yogabook / joints / hip joints
Contents
- 1 Image: hip joint from dorsal (linkmap)
- 2 Hip joint
- 3 Articulating bones
- 4 Die Bewegungen und die ausführenden Muskeln
- 5 Die Bewegungen und die ausführenden Muskeln
- 6 Ligaments
- 6.1 outer ligaments – inner ligaments
- 6.2 Lig. capitis femoris
- 6.3 Lig. cooperi
- 6.4 Lig. ischiocapsulare
- 6.5 Iliofemoral ligament
- 6.6 Ischiofemoral ligament
- 6.7 Lacunar ligament
- 6.8 Lig. orbicularis
- 6.9 Lig. pectineum
- 6.10 Pubocapsular ligament
- 6.11 Pubofemoral ligament
- 6.12 Lig. transversum acetabuli
- 6.13 Membrana obturatoria
- 6.14 Lig. teres femoris
- 6.15 Iliotibial tract
- 7 Bursa (bursae)
- 7.1 Bursa bicipitis femoris superior
- 7.2 Gluteofascial bursa
- 7.3 Bursae gluteofemorales
- 7.4 Bursa ischiadica glutaei maximi
- 7.5 Bursa iliopectinea (also: Bursa subiliaca)
- 7.6 Bursa ischiadica obturatorii interni
- 7.7 Bursa obturatoris interni
- 7.8 Bursa pectinei
- 7.9 Bursa piriformis
- 7.10 Bursa quadratus femoris
- 7.11 Bursa recti femoris
- 7.12 Bursa subcutanea ischiadica
- 7.13 Bursa subcutanea sipna iliaca anterior superior
- 7.14 Bursa subcutanea trochanterica
- 7.15 Bursa subtendinea iliaca (iliaca subtendinea)
- 7.16 Bursa trochanterica musculi glutei maximi
- 7.17 Bursa trochanterica musculi glutei medii
- 7.18 Bursa trochanterica musculi glutei minimi
- 7.19 Bursa vesicularis semimembranosi
- 8 Bewegungen
- 9 Pathology
- 10 Tests
- 11 Pictures
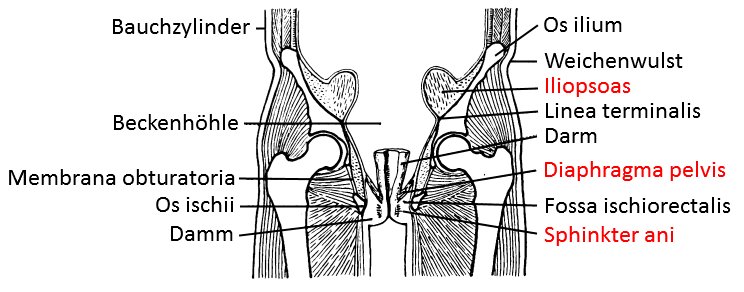
- 11.1 Hip joint, transverse incision
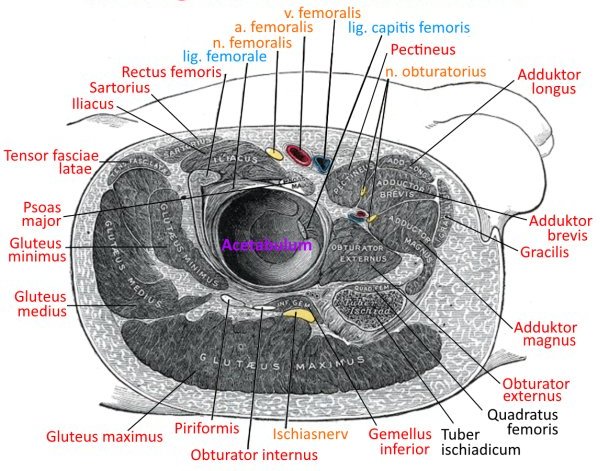
- 11.2 hip joint, medial
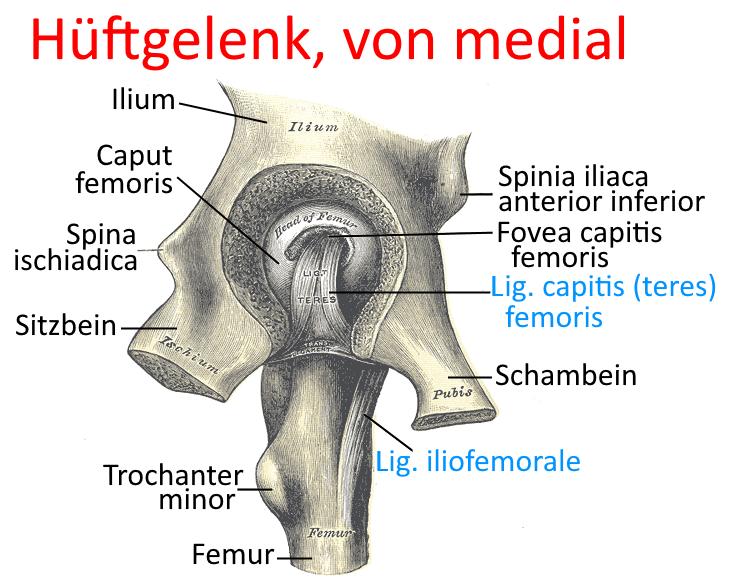
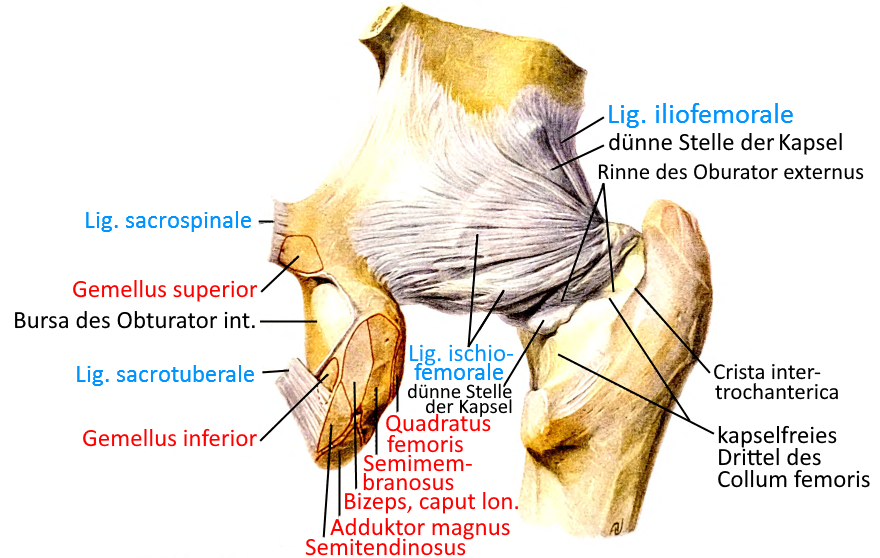
- 11.3 hip joint, dorsal
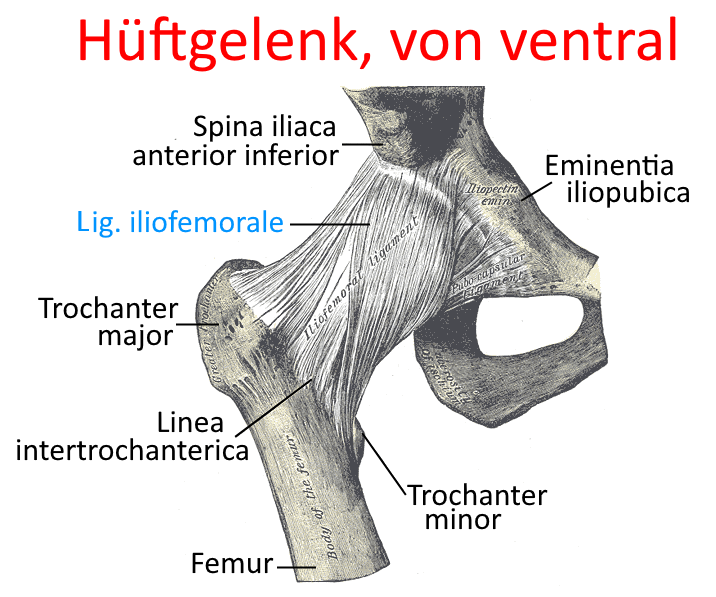
- 11.4 hip joint, ventral
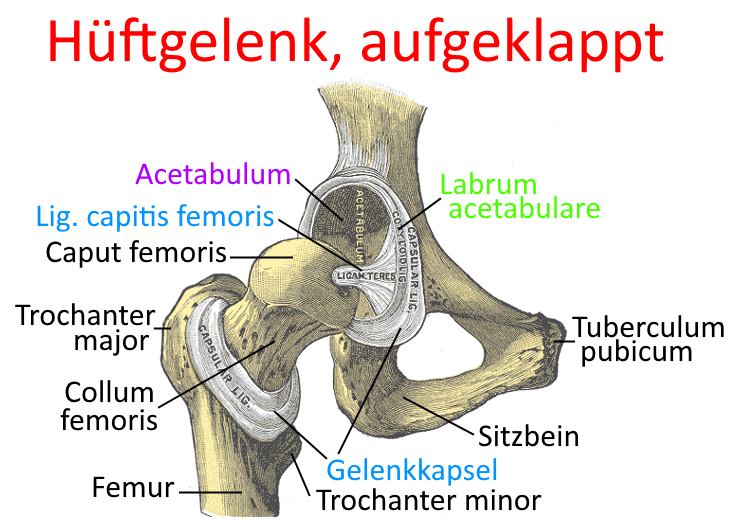
- 11.5 hip joint, unfolded
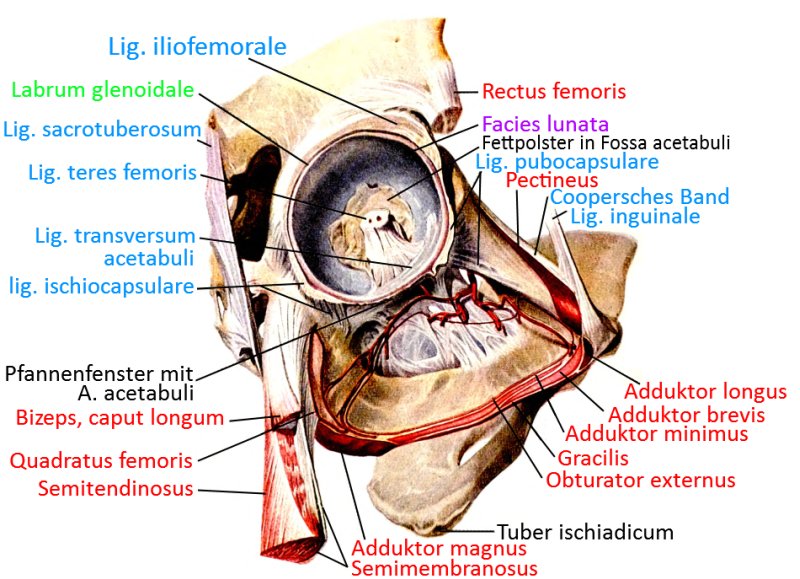
- 11.6 Acetabulum in context (image links to linkmap)
- 11.7 hip joint from ventral (image links to linkmap)
- 11.8 hip joint from ventral, saw cut (image links to linkmap)
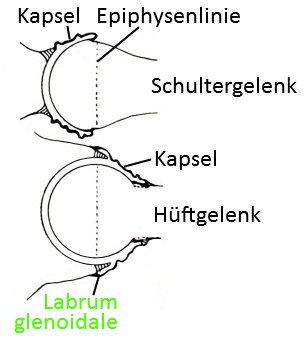
- 11.9 Comparison of the ball and socket joints hip joint – shoulder joint
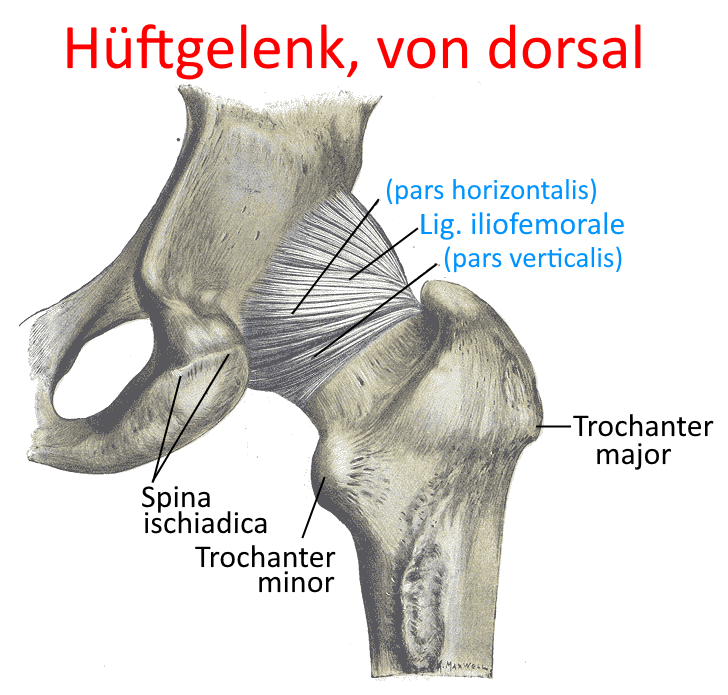
- 11.10 Position of the hip joint in the body
Image: hip joint from dorsal (linkmap)
Hip joint
The hip joint is the joint in which the lower extremity leg can be moved relative to the pelvis (and thus to the upper body), its range of motion is three-dimensional: lateral, frontal and the rotation of the leg around its axis, whereby the lateral abduction capability depends heavily on the rotation: the further the leg is turned out, the further it can be laterally abducted.
The mobility indicated for normal zero changes due to the ligament guidance and becomes more pronounced in the direction of flexion. The following is specified for normal zero:
Extension/flexion: 15/0/140
Exorotation/endorotation: 15/0/140
Abduction/adduction: 45/0/35
Articulating bones
Die Bewegungen und die ausführenden Muskeln
Die Bewegungen und die ausführenden Muskeln
Exorotation: M. gluteus maximus, M. quadratus femoris, M. obturatorius internus, m. gluteus medius und M. gluteus minimus (each with their dorsal fibres), M. iliopsoas, M. obturatorius externus, M. pectineus, Adduktor magnus with the proximal part inserting at the linea aspera, Adduktor longus, Adduktor brevis, M. piriformis, Mm. gemelli, M. sartorius, M. psoas major, M. iliacus
Endorotation: M. gluteus medius und M. gluteus minimus, (with their front fibres), M. tensor fasciae latae, M. adductor magnus (with the part that attaches to the adductor tuberosity: with flexed, abducted thigh)
Extension: M. gluteus maximus, M. gluteus medius und M. gluteus minimus (with their dorsal fibres), M. adductor magnus, M. piriformis, M. semitendinosus, M. semimembranosus, Bizeps femoris, caput longum,
obturatorius internus near Neutral Null
Flexion: M. psoas major, M. iliacus, M. rectus femoris, M. sartorius, M. tensor fasciae latae, M. pectineus, M. adductor longus, M. adductor brevis, M. gluteus medius und M. gluteus minimus, ventrale parts, M. gracilis
abduction: M. gluteus maximus (with insertion to the fascia lata), M. gluteus medius, M. gluteus minimus, M. tensor fasciae latae, M. piriformis, M. sartorius, M. obturatorius internus if the hip joint is flexed
adduction: M. adductor magnus (with attachment to the gluteal tuberosity), M. adductor longus, M. adductor brevis, M. adductor minimus, M. gluteus maximus (caudal fibres), M. semitendinosus, M. semimembranosus, biceps femoris, caput longum, M. gracilis,
M. pectineus, M. quadratus femoris, obturatorius internus, obturatorius externus
Ligaments
- Lig. capitis femoris
- Lig. cooperi
- Iliofemoral ligament
- Lig. ischiocapsulare
- Ischiofemoral ligament
- Lig. pectineum
- Pubofemoral ligament
- Lig. teres femoris
- Lig. transversum acetabuli
- Membrana obturatoria
- Iliotibial tract
outer ligaments – inner ligaments
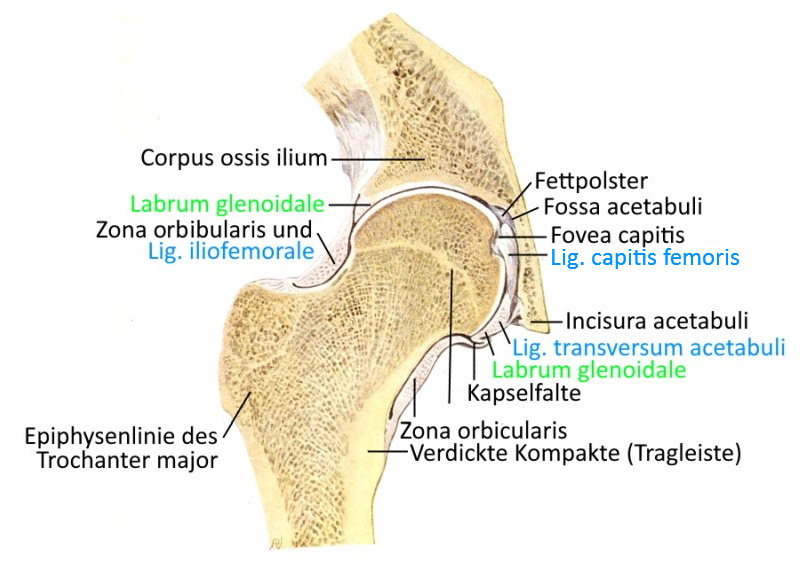
The helically arranged outer ligaments of the hip joint wrap around each other in the direction of extension and loosen their screw connection with increasing flexion, so that the range of motion there continues to increase. They radiate into the zona orbicularis, a ring-shaped ligamentous structure that is placed around the neck of the femur and prevents dislocation of the hip joint. The capitis femoris ligament, on the other hand, is considered an internal ligament because it lies deep in the hip joint.
Lig. capitis femoris
A ligament arising from the fovea capitits of the femoral head and extending to the acetabular fossa, in which an artery runs: the ramus acetabularis of the obturator artery. However, this is often atrophied in adults. This ligament does not appear to have a mechanical function. The incisura acetabuli, from which the ligament emerges, is bridged by the transverse acetabular ligament.
Images:
Linkmap: Acetabulum in context
Linkmap: Hip joint, frontal saw cut
Linkmap: Hip joint, muscles, section
Linkmap: Hip joint, medial view
Linkmap: Hip joint, unfolded
Lig. cooperi
Also known as the pectineal ligament along the pecten ossis pubis of the ramus superior ossis pubis in extension of the lacunar ligament. The ligament forms the dorsal border of the inguinal canal.
Images:
Linkmap: Trunk, abdominal wall from oblique inside
Linkmap: Pelvis, ligaments from ventral view
Linkmap: Acetabulum in context
Lig. ischiocapsulare
Old name for ischiofemoral ligament.
Images:
Linkmap: Hip ligament from dorsal
Linkmap: Acetabulum in context
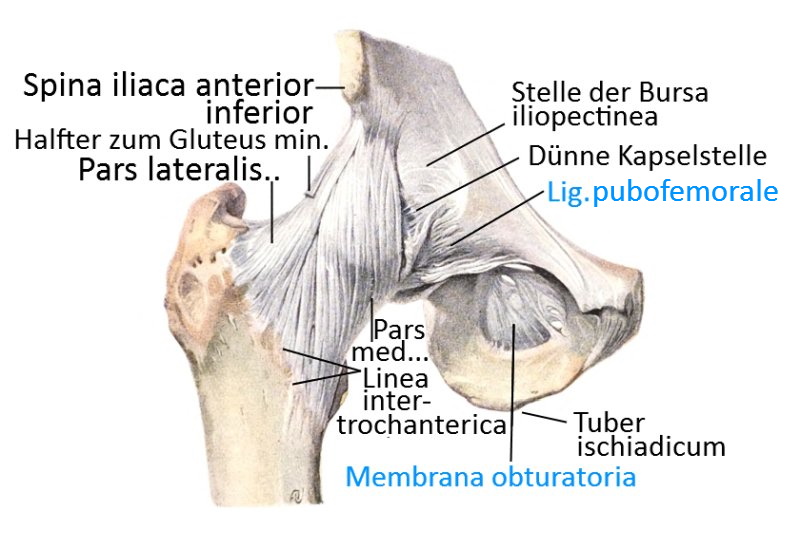
Iliofemoral ligament
The iliofemoral ligament is the strongest ligament in the human body and runs from the SIAS (spina iliaca anterior inferior) to the linea intertrochanterica femoris. It can be divided into two parts: Pars verticalis with fiber tracts and Pars horizontalis with lateral fiber tracts.
Already in standard anatomical position, this ligament inhibits hip extension so that the hip flexors have to work less.
Images:
Linkmap: Hip joint, muscles, section
Linkmap: Hip joint from medial
Linkmap: Hip joint, ligaments, dorsal view
Linkmap: Hip joint, ligaments, ventral
Linkmap: Obturatorius externus
Linkmap: Acetabulum in context
Linkmap: Dorsal view of the hip joint
Linkmap: Hip joint, frontal saw cut
Ischiofemoral ligament
Tent-shaped ligament in the dorsal hip joint from the craniolateral ischium dorsally over the femoral head to the linea intertrochanterica femoris.
Images:
Linkmap: Hip joint from dorsal
Linkmap: Acetabulum in context
Lacunar ligament
The lacunar ligament is not strictly speaking one of the ligaments of the hip joint. It runs from the inguinal ligament in the floor down to the pubic bone.
Images:
Linkmap: Trunk, lateral, profound
Linkmap: Trunk, abdominal wall from oblique inside
Linkmap: Pelvis, ligaments from ventral
Lig. orbicularis
Confluent ligament with the lateral fibers of the iliofemoral ligament, transversely encompassing the femoral head and limiting the extension.
Lig. pectineum
Another name for the cooper’s ligament.
Images:
Linkmap: Torso, abdominal wall from oblique inside
Linkmap: Pelvis, ligaments from ventral view
Linkmap: Acetabulum in context
Pubocapsular ligament
Old name for pubofemoral ligament
Pubofemoral ligament
Ligament running from the ramus superioris ossis pubis to the linea intertrochanterica femoris.
Images:
Linkmap: Hip joint from ventral view, ligaments
Linkmap: Acetabulum in context
Linkmap: Obturatorius externus
Lig. transversum acetabuli
The acetabular transverse ligament closes the gap (acetabular incisura) in the acetabular labrum.
Images:
Linkmap: Acetabulum in context
Linkmap: Hip joint, frontal saw cut
Membrana obturatoria
The obturator membrane is the thin, fibrous membrane that largely closes the obturator foramen. The origins of the obturator externus and obturator internus muscles lie on this membrane.
Images:
Linkmap: Acetabulum in context
Linkmap: Hip joint, frontal saw cut
Lig. teres femoris
Old name for capitis femoris ligament, see there.
Iliotibial tract
the strong ligamentous structure that provides the tension belt for the femur. The iliotibial tract is a pronounced reinforcement of the lateral fascia (fascia lata). Starting from the SIAS, it joins at the level of the greater trochanter with tendon fibers of the tensor fasciae latae, the gluteus maximus and the fascia of the gluteus medius. The iliotibial tract is divided in the trifurcation into
- a ventral part that radiates into the lateral retinacuum patellae
- a medial part that attaches to the Gerdy tuberosity of the lateral tibial condyle
- a dorsal part that radiates into the fascia cruris together with fibers of the biceps femoris.
The ventral part justifies the assessment that a contracted iliotibial tract promotes the tendency to(lateral) patellar dislocation.
Proximal to the knee joint, the iliotibial tract is connected to the shaft of the femur via the strong Kaplan fibers. There are three main connections: obliquely distally, above the femoral condyle, transversely to the dorsolateral femur and a spectrum of fibers between the dorsolateral femur and the Gerdy tubercle.
The iliotibial tract thus spans the hip joint laterally, meaning that the muscles radiating into it have an abducting effect. It is tensioned by the tensor fasciae latae, which has an abducting, endorotating and flexing effect in the hip joint. Depending on the angle in the knee joint, it also supports extension (less than 30° flexion) or flexion (more than 30°). During extension, the iliotibial tract slides ventrally over the lateral femoral condyle, restricted by the Kaplan fibers, and dorsally during flexion.
The part of the iliotibial tract between the Kaplan fibers and the insertion on the Gerdy tuberosity escapes the tensile influence of the tensor fasciae latae, which is why it is sometimes referred to as the tractotibial ligament or lateral anterior femorotibial ligament. tractotibial ligament or lateral anterior femorotibial ligament, which thus plays a stabilizing role for the knee joint by limiting endorotation in the flexed state, lateral gapping and the anterior drawer, i.e. the ventral translation of the tibia.
The ventral part, which radiates into the lateral retinacuum patellae, limits the movement of the patella medially, thus preventing medial dislocation of the patella.
Images:
Linkmap: Gluteus maximus
Linkmap: Hip, thigh, schematic
Linkmap: Trunk, lateral, superficial
Linkmap: Trunk, ventral, head to knee
Bursa (bursae)
Bursa bicipitis femoris superior
Rarely occurring inconstant bursa located on the ischial tuberosity between the tendon of origin of the biceps femoris and that of the semimembranosus.
Gluteofascial bursa
Bursa located between the tendon of origin of the vastus lateralis and the insertion tendon of the gluteus maximus at the level of the confluence of the insertion tendons of the gluteus maximus and the tensor fasciae lata, sometimes also referred to as the trochanteric bursa (without further addition).
Bursae gluteofemorales
Usually several bursae between the femoral shaft and the insertion area of the gluteus maximus.
Bursa ischiadica glutaei maximi
Bursa between the caudal edge of the gluteus maximus and the tuber ischiadicum
Bursa iliopectinea (also: Bursa subiliaca)
Bursa between the iliopsoas and the eminentia iliopubica of the ilium and partly the joint capsule, which is necessary due to the deflection of the iliopsoas. The bursa communicates inconstantly (14%) and then also not from birth with the underlying hip joint. It is 5-7 cm long approximately longitudinally of the leg and 2-4 cm wide (approximately transverse).
Pictures: (still without)
Bursa ischiadica obturatorii interni
Bursa between the insertion tendon of the internal obturator tendon and the cartilaginous surface of the lesser sciatic incisura, which becomes necessary due to the deflection of the tendon of the internal obturator tendon over the incisura as a hypomochlion. This bursa usually continues between the Gemelli.
Images: (still without)
Bursa obturatoris interni
Bursa between the insertion tendon of the obturator internus and the joint capsule of the hip joint.
Bursa pectinei
Bursa located between the attachment tendons of the pectineus and iliopsoas.
Bursa piriformis
Inconstant bursa between the greater trochanter and the piriformis insertion tendon
Bursa quadratus femoris
Bursa located between the attachment tendon of the quadratus femoris and the crista intertrochanterica, which serves as a hypomochlion.
Bursa recti femoris
Bursa located between the cranial edge of the acetabulum and the rectus femoris.
Bursa subcutanea ischiadica
Inconstant subcutaneous bursa between skin and tuber ischiadicum.
Bursa subcutanea sipna iliaca anterior superior
Subcutaneous bursa between skin and SIAS
Bursa subcutanea trochanterica
Subcutaneous bursa between the skin and the greater trochanter.
Bursa subtendinea iliaca (iliaca subtendinea)
Bursa located between the lesser trochanter and the pectineus and iliopsoas insertion tendons
Bursa trochanterica musculi glutei maximi
Bursa between the greater trochanter of the femur and the tendon of the gluteus maximus
Images: (still without)
Bursa trochanterica musculi glutei medii
Bursa between the cranial part of the greater trochanter of the femur and tendon of the gluteus medius
Images: (still without)
Bursa trochanterica musculi glutei minimi
Bursa between the greater trochanter of the femur and the tendon of the gluteus minimus
Images: (still without)
Bursa vesicularis semimembranosi
Bursa between the tendon of origin of the semimembranosus ventrally and the quadratus femoris and adductor longus muscles dorsally.
Bewegungen
The hip joint offers three-dimensional mobility with a large range of motion: external rotation / internal rotation, extension / flexion, abduction /adduction. The movements and their executing muscles in detail:
External rotation M. gluteus maximus, M. quadratus femoris, M. obturatorius internus, .m. gluteus medius, M. gluteus minimus, M. iliopsoas, M. obturatorius externus, M. pectineus, Adduktor magnus, Adduktor longus, Adduktor brevis, M. piriformis, Mm. gemelli, M. sartorius, M. psoas major, M. iliacus
Internal rotation M. gluteus medius und M. gluteus minimus, (mit ihren vorderen Fasern), M. tensor fasciae latae, M. adductor magnus (mit dem Teil, der am tuberculum adductorium ansetzt: bei flektiertem, abduziertem Oberschenkel)
Extension M. gluteus maximus, M. gluteus medius, M. gluteus minimus, M. adductor magnus, M. piriformis, M. semitendinosus, M. semimembranosus, Bizeps femoris, caput longum, obturatorius internus nahe Neutral Null
Flexion M. psoas major, M. iliacus, M. rectus femoris, M. sartorius, M. tensor fasciae latae, M. pectineus, M. adductor longus, M. adductor brevis, M. gluteus medius und M. gluteus minimus, je ventrale Anteile, M. gracilis
Abduction M. gluteus maximus (mit Ansatz an der fascia lata), M. gluteus medius, M. gluteus minimus, M. tensor fasciae latae, M. piriformis, M. sartorius, M. obturatorius internus wenn das Hüftgelenk flektiert ist
Adduction M. adductor magnus, M. adductor longus, M. adductor brevis, M. adductor minimus, M. gluteus maximus, M. semitendinosus, M. semimembranosus, Bizeps femoris, caput longum, M. gracilis, M. pectineus, M. quadratus femoris, obturatorius internus, obturatorius externus
Pathology
- Osteoarthritis
- Perthes‘ disease
- Impingement(femoroacetabular impingement)
- M. Ankylosing spondylitis
- Secondary conditions due to altered statics and kinetics in pathology of the foot or knee joint
- Fracture of the femoral neck
- Groin pain: There are a number of sports in which there is a significant risk of groin pain. For example, 60% of footballers suffer from it during their career, and handball and volleyball players are also predisposed. Another group are those who play racket sports and endurance sports such as cross-country skiing. Weight training, gymnastics and fencing can also lead to groin pain. The type of exposure causing the pain varies across all these sports. While ball sports are more prone to adductor injuries from abduction to muscle tears, in cross-country skiing it is the incorrect loading of periarticular structures of the hip joint that are affected by errors in running style, leg length discrepancies or inadequate equipment.
- Functional disorders include insertion tendinopathies, which are based on muscular imbalances or shortening as well as overloading, but also blockages of the sacroiliac joint.
- Structural disorders: Arthroses of the hip joint or sacroiliac joint and disorders of the symphysis belong to the structural disorders, as well as disorders of the apophyses and epiphyses in children and Perthes‘ disease and van Neck’s disease as aseptic necroses.
The sports history of those affected by groin pain often includes running or sprinting sports including hurdling, walking and jumping in various forms, but also martial arts including fencing. Acute injuries are often muscle or tendon ruptures. Chronic complaints that slowly creep in are caused by overloading the joints or tendon insertions. The localization of pain can sometimes be misleading, as disorders of the hip joint can radiate into the knee, just as disorders of the sacroiliac joint can radiate into the groin. Changes in the training program, intensity or level, as well as other factors, are also important for the medical history. Painful pressure in areas of insertions is indicative of insertion tendinopathy. Abduction restrictions are non-specific and are usually due to contracted muscles. Stretching pain or contraction pain, i.e. pain on exertion, in turn indicate insertion tendinopathies. Painful internal rotation deficits are usually due to articular disorders: capsulitis, arthritis or arthrosis. Complex movement disorders usually indicate articular disorders. Leg length discrepancies must be determined reliably. A variable leg length difference, which is sometimes apparent and sometimes not, very often indicates a disorder of the sacroiliac joint, just like the positive spine test (retraction phenomenon) and /or the forward movement phenomenon. Common insertion tendinopathies include those at the origin of the adductor longus and the gracilis, those at the origin of the rectus femoris, those at the insertion of the rectus abdominis and symphysitis.
Tests
Tests of the hip joint
General tests
- Mennell test (distinction hip joint – sacroiliac joint)
- figure-4-sign (Patrick test, Faber test)
- 4-er-Zeichen test
- Trendelenburg
- Duchenne-sign (Watschelgang)
Pelvic torsion
DGS (Deep Gluteal Syndrome / Piriformis syndrome)
- Piriformis test
- FAIR Test (Flexion, Abduction, Internal Rotation) for piriformis
- Active piriformis test
- Seated piriformis stretch test
- Beatty maneuver
- Freiberg sign
- Pace Manöver
- Heel contralateral knee maneuver
- JAGAS test
- Filler-sign
posterior labrum
anterior labrum
Hip dysplasia
- Galeazzi (Allis) test (Leg length difference, hip dysplasia)
- Ortoani/Barlow
- Kalchschmidt dysplasia test
mixed
- FADDIR test (Hip impingement (FAI) or labrum damage)
- Anvill test (Coxarthrosis, coxitis, loose Endoprosthesis)
- McCarthy-Test (Hip impingement (FAI) or labrum damage)
Tests of the movement directions
Abduction
External rotation
- definite yoga hip external rotation test in half lotus forward bend
- definite yoga hip external rotation test in hip opener 3
- definite yoga rotational side discrepancy in savasana
Tests of the spanning muscles
Hip flexor contracture
Small glutes
Pictures
Hip joint, transverse incision
hip joint, medial
hip joint, dorsal
hip joint, ventral
hip joint, unfolded
Acetabulum in context (image links to linkmap)
hip joint from ventral (image links to linkmap)
hip joint from ventral, saw cut (image links to linkmap)
Comparison of the ball and socket joints hip joint – shoulder joint
Position of the hip joint in the body