yogabook / joints / knee joint
Contents
- 1 Image: Knee from the side
- 2 Knee joint
- 3 Articulating bones
- 4 Partial joints
- 5 The movements and the muscles involved
- 6 Ligaments
- 6.1 Patellar ligament
- 6.2 Collateral ligaments Ligg. collateralia
- 6.3 Cruciate ligaments Ligg. cruciata
- 6.4 Meniscofemoral ligaments Ligg. meniscofemoralia
- 6.5 Lig. popliteofibulare (LPF)
- 6.6 Lig. popliteum arcuatum
- 6.7 Lig. popliteum obliquum (lig. bourgery)
- 6.8 Lig. collaterale mediale posterius (posterior oblique ligament, POL, posterior inner ligament, medial capsular ligament)
- 6.9 Lig. capitis fibulae anterius
- 6.10 Lig. capitis fibulae posterius
- 6.11 Lig. transversum genus
- 6.12 Retinaculum patellae
- 6.13 Medial capsular ligament
- 7 Bursa (bursae)
- 7.1 Bursa anserina
- 7.2 Bursa bicipitis femoris inferior
- 7.3 Bicipitogastrocnemial bursa
- 7.4 Bursa capitis tibialis gastrocnemii
- 7.5 Bursa gastrocnemiosemimembranosa
- 7.6 Bursa infrapatellaris profunda
- 7.7 Bursa infrapatellaris subcutanea
- 7.8 Bursa Lig. cruciatorum
- 7.9 Medial patellar bursa
- 7.10 Lateral patellar bursa
- 7.11 Bursa poplitei
- 7.12 Bursa sartorii proprii
- 7.13 Bursa subaponeurotica praepatellaris
- 7.14 Bursa subcutanea epicondyli tibialis
- 7.15 Bursa subcutanea praepatellaris
- 7.16 Bursa subcutanea tuberositatis tibiae
- 7.17 Bursa subfascialis praepatellaris
- 7.18 Bursa subtendinea gastrocnemii medialis
- 7.19 Bursa subtendinea gastrocnemii lateralis
- 7.20 Bursa subtendinea praepatellaris
- 7.21 Bursa subtendinea semimembranosi (musculi semimembranosi, semimembranosa tibialis)
- 7.22 Suprapatellar bursa
- 7.23 Bursa suprapatellaris intermuscularis accidentalis
- 8 Further structures
- 9 Movements
- 10 Pathology
- 11 Tests
- 11.1 Tests of the knee joint
- 11.1.1 Meniscus
- 11.1.2 Medial collateral ligament
- 11.1.3 Lateral collateral ligament
- 11.1.4 Cruciate ligaments
- 11.1.5 ITBS (Runners knee)
- 11.1.6 IT-Band (Tractus iliotibialis) Verkürzung
- 11.1.7 Chondropathia patellae
- 11.1.8 Patella mixed
- 11.1.9 Hoffa-syndrome
- 11.1.10 Joint effusion
- 11.1.11 Q-angle
- 11.1.12 (Posterolateral Instability)
- 11.1.13 Patellaluxation/-subluxation
- 11.1.14 Plica-Syndrom
- 11.1.15 mixed
- 11.2 Tests of the movement directions
- 11.3 Tests of the spanning muscles
- 11.1 Tests of the knee joint
- 12 Images
- 12.1 Knee from dorsal, ligaments
- 12.2 Knee from dorsal
- 12.3 Knee from dorsal, capsule
- 12.4 Knee from ventral
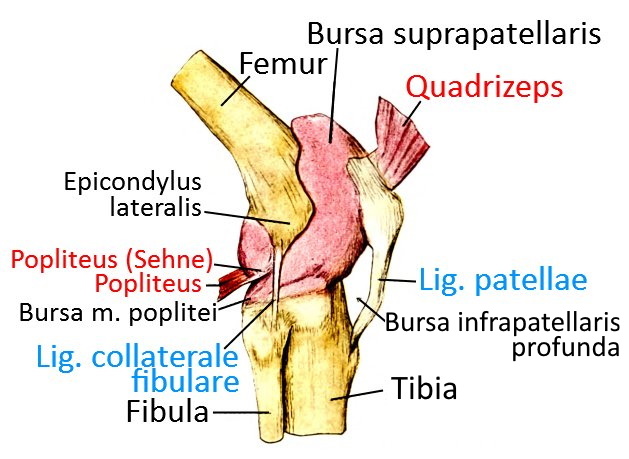
- 12.5 Knee from ventrolateral
- 12.6 Knee from lateral
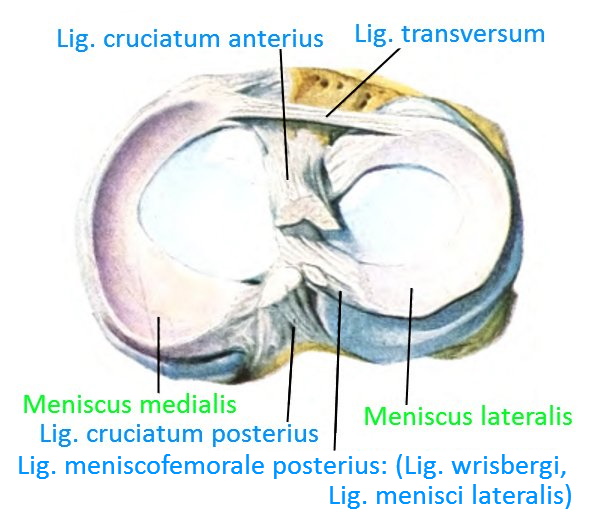
- 12.7 Knee transversal
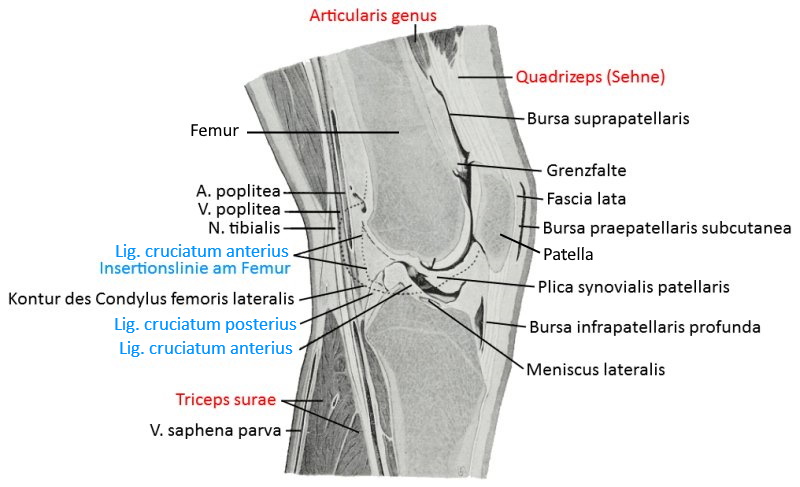
- 12.8 Knee, saggital
- 12.9 ventral view in 90° flexion (image links to linkmap)
- 12.10 Lateral view in 45° flexion with expanded bursae (image links to linkmap)
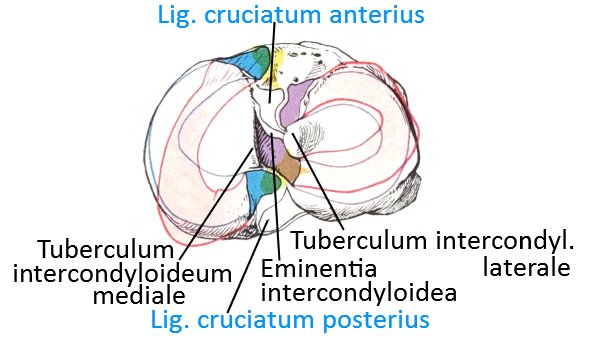
- 12.11 Menisci on tibia from cranial (image links to linkmap)
- 12.12 Menisci with loaded rotation (image links to linkmap)
Image: Knee from the side
Knee joint
The knee joint is usually understood to be the hinge joint in which the lower leg (more precisely the tibia) moves relative to the upper leg (more precisely the femur); this is the femorotibial articulation. As with the elbow joint, the main movement is flexion/extension. In addition, when the knee is flexed, the lower leg can rotate a little in relation to the thigh, but the movement is different from that of the forearm, as there is no overturning(pronation) of two bones and the range of movement is significantly smaller. The axis of rotation of the tibia runs through the medial meniscus, as this is fused with the medial ligament. In principle, translational movements in sagittal and transverse directions are also possible between the two bones, the tibia and femur, as well as compression/distraction movements, all of which are limited by the ligamentous structure of the knee joint. The physiological range of motion of the knee joint in the direction of flexion/extension is given as 5-0-150, whereby the 150° applies to active flexion due to passive insufficiency, while much more can be achieved passively. The degree of hyperextensibility of the knee joint varies from 0° to over 5°, whereby pain can occur from an individually different angle, but does not have to. The range of motion in the direction of rotation is specified as 10° internal rotation and 25° external rotation.
To stabilize the knee joint in movement and posture, the knee joint is well equipped proprioceptively with many sensors in the joint capsule-ligament apparatus. The information from the proprioceptors is processed in a neuronal network in the spinal cord and corresponding muscle actions are initiated. Therefore, the loss of a group of proprioceptors, such as the mechanoreceptors in the anterior cruciate ligament, does not directly result in a complete loss of the increased innervation of the hamstrings in the event of ventral translation of the tibia, but it does result in a reduced response and increased time lag – which causes increased wear and tear during intensive use of the knee joint.
The external angle of the two shafts of the femur and tibia in the frontal plane is physiologically 174° (and not 180°, due to the CCD angle in the femur) – if it falls below 171°, this is referred to as a knock-knee (genu valgum), if it exceeds 180° it is referred to as a bow-leg (genu varum), both of which are pathological and cause damage to the musculoskeletal system, especially the lower extremities. This is a problem that has so far been unsolvable for surgical plasty after tears, which is why postoperative physiotherapy training adapted to the new situation is of great importance.
Capsule-tape apparatus
The extensive apparatus of ligaments and joint capsule lined with capsular ligaments, which in the case of the knee joint is extremely important for stability, can be divided into 4 fractions, which have an active and a passive aspect:
Media complex
passive:
- Medialretinaculum
- Lig. collaterale mediale
- Lig. popliteum obliquus (Lig. obliquus posterior, POL)
- Medial capsular ligament
- Medial half of the dorsal joint capsule
- Inner meniscus
- Anterior cru ciate ligament (ACL) and posterior cruciate ligament (PCL)
- Bony specifics of the tibial plateau and the medial femoral condyle
active:
- Vastus medialis
- Vastus medialis obliquus
- M. sartorius (Pes anserinus superficialis)
- M. gracilis (Pes anserinus superficialis)
- M. semitendinosus (Pes anserinus superficialis)
- M. semimembranosus (Pes anserinus profundus)
- M. gastrocnemius, Caput mediale
Lateral complex
passive:
- Joint capsule
- Lateral capsular ligament
- Lateral patellarretinaculum
- Lateral collateral ligament
- Tractus iliotibialis, also as reserve extensor apparatus
- Tractotibial ligament
- Kaplan fibers
active:
Central complex
passive:
- posterior cruciate ligament
- anterior cruciate ligament
- Lig. meniscofemorale anterius
- Lig. meniscofemorale posterius
- Innenmeniskus
- Außenmeniskus
Ventral complex
passive:
- Lig. patellae
- Retinaculum patellae mediale
- Retinaculum patellae laterale
- Corpus adiposum infrapatellare (Hoffa’scher Fettkörper)
active:
Dorsal complex
passive:
- Dorsal capsule
- Lig. popliteum arcuatum
- Lig. popliteum obliquum
active:
Patella
The patella, which is flexibly supported by the femur(femoropatellar sliding bearing), is not directly associated with the knee joint as the femorotibial articulation, but is important for the transmission of force from the quadriceps. The patella and femur form a real joint here, the femoropatellar articulation. The transmission of force via the patella increases the lever arm and thus the possible torque in the knee joint for extension.
Around 50% of the distal tendon fibers of the quadriceps insert at the cranial patellar pole, the remaining fibers of the attachment tendon cover the patella in the direction of the tibial tuberosity or run medial or lateral to the patella as the medial patellarretinaculum or lateral patellarretinaculum.
Articulating bones
Partial joints
- Femorotibial joint Art. femorotibialis
- Femoropatellar joint (femoropatellar articulation, femoropatellar sliding bearing)
Femorotibial joint
The femorotibial joint is the joint that is usually meant when talking about the „knee joint“, i.e. the joint between the femur and tibia. It is a joint that combines the properties of a pivot joint (trochoidea) and a hinge joint (ginglymus), i.e. a combination of rolling and sliding movement of the two joint bodies. This connection is also known as a trochogingly joint or bicondylar joint. Adequate stability of the joint therefore requires good ligament guidance, which is provided here in the form of the cruciate and collateral ligaments.
Femoropatellar sliding bearing Art. femoropatellaris
The femoropatellar sliding bearing is the joint in which the patella rests flexibly on the femur, which transmits the contraction force of the quadriceps. During extension and flexion of the knee joint, the patella moves on the femur, as the patellar ligament is a non-elastic band that keeps the lower patellar pole at an approximately constant distance from the tibial tuberosity when tensed, whereas the quadriceps, as a contractile muscle, changes its length over a large range.
When the knee joint is flexed, this results in considerable contact pressure of the patella against the femur. The wear caused by overuse or uneven movement of the patella, for example when the lower leg rotates during extension or flexion, can lead to damage to the retropatellar cartilage(PFPS).
This joint is often affected by retropatellar cartilage disorders, for example in the form of chondropathia patellae (PFPS) or retropatellar arthrosis. Both phenomena are favored by:
- Incongruence of the joint surfaces
- Anomalies such as lack of height of the ridge (intercondylar sulcus) between the joint surfaces with the femoral condyles
- Relative hypertonus of the vastus lateralis or rectus femoris
- Overuse
A closer look reveals 3 rotational and 3 translational dimensions of movement in the femoropatellar sliding bearing:
- Translation superior-inferior, the most important physiological dimension of movement
- Rotation around the transverse medio-lateral axis of the patella due to the non-constant radii of the femoral condyles; this movement is referred to as flexion
- medio-lateral translation due to the variable, tolerance-dependent guidance of the fin of the patella in the trochlea (sulcus intercondylaris), „ML Shift“
- Rotation around the anterior-posterior transverse line perpendicular to the patella
- Rotation around the superior-inferior axis (tilt)
- anterior-posterior translation
The movements and the muscles involved
Extension: M. quadriceps femoris (almost exclusively) thereby
M. rectus femoris with stretched hip joint more powerful,
M. tensor fasciae latae (insignificant)
Flexion: M. semimembranosus, M. semitendinosus, M. biceps femoris, M. gracilis, M. sartorius, M. poplieteus, M. gastrocnemius, M. plantaris. The tensor fasciae latae has a bending effect on the knee joint via the iliotibial band with the knee bend more than 30°.
Internal rotation of the lower leg: M. semimembranosus, M. semitendinosus, M. gracilis, M. sartorius, M. poplieteus
External rotation of the lower leg: M. biceps femoris
Ligaments
- Lig. collaterale mediale
- Lig. collaterale laterale
- Lig. cruciatum anterius
- Lig. cruciatum posterius
- Ligg. meniscofemoralia
- Lig. meniscofemorale anterius (Humphrey)
- Lig. meniscofemorale anterius (Wrisberg)
- Lig. patellae
- Lig. popliteum obliquum (posterior oblique ligament, POL, Bourgery)
- Lig. capitis fibulae anterius
- Lig. capitis fibulae posterius
- Lig. transversum genus
- Retinaculum patellae
- Retinaculum patellae laterale
- Retinaculum patellae mediale
- Retinaculum patellae transversale laterale
- Retinaculum patellae transversale mediale
Patellar ligament
The approx. 5-6 mm thick ligament is a capsular ligament that transmits the contraction force of the quadriceps from the lower edge of the patella(caudal patellar pole) to the tibia, where it inserts at the tibial tuberosity. If the quadriceps are not under tension, the patellar ligament is slack and could become trapped in the joint space when the knee joint is largely extended. This is why the Hoffa’s adipose body (corpus adiposum infrapatellare) lies behind(dorsally or profoundly) the patellar l igament, which prevents this due to its volume. A change in Hoffa’s fat body can lead to Hoffa’s syndrome, which usually only occurs secondarily.
Images:
Linkmap: Knee joint ventrolateral
Linkmap: Lateral knee joint
Linkmap: Knee joint, sagittal section
Linkmap: Tibia
Linkmap: Bones of the lower leg
Linkmap: Trunk ventral head to knee
Linkmap: Trunk lateral, superficial
Linkmap: Knee joint, 90° inflected
Linkmap: Lateral knee joint, bursa
Collateral ligaments Ligg. collateralia
the medial and lateral collateral ligaments that run longitudinally on the medial and lateral side of the knee joint, which tighten when the knee joint is extended due to the shape of the condyles and thus increasingly prevent the endo-and exorotation of the lower leg in the knee joint: the medial collateral ligament and the lateral collateral ligament (fibular). Another important task of the collateral ligaments is to absorb varusand valgus-likemovements and corresponding forces.
Lig. collaterale mediale (inner collateral ligament, lig. collaterale tibiale)
broad, flat ligament, approx. 9-11 cm long, which runs slightly offset dorsally on the medial side of the knee joint and stabilizes it against valgus movement. It runs from the epicondylus medialis femoris to the condylus medialis tibiae. It has an anterior and a posterior part, both of which diverge slightly distally. The more profound parts are fused with the medial meniscus. The proximal part is connected to the medial patellarretinaculum, the distal part merges into the popliteal oblique ligament and the dorsomedial capsule. The distal parts are partly overlaid by the pes anserinus and its attached muscles, which is why abursa (bursa anserina) buffers between them to reduce shear forces. A bursa separates the medial collateral ligament from the more profound structures, namely the joint capsule, which is reinforced with a capsular ligament, and the medial meniscus. The medial collateral ligament not only limits the valgus movement of the tibia and thus prevents medial gapping, but together with the fibular collateral ligament ( lateral collateral ligament) also limits the exorotation of the lower leg in the knee joint, which is why it is at risk in breaststroke athletes. The classic valgus stress test of the knee joint tests the sufficiency of the ligament. Due to the complex anatomy of the medial collateral ligament, the results of reconstructive surgery are often unsatisfactory. In particular, calcifications, which are more likely to occur the longer the knee joint is immobilized, often lead to functional deficits and restricted mobility.
Images:
Linkmap: Knee joint, dorsal, ligaments
Linkmap: Knee joint, dorsal
Linkmap: Knee joint, dorsal, capsule
Linkmap: Knee joint ventrolateral
Linkmap: Knee joint, 90° flexed
Lateral collateral ligament (outer collateral ligament, fibular collateral ligament)
The outer or fibular collateral ligament is a strong round ligament 5-7 cm long and, unlike the inner collateral ligament, has no connection to the meniscus. It is largely covered by the biceps femoris. It runs from the lateral femoral epicondyle, just below the sulcus of the popliteus tendon, to the head of the fibula. It splits the attachment tendon of the biceps femoris into an anterior and a posterior branch. The bursa subtendinea musculi bicipitis femoris inferior lies between the lateral collateral ligament and the biceps femoris. The popliteus tendon runs between the lateral collateral ligament and the lateral capsule. The ligament secures the knee joint against varus movement and limits exorotation.
Images:
Linkmap: Dorsal view of the knee joint, ligaments
Linkmap: Knee joint dorsal
Linkmap: Knee joint dorsal, capsule
Linkmap: Knee joint, 90° inflected
Linkmap: Lateral knee joint
Linkmap: Lateral knee joint, bursa
Cruciate ligaments Ligg. cruciata
The two ligaments that run intra-articularly but retrosynovially in the knee joint and prevent the tibia from shifting ventrally or dorsally in relation to the femur: the anterior cru ciate ligament and the even stronger posterior cruciate ligament. In terms of developmental history, they have migrated into the knee joint from the dorsal side. If they are damaged, unphysiological displacements occur, resulting in instability during movement and increased wear of the knee joint. Damage such as overstretching and tears can be recognized by the anterior or posterior drawer effect. In the English literature, theanterior cruciate ligament is referred to as the ACL(anterior cruciate ligament) and the posterior cruciate l igament as the PCL(posterior cruciate ligament). The name cruciate ligament comes from the fact that the two cruciate ligaments with their different directions of tension cross in the middle of the knee joint and develop complex biomechanics. To a limited extent, the cruciate ligaments also restrict the varus and valgus movements of the knee joint. As they wrap around each other during endorotation of the lower leg in the knee joint, they limit these movements. Tension and release as well as tightening and loosening of the cruciate ligaments are important for their metabolism.
Lig. cruciatum anterius (ACL, LCA, anterior cruciate ligament, anterior cruciate ligament)
The anterior cruciate ligament is probably the most important ligament for stabilizing the knee joint in the sagittal direction and, together with the posterior cruciate ligament, which runs in the opposite direction, secures it against translation of the tibia. Particularly in a slightly flexed position of the knee joint (approx. 20-30°), it strongly secures the tibia against forward displacement. Both cruciate ligaments together limit the final rotation of the lower leg in the knee joint. The anterior cruciate ligament also limits the extension of the knee joint. It runs from the lateral wall of the intercondylar fossa of the lateral femoral condyle to the proximal medial tibia at the anterior intercondylar area in front of the intercondylar eminence, just ventral to the medial intercondylar tubercle between the insertions of the anterior menisci. It therefore runs from posterior-superior-lateral to anterior-inferior-medial. Some fibers insert at the meniscal root of the medial meniscus. A distinction is made between two bundles according to origin and insertion: an anterior (anteromedial) bundle, which runs from the intercondylar line to the anterior tibial plateau, and a posterior (posterolateral) bundle, which runs from the border between the bone and cartilage of the femoral condyle to the posterior area of the tibia, close to the medial meniscus. An intermediate bundle can also be identified. The LCA is supplied with arterial blood from both sides, but the center and the insertion areas are usually not supplied with arterial blood. It has many mechanoreceptors (Golgi type III receptors, Ruffini corpuscles, Pacini type II corpuscles and free nerve endings), which serve the proprioception of the knee joint, but also the activation of knee joint stabilizing muscles, such as the hamstrings, which also pulls the tibia dorsally. In the event of ruptures of the LCA or replacement with a plastic, this function is no longer available, which puts more strain on the plastic than on the native cruciate ligament and leads to increased ventral translation and increased wear. If the ACL is damaged, the rolling-sliding mechanism of the knee joint is disrupted and damage occurs primarily to the posterior horns of the menisci, later also to cartilage damage to the tibia and femur, which can also be detected radiologically.
Images:
Linkmap: Knee joint from the dorsal side, ligaments
Linkmap: Dorsal knee joint, capsule
Linkmap: Knee joint ventral
Linkmap: Knee joint transversal
Linkmap: Knee joint, 90° inflected
Linkmap: Knee joint, menisci
Linkmap: Knee joint, distortion of the menisci during torsion
Posterior cruciate ligament (PCL, posterior cruciate ligament)
The posterior cruciate ligament runs from the inside of the medial femoral condyle diagonally to the lateral distal to the posterior intercondylar area, i.e. from ventral-cranial-medial to dorsal-caudal-lateral and thus runs transversely to the anterior cruciate ligament. A longer, stronger anterolateral and a shorter, less strong dorsomedial fiber bundle can be distinguished.
dorsomedial fiber bundle. The quadriceps, innervated by the proprioceptors of the longitudinal retinaculi of the patella, which radiate from its fibers, work to prevent excessive strain on the posterior cruciate ligament. Good development of the two important quadriceps parts, vastus medialis and vastus lateralis, from which these retinaculi radiate, is therefore important for an athlete.
Images:
Linkmap: Knee joint from dorsal, ligaments
Linkmap: Dorsal knee joint, capsule
Linkmap: Knee joint ventral
Linkmap: Knee joint transversal
Linkmap: Knee joint, 90° inflected
Linkmap: Knee joint, menisci
Linkmap: Knee joint, distortion of the menisci during torsion
Meniscofemoral ligaments Ligg. meniscofemoralia
The meniscofemoral ligaments support the posterior cruciate ligament and occur inconsistently. The Humphrey ligament stretches when the knee joint is flexed and the Wrisberg ligament stretches when the knee joint is extended. If the posterior cruciate ligament is damaged, they can partially take over its function. They stabilize the knee joint with regard to posterior translation of the tibia:
- the Wrisberg ligament (posterior meniscofemoral ligament), which can be differentiated into three types and lies dorsal to the posterior cruciate ligament, accounting for approx. 70%.
- the Humphrey ligament (anterior meniscofemoral ligament) lying ventral to the posterior cruciate ligament in about 50% of cases
Information on the presence of the ligaments varies in the literature. The Wrisberg ligament can be quite pronounced. In 61% of cases, both meniscofemoral ligaments are present. They then wrap around the posterior cruciate ligament. The Humphrey ligament stretches in flexion, the Wrisberg ligament in extension of the knee joint. Both tighten when the lower leg is in endorotation. Their most important task is to prevent the posterior horn of the lateral meniscus from becoming trapped.
Images:
Linkmap: Knee joint from dorsal, ligaments
Linkmap: Knee joint transversal
Linkmap: Knee joint, menisci
Anterior meniscofemoral ligament: „Humphrey ligament„
The anterior meniscofemoral ligament runs from the posterior meniscal root of the lateral meniscus in front of the posterior cruciate ligament to the inner surface of the medial femoral condyle.
Posterior meniscofemoral ligament: „Wrisbergligament„
Like the anterior meniscofemoral ligament, the posterior meniscofemoral ligament runs from the posterior meniscal root of the lateral outer meniscus to the medial femoral condyle, but runs behind the posterior cruciate ligament. An existing Wrisberg ligament must not be misinterpreted radiologically as a tear of the meniscus. The origin of the three types of Wrisberg ligament is identical, but they differ in their attachment:
- Posterior horn of the medial meniscus (most common form)
- fan-shaped from the meniscus to further medial to the tibia
- without attachment to the meniscus, only to the tibia, sometimes considered part of the posterior cruciate ligament as it is not connected to the meniscus
Images:
Linkmap: Knee joint, meniscus
Lig. popliteofibulare (LPF)
The popliteofibular ligament (LPF) radiates from the head of the fibula into the tendon of the popliteus.
Lig. popliteum arcuatum
The popliteus arcuate ligament is an extracapsular dorsal ligament of the knee joint that runs from the posterior edge of the head of the fibula obliquely in a craniomedial direction and crosses the popliteus insertion, which it attaches to the joint capsule. It covers the dorsolateral joint area in a fan shape and runs partly parallel to the lateral collateral ligament.
Images: (still without)
Lig. popliteum obliquum (lig. bourgery)
The oblique popliteofibular ligament, which runs from the posterior edge of the head of the tibia obliquely craniolaterally to the upper edge of the intercondylar fossa and to the posterior surface of the femur, taking up the tendon of the semimembranosus in a lateral split. It reinforces the dorsal capsule of the knee joint. In extension of the knee joint it is taut and prevents medial and lateral gapping, in flexion it is relaxed. Because of its connection to the semimembranosus, it still contributes to the stability of the joint even when relaxed in flexion. This ligament can have connections to the medial collateral ligament, the popliteus tendon and the dorsal capsule.
Images:
Linkmap: Knee joint dorsal
Linkmap: Knee joint, sagittal section
Lig. collaterale mediale posterius (posterior oblique ligament, POL, posterior inner ligament, medial capsular ligament)
The POL moves from the adductor tuberosity in three different lines:
- to the posterior edge of the tibia and medial meniscus (this is the main traction)
- to the tendon of the semimembranosus (medial fiber tract)
- merges with the tendon of the semimembranosus in the lig. popliteum obliquum
It stabilizes against valgus stress and exorotation, both in extension (together with the medial collateral ligament) and in flexion (in conjunction with the tensed semimembranosus). Together with the posterior horn of the medial meniscus, the ACL and the medial collateral l igament, it protects against excessive translation of the tibia in the sagittal direction.
Lig. capitis fibulae anterius
Ventral ligament of the proximal tibiofibular joint that reinforces the capsule. It runs from the ventral caput fibulae and facies articularis fibularis of the lateral tibial condyle. The anterior capitis fibulae ligament is stronger than its posterior equivalent, the posterior capitis fibulae ligament.
Images:
Linkmap: Knee joint from dorsal, ligaments
Linkmap: Knee joint, 90° flexed
Lig. capitis fibulae posterius
Dorsal ligament of the proximal tibiofibular joint that reinforces the capsule dorsally. It is less pronounced than its ventral counterpart, the anterior capitis fibulae ligament.
Images: (still without)
Lig. transversum genus
The variably pronounced transverse genus ligament is an intra-articular ligament that connects the two anterior horns of the menisci(inner meniscus and outer meniscus). No significant function has yet been demonstrated.
Linkmap: Knee joint, 90° flexed
Linkmap: Knee joint, menisci
Linkmap: Knee joint, transverse
Retinaculum patellae
The retinaculum patellae consists of two individual longitudinal ligaments, a lateral retinaculum patellae laterale and a medial retinaculum patellae mediale, which surround the patella from the outside and hold it in position.
lateral trans verse and in 30% also a medial transverse retinaculum. The transverse retinaculi lie deeper than the longitudinal retinaculi. Patelladislocations are therefore generally prevented if the ligamentous apparatus is undamaged. The longitudinal fibers of the patellar retinaculum can transfer a residual contraction force of the quadriceps to the tibia in the event of a tear in the patellar ligament and thus maintain a small residual extensor function, which is why they are referred to as the reserve extensor apparatus.
Medial patellar retinaculum (MPFL)
The medial patellar retinaculum originates from the tendon fibers of the medial vastus, which do not attach to the cranial patellar pole and do not cover the patella. They extend to the medial edge of the patella and the tibial collateral ligament as well as to the medial condyle of the tibia medial to the tibial tuberosity and the patellar ligament.
Images: (still without)
Lateral patellar retinaculum
The lateral patellar retinaculum arises from the tendons of the lateral vastus and the rectus femoris and extends to the lateral edge of the patella and the collateral fibular ligament as well as to the lateral condyle of the tibia lateral to the tibial tuberosity and the patellar ligament.
Images:
Linkmap: Knee joint ventrolateral
Retinaculum patellae, transverse parts
In addition to the retinaculum patellae laterale and retinaculum patellae mediale, there is often a lateral transverse part(retinaculum patellae transversale laterale) and in 30% a medial transverse part(retinaculum patellae transversale mediale).
Images: (still without)
Lateral transverse patellar retinaculum (LPTL)
The transverse lateral part originates from tissue of the iliotibial tract and runs on the one hand without connection to the lateral epicondyle as the lateral patellofemoral ligament to the mid-superior lateral edge of the patella and on the other hand runs further caudally (lower lateral edge of the patella) as the lateral patellofemoral ligament. Further cranially there is a connection between the patella and the lateral condyle of the femur via the Kaplan fibers.
Images: (still without)
Lateral patellofemoral ligament
The fiber tract of the transverse lateral patellarretinaculum described above from the mid-superior lateral edge of the patella to the iliotibial tract.
Lateral patellotibial ligament
The fiber tract of the transverse lateralretinaculum patellae from the lower lateral edge of the patella to the iliotibial tract described above.
Kaplan fibers
the cranial connection of the lateral patellarretinaculum to the lateral condyle of the femur.
Retinaculum patellae transversale mediale (patellotibial ligament)
The transverse medial part consisting of fibers of the tendon of the vastus medialis, which extend to the medial edge of the patella and to the femur lateral to the medial collateral ligament.
Images: (still without)
Medial patellofemoral ligament
the cranial (femoral) part of the retinaculum patellae transversale mediale
Medial patellotibial ligament
the caudal (tibial) part of the transverse medial patellarretinaculum
Medial capsular ligament
The medial capsular ligament, which runs from cranial to caudal, represents the fiber-reinforced middle third of the medial capsule. It is firmly fused to the base of the meniscus. The cranial part is referred to as meniscofemoral, the caudal part as meniscotibial. During
extension of the knee joint it is taut and becomes slack even with slight flexion, only to tighten again with further flexion, so that it protects against valgus stress and excessive exorotation during extension and further flexion.
Bursa (bursae)
There are many bursae in the knee area, which is often subject to high mechanical stress. Some of these are constant, others are caused by corresponding stimuli/stress, such as frequent, prolonged kneeling or activities on the knees or in a squatting position. Bursitis can also develop here if overloaded, especially in the:
- Bursa subcutanea praepatellaris „Housemaid’s Knee“
- Bursa subcutanea infrapatellaris due to frequent or prolonged kneeling „clergyman’s knee“, „priest’s knee“
- Bursa subcutanea tuberositatis tibiae
These bursitis often occur in craftsmen, roofers, tilers, carpet layers, fitters and cleaners with kneeling activities as well as clerics whose religion requires kneeling prayers.
Bursa anserina
in the area below the knee joint between the inner collateral ligament and the common insertion tendon of the semitendinosus, sartorius and gracilis on the pes anserinus superficialis. The bursa ensures that the structures can move relative to each other.
(Breast) swimmers and runners are particularly affected by bursitis.
Pictures: (still without)
Bursa bicipitis femoris inferior
Constant, non-communicating bursa between the lateral collateral ligament and the insertion tendon of the biceps femoris.
Images:
Linkmap: Poplitea profunda
Bicipitogastrocnemial bursa
Inconstant bursa located between the insertion of the biceps femoris and the lateral caput of the gastrocnemius.
Images:
Linkmap: Poplitea profunda
Bursa capitis tibialis gastrocnemii
Other name for the bursa subtendinea gastrocnemii medialis
Bursa gastrocnemiosemimembranosa
Bursa between the medial head of the gastrocnemius and the insertion tendon of the biceps femoris, which in 1/3 of cases communicates with the inconstant bursa subtendinea gastrocnemii medialis, whereby the communication channel is only open during flexion of the knee joint. This bursa is considered the main site of popliteal cysts(Baker’s cysts). This bursa is also regarded as the union of the bursa subtendinea gastrocnemii medialis and the bursa subtendinea semimembranosi in the case of the existence of a communication channel.
Bursa infrapatellaris profunda
usually non-communicating bursa between the patellar ligament and the outer layer of the joint capsule or Hoffa’s fat body. Both forms of infrapatellar bursitis (profunda and subcutanea) are often caused by prolonged kneeling in an otherwise upright position, which is why the bursitis is known as „clergyman’s knee“. Sporting activities can also trigger it.
Images:
Linkmap: Lateral view of the knee joint, bursa
Linkmap: Knee joint, 90° flexed
Linkmap: Patella
Linkmap: Knee joint, sagittal view
Bursa infrapatellaris subcutanea
Bursa between the patellar ligament and skin. Both forms of infrapatellar bursitis (profunda and subcutanea) are often caused by prolonged kneeling in an otherwise upright position, which is why the bursitis is called „priest’s knee“. Sporting activities can also be a trigger. The bursa can communicate with the bursa subcutanea praepatellaris and the bursa subcutanea tuberositas tibiae.
Images: (not yet available)
Bursa Lig. cruciatorum
Inconstant bursa in the fatty connective tissue that lies between the collagen fibers of the cruciate ligaments.
Medial patellar bursa
Inconstant bursa between patella and retinaculum patellae mediale.
Lateral patellar bursa
Inconstant bursa between the patella and the lateral patellarretinaculum.
Bursa poplitei
communicating bursa, also known as the subpopliteal recess or popliteal recess, which lies between the tibia, the outer meniscus and the tendon of origin of the popliteus. It is inconstantly connected to the tibiofibular joint and then connects both joint cavities.
Images:
Linkmap: Lateral view of the knee joint, bursa
Linkmap: Poplitea profund
Bursa sartorii proprii
Bursa located between the superficial and deep tendon layers before insertion of the Sartorius.
Bursa subaponeurotica praepatellaris
Inconstant (80%) bursa between the patella, quadriceps tendon and the superficial fascia. It can communicate with the bursa subcutanea praepatellaris and the bursa subfascialis praepatellaris.
Bursa subcutanea epicondyli tibialis
Inconstant subcutaneous bursa on the medial epicondyle of the tibia, occasionally triggered by mechanical stress(pressure), for example in riders.
Bursa subcutanea praepatellaris
Inconstant, often non-communicating bursa located under the skin in front of the kneecap. It is also known as the prepatellar recess. Frequent kneeling can lead to its inflammation(bursitis)(bursitis praepatellaris, Housemaids knee, common in roofers, tilers or carpet layers). Communication may take place with the bursa infrapatellaris subcutanea, bursa subfascialis praepatellaris, bursa subaponeurotica praepatellaris.
Linkmap: Patella
Linkmap: Knee joint, sagittal view
Bursa subcutanea tuberositatis tibiae
Inconstant subcutaneous bursa over the tibial tuberosity that develops as a reaction to repetitive kneeling activities. This bursa is at the top of the list of occupational bursitis of the knee.
Bursa subfascialis praepatellaris
Often non-communicating bursa between the patella and its ventral fascia (fascia superficialis). It may communicate with the subcutaneousbursa praepatellaris and the subaponeuroticbursa praepatellaris
Images: (not yet available)
Bursa subtendinea gastrocnemii medialis
communicating bursa between the medial condyle of the femur and the tendon of the medial origin of the gastrocnemius. In addition to communicating with the knee joint, both bursae of the gastrocnemius can also communicate with each other.
This bursa is also known as the bursa capitis tibialis m. gastrocnemii.
Images:
Linkmap: Poplitea profunda
Bursa subtendinea gastrocnemii lateralis
communicating bursa between the lateral condyle of the femur and the lateral tendon of origin of the gastrocnemius. In addition to communicating with the knee joint, both bursae of the gastrocnemius can also communicate with each other.
This bursa is also known as the bursa capitis fibularis m. gastrocnemii.
Images:
Linkmap: Poplitea profunda
Bursa subtendinea praepatellaris
Usually non-communicating bursa under the tendon fibers of the quadriceps or the patellar ligament directly on the patella
Images: (still without)
Bursa subtendinea semimembranosi (musculi semimembranosi, semimembranosa tibialis)
communicating bursa between the attachment tendon of the semimembranosus and the medial condyle of the tibia or the medial origin of the gracilis.
Images: (still without)
Suprapatellar bursa
Bursa located proximal to the patella between the distal femur and the attachment tendon of the vastus intermedius of the quadriceps. It allows the tendon to glide against the bone. The bursa communicates with the joint cavity from the 5th (fetal) month and is therefore also called the suprapatellar recess. It extends from the cranial patellar pole up to 8 cm cranially.
Images:
Linkmap: Lateral view of the knee joint, bursa
Linkmap: Patella
Linkmap: Knee joint, sagittal view
Bursa suprapatellaris intermuscularis accidentalis
Inconstant, rarely occurring bursa between the rectus femoris ventrally, the vastus intermedius dorsally and the vastus medialis or vastus lateralis medially or laterally. It is located more superficially than the anterior and superior recess of the joint capsule and the suprapatellarbursa.
Further structures
Menisci (inner meniscus, outer meniscus)
The menisci, which consist of fibrocartilage, are named after their curved shape. They are divided into cornu anterius, pars intermedia and cornu posterius. The menisci act as a buffer that absorbs pressure and impact from the bones and distributes it more evenly. They bear around 45% of the load. At the same time, their outwardly thickening shape contributes to the guidance of the joint partners. The functions of the menisci also include proprioception and reinforcement of the medial collateral ligament. During flexion of the knee joint, the menisci slide dorsally, during extension they slide ventrally, partially absorbing or slowing down rotational movements and load peaks.
The far outer zone („red zone„) of the menisci is still well vascularized, in a transition zone („white-red zone„) further inwards the vascularization is already clearly weakening and in the innermost area („white zone„) near the contact surface of the articular cartilage there is no longer any vascularization. The menisci are supplied by different arteries: inner meniscus: R. articularis of the A. genus descendens and A. genus superior medialis, outer meniscus: A. genus inferior lateralis.
Menisci also help to distribute the synovial fluid over a larger area than would be the case if only the cartilage of the femur and tibia were in contact. The menisci are particularly damaged when the lower leg is rotated in the knee joint under load and when the knee joint is rapidly extended or flexed under load. Steinmann1, Steinmann 2, Apley, Böhler, McMurray, Payr(medial meniscus) are common tests for meniscus lesions, but others are available in the tests section of the yoga book.
Meniscus lateralis (articulationis) genus / outer meniscus
The outer meniscus extends with its anterior cornu from the front of the eminentia intercondylaris of the tibia, near the insertion of the anterior cruciate ligament, to its posterior side (posterior horn). Shortly before its dorsal end, the posterior meniscofemoral ligament (Wrisberg ligament) often forms from a fiber bundle of the posterior horn. The outer meniscus is subjected to increased stress by endorotation in the knee joint and is relieved by exorotation.
Meniscus medialis (articulationis) genus / medial meniscus
In contrast to the barely connected outer meniscus, the middle part of the inner meniscus is firmly fused with the medial joint capsule, which is reinforced with fibers (buffered against the inner ligament by a bursa ), and the inner collateral ligament. It runs from the area intercondylaris anterior (anterior horn) to the area intercondylaris posterior (posterior horn). The anterior horn is attached to the anterior intercondylar fossa of the tibia by the anterior meniscofemoral ligament (Humphey ligament), while the posterior horn is attached to the posterior intercondylar fossa by the posterior meniscofemoral ligament (Wrisberg ligament). The posterior horn is connected to the bourgery ligament (posterior oblique ligament, POL) and also to the semimembranosus, which makes this part of the meniscus less mobile and therefore more susceptible to injury. .
Hoffa’s fat body / corpus adiposum infrapatellare
the fatty body located behind(dorsal) the patellar ligament, which prevents the patellar ligament from becoming trapped in the joint space when the knee joint is extended. An altered fat body can itself become trapped, causing impingement, which is known as Hoffa’s (Kastert’s) syndrome. The Hoffa’s fat body is partly responsible for the supply of the anterior cruciate ligament. The knee should be mobilized again as soon as possible after an anterior cruciate ligament plastic surgery to avoid adhesions of the Hoffa’s fat body to the cruciate ligament. Various interventions on the knee joint can damage Hoffa’s fat body and lead to pain phenomena, some of which are resistant to treatment, possibly with fibrosis, with the medial and lateral parts proving to be particularly sensitive.
Plicae
The plicae synoviales are folds of synovia that have not regressed after embryonic formation of the knee. The knee joint develops fetally from three compartments separated by synovial septa: one lateral, one medial and one patellar. In 25-30% of cases, these septa regress incompletely, leaving the synovial plicae:
Plica synovialis mediopatellaris
Plica synovialis infrapatellaris
Plica synovialis lateralis
Plica synovialis suprapatellaris
Due to their elastin and fatty tissue content, they do not normally pose a problem. They usually remain asymptomatic and are at most detected as an incidental finding. The plica synovialis mediopatellaris(medial shelf) is the one that most frequently leads to disorders because it is located in an easily irritated area. For more information on the disorders caused by plicae, see plica syndrome.
Movements
Extension (stretching) quadriceps femoris muscle (almost exclusively), rectus femoris muscle more powerful when the hip joint is extended, tensor fasciae latae muscle (insignificant)
Flexion (bending) M. semimembranosus, M. semitendinosus, M. biceps femoris, M. gracilis, M. sartorius, M. poplieteus, M. gastrocnemius, M. plantaris. The tensor fasciae latae also has a flexing effect via the iliotibial tract when the knee joint is flexed by at least 30°.
Internal rotation of the lower leg: M. semimembranosus, M. semitendinosus, M. gracilis, M. sartorius, M. poplieteus
External rotation of the lower leg: M. biceps femoris
Pathology
The knee is a region with a very high density of entities. Here are some diseases of the joint:
Important misalignments of the knee are
- genu vargum (bow leg), also unilateral
- genu valgum (X-leg), also unilateral
- genu flexum (non-extensible knee, also: genu procurvatum, extension deficit)
- genu recurvatum (knee hyperextended by more than 5°)
In the case of knee injuries, it is helpful to know the direction, duration and strength of the force applied as well as the position of the knee. In the case of diseases, a careful medical history and corresponding functional tests are important. The following are some of the more common entities or disorders of the knee joint:
- Osgood-Schlatter disease is a typical disease of the knee in adolescents with pain in the area of the tibial tuberosity, especially during jumping sports
- Patellar tendinitis (jumper’s knee) is a typical condition of older adolescents/young adults
- Degenerative meniscopathies/damage to the menisci occur from young adulthood onwards, possibly with incarcerations
- Gonarthrosis, i.e. osteoarthritis of the knee joint. See also the article on cartilage damage in the knee joint
- Chondropathia patellae
- Retropatellar arthrosis, possibly with a feeling of instability, is particularly painful when climbing stairs or walking downhill and is noticeable by rubbing; the knee may be swollen at the same time
- Diffuse knee pain without causative trauma is often the result of meniscus degeneration or osteoarthritis, often with signs of inflammation, swelling, overheating
- Baker’s cysts become noticeable through pain or a popliteal foreign body sensation, the neighboring joints hip joint, SI joint, ankle/foot can be involved or causative, anatomical and functional leg length discrepancies can be the cause
- Knee joint swelling can be synovial (more than the physiological 2 ml, usually after overloading, only slight overheating, self-resolving within days) or bloody (hemarthrosis, usually traumatic, bulging, painful swelling, overheating).
- Infections in the joint show marked overheating and redness, bulging, clearly painful effusion, painfully restricted movement.
- Tearing, tearing or overstretching of one or more ligaments: outer ligament, inner ligament, anterior or posterior cruciate ligament
- Psoriatic arthritis
- Perthes‘ disease and consequential damage to the knee
- Gout
- Baker’s cyst
- Rheumatoid arthritis (RA)/chronic polyarthritis (CP) (also: true „rheumatism“)
- more rarely: impingement
- Mobrus ankylosing spondylitis
- Secondary conditions in pathology of the foot
- Plica syndrome
- Runner’s knee/ITBS (Iliotibial Band Syndrome)
- Hoffa syndrome
Note the other health conditions with regard to secondary genupathies, such as those caused by Lyme disease
- Patellofemoral knee pain usually increases with strain, especially when descending stairs and sitting for long periods. If the pain continues to worsen under strain, this is indicative of cartilage damage; symptoms that first improve and then worsen later are more likely to indicate a muscle/tendon problem(quadriceps tendon, lig. patellae).
- Patellar luxation can show joint effusions, sometimes the medial retinaculum tears
- Patellar subluxation
- Patella baja (low position), possibly as a result of patella fractures or quadriceps tendon rupture
- Patella alta (high patella ), usually traumatic with rupture
- Patellar lateralization
- Excessive pronation rotates the tibia inwards and stresses the peripatellar soft tissue structures, causing ventral knee pain
When the quadriceps are not tensed, the patella is slightly lateralized. With tension and further flexion, it medializes and enters the trochlear gliding bearing. Unstable kneecaps and patellae altae only enter the gliding bearing with further flexion. All patellar malalignments lead to ventral peripatellar pain with tendinopathy and retropatellar cartilage changes, including an altered leg axis
Tests
Tests of the knee joint
Meniscus
- Joint Line Tenderness Palpation
- Thessaly test
- Apley grinding test
- Steinmann 1 sign
- Steinmann 2 sign
- Payr-sign (medial meniscus)
- McMurray test
- Childress test/Duck-walk test
- Merke sign
- Eges test
- Paessler-rotation-compression test
- Jump-Sign / Finochietto test
- Tschaklin sign
- Turner sign
- Chabot test
Medial collateral ligament
Lateral collateral ligament
Cruciate ligaments
- Lelli-Test (Ruptur des ACL)
- (Lateral) Pivot-Shift-Test (MacIntosh) (hyperextension or rupture of the ACL)
- Lachmann-(-Trillat / Ritchie-)Test (ACL)
- reversed Pivot-Shift-Test (PCL)
- Schubladen (drawer) Test (ACL and PCL)
- Gravity-Sign (posterior sag test, Godfrey-Test) (PCL)
- Marten-Test (Insufficiency of the ACL)
- Quadriceps Active Test / Active Drawer Test (PCL)
- Hyperextensions-Test (PCL)
ITBS (Runners knee)
IT-Band (Tractus iliotibialis) Verkürzung
Chondropathia patellae
Patella mixed
Hoffa-syndrome
Joint effusion
Q-angle
(Posterolateral Instability)
Patellaluxation/-subluxation
- Fairbank apprehension test (Smilie-Test)
- McConnell test
- Tilt test (tension of the lateral retinaculum)
- Subluxation suppression test
Plica-Syndrom
mixed
- Fründ sign (chondropathia patellae, retropatellar arthrosis, patella fracture)
- Böhler sign (menisci, collateral ligament damage)
- Dreyer test (patella fracture, Quadrizepssehnenriß)
Tests of the movement directions
Tests of the spanning muscles
Quadrizeps
Hamstrings
Images
Knee from dorsal, ligaments
Knee from dorsal
Knee from dorsal, capsule
Knee from ventral
Knee from ventrolateral
Knee from lateral
Knee transversal
Knee, saggital
ventral view in 90° flexion (image links to linkmap)

Lateral view in 45° flexion with expanded bursae (image links to linkmap)
Menisci on tibia from cranial (image links to linkmap)
Menisci with loaded rotation (image links to linkmap)