moderate risk: 0.5 to 0.599 (see age-dependent definition above)
- High risk: from 0.6
Here you will find a calculator for WHtR and BMI.
Waist circumference / abdominal girth
An increased waist circumference of more than 80 cm (women) or 94 cm (men) is considered a risk factor for cardiovascular diseases such as CHD, heart attack, stroke and also type 2 diabetes mellitus. At 88 cm and 102 cm respectively, the risk is considered to be significantly increased. The waist circumference is measured on an empty stomach, standing, exhaling slightly, midway between the iliac crest and the lower ribs.
Walking (in general, in any form)
see movement physiology – walking.
Warming up
Warming up is a time-honoured practice in sport, without the physiological principles being known in detail to all those performing it. It includes warming up the
active musculoskeletal system on the one hand, and the passive on the other. In the area of the active musculoskeletal system, the focus is on the muscles. On the one hand, the warm-up should pre-activate the relevant muscles, while on the other hand the increase in flexibility associated with the warm-up is desirable, because it reduces the risk of muscle fibre tears, tendon tears, strains and even ligament tears.
In the area of the passive musculoskeletal system, the focus is on warming and stimulating the formation and release of synovial fluid („joint lubricant“). It is known that the main component, hyaluronic acid, becomes increasingly cross-linked with decreasing temperature, which increases its viscosity and worsens lubrication, thereby increasing the tendency of cartilage to wear out. Furthermore, warming up leads to better saturation and increased thickness of the cartilage via the increased synovia and thus to its improved resilience. As the joint itself has no significant heat-generating tissue, it is primarily the heat generated by the highly exothermic muscles that acts locally on the joint and is also transported to the joint via the bloodstream that does this. This implies that the time it takes to „warm up“ the joint is much greater than that required by the muscles.
Warming up also has positive effects outside the movement apparatus. The core body temperature rises due to muscular metabolic activity, which accelerates various chemical reactions in metabolic processes (RGT rule of chemistry), especially because the effectiveness of enzymes increases. In the nervous system, excitability is increased, which leads to faster reactions and contraction and thus enables better movement sequences. The sensory system is also sharpened, proprioceptively, especially in the muscle spindles, but also the pressure and touch sensors of the skin. The cardiac output and respiratory volume are increased, as is the amount of circulating blood, which improves performance and the supply of all tissues in several ways. Without warming up, this performance would only be achieved with a certain time lag.
In addition to the general warm-up of the body with the aforementioned positive effects, the relevant muscle groups in particular should be sufficiently pre-activated. An inadequate warm-up tends to lead to side stitches and premature fatigue due to the acidic metabolites produced.
As the risk of non-traumatic injury generally increases with age, warming up also becomes more important with age. Endurance athletes require more warm-up time than most team athletes due to the non-stop exertion
. There is no such thing as too much warm-up, except in the sense of fatigue already setting in, which reduces performance and increases susceptibility to injury. The mental/psychological attitude can have an influence on the warm-up, positive motivation and performance expectations improve the effect.
The amount of time needed to warm up depends on the time of day; more time is needed in the morning and less as the day progresses towards the evening. In high ambient temperatures, if the body is sufficiently warmed up, temporary cooling before the performance requirement can also be useful.
Weekend warrior
Weekend warrior is the term for people who do not exercise during the week, but then do so more intensively at the weekend, or at least several times a weekend. Their sporting behaviour can reduce the general health risk in the cardiopulmonary sense and in other areas in a reasonably comparable way to regular sport during the week. A Chinese study showed the following risk reductions:
- Parkinson’s: 45%
- Dementia: 26%
- Stroke: 21%
- Depression: 40%
- Anxiety disorder: 37%
So while there are clearly some health benefits, irregular sporting behaviour puts significantly more strain on the exercise system than regular sport. There are clear disadvantages in terms of injury frequency and susceptibility. An increase in performance can also hardly be achieved as a weekend warrior in the same way as with a training plan that is cleverly spread out over the week. The reason for this is obvious: muscular regeneration during intensive training is by no means complete from one day to the next, i.e. in the order of 24 hours. If you wanted to schedule a training programme so that regeneration is essentially complete the next day, it would be too low-threshold for an increase in performance.
From a technical point of view, therefore, those affected would be engaging in regular weekend short-term overtraining without, of course, risking the psychological symptoms of long-term overtraining. It would be somewhat more favourable for the effectiveness of the overall training on a weekend if the loads on the weekend were as varied as possible and the same sport was not practised from Friday to Sunday. But even then, the bradytrophic tissues are very likely to be overtaxed, as their regeneration time is sometimes dramatically longer than that of the muscles.
It is not uncommon for weekend warriors to be former athletes who practise their sport with their usual intensity at the weekend, even though they do not regularly train for it during the week, but often lead a largely sedentary lifestyle.
Wetness
Wetness or moisture is an important cofactor of cold, both in the form of liquid on the skin, as when swimming, and in the form of high humidity of the air. Even if cold air can bind less water vapor than warm air, the water content in the air is sufficient to extract heat from the body more quickly due to better thermal conductitity. This is very clear when we are in water: while we have a wafer-thin film of air on our skin when moving in the medium of air, which is largely held in place by our hair and prevents the temperature from dropping abruptly to outside levels, this is not the case when we are in water, especially when moving in water. If a person regularly spends long periods in the water, the body has to build up subcutaneous fatty tissue to protect itself from hypothermia. This effect can be seen regularly when comparing professional swimmers with terrestrial endurance athletes. The reduction of the film in which the temperature constantly drops and the resulting reduced protection against the cold is also known as the wind-chill effect in the air: the stronger the wind blows, the colder the air is perceived to be.
Windlass mechanism
The Windlass mechanism (winch mechanism) refers to the fact that the dorsiflexion of the toes towards the end of the rolling phase of the foot pulls the plantar plate of the metatarsophalangeal joints forwards (towards the tiptoe) and thus tenses the plantar fascia, which results in the forefoot being pulled towards the calcaneus and thus promotes the longitudinal arch of the foot. Under physiological conditions, the shortening of the distance between the metatarsal head and the calcaneus can be more than 1 cm, and the longitudinal arch of the foot is promoted accordingly. The Windlass mechanism can be impaired by a variety of disorders of the foot. This loss of function cannot be compensated for with orthoses.
Windkessel function
see movement physiology – circulation/Windkessel function.
Working heart rate / working pulse
The working heart rate is the amount by which the heart rate increases during exercise compared to the resting heart rate.
Working point
The point in the ROM at which a muscle works in a static pose, such as an asana or other isometric contraction. The term can refer to the sarcomere length or to the angle in a covered joint.
Working range
The section of the ROM relating to a movement that is used for a cyclical movement or repetitions of an exercise. The movement can be a one-dimensional movement or one in a combination of several movement dimensions. There are always (usually, but not always: soft) movement limits that define an interval or a set, which is referred to as ROM for this movement. The working range is the subset of the ROM used in the exercise. The term can refer to the interval of sarcomere length or to the angular interval in an spanned joint.
Wound healing
See tissue repair
