yogabook / joints / knee joint
Contents
- 1 Image: Knee from the side
- 2 Knee joint
- 3 Articulating bones
- 4 Partial joints
- 5 The movements and the muscles involved
- 6 Ligaments
- 6.1 Patellar ligament
- 6.2 Collateral ligaments Ligg. collateralia
- 6.3 Cruciate ligaments Ligg. cruciata
- 6.4 Meniscofemoral ligaments Ligg. meniscofemoralia
- 6.5 Lig. popliteofibulare (LPF)
- 6.6 Lig. popliteum arcuatum
- 6.7 Lig. popliteum obliquum (lig. bourgery)
- 6.8 Lig. collaterale mediale posterius (posterior oblique ligament, POL, posterior inner ligament, medial capsular ligament)
- 6.9 Lig. capitis fibulae anterius
- 6.10 Lig. capitis fibulae posterius
- 6.11 Lig. transversum genus
- 6.12 Retinaculum patellae
- 6.13 Medial capsular ligament
- 7 Bursa (bursae)
- 7.1 Bursa anserina
- 7.2 Bursa bicipitis femoris inferior
- 7.3 Bicipitogastrocnemial bursa
- 7.4 Bursa capitis tibialis gastrocnemii
- 7.5 Bursa gastrocnemiosemimembranosa
- 7.6 Bursa infrapatellaris profunda
- 7.7 Bursa infrapatellaris subcutanea
- 7.8 Bursa Lig. cruciatorum
- 7.9 Medial patellar bursa
- 7.10 Lateral patellar bursa
- 7.11 Bursa poplitei
- 7.12 Bursa sartorii proprii
- 7.13 Bursa subaponeurotica praepatellaris
- 7.14 Bursa subcutanea epicondyli tibialis
- 7.15 Bursa subcutanea praepatellaris
- 7.16 Bursa subcutanea tuberositatis tibiae
- 7.17 Bursa subfascialis praepatellaris
- 7.18 Bursa subtendinea gastrocnemii medialis
- 7.19 Bursa subtendinea gastrocnemii lateralis
- 7.20 Bursa subtendinea praepatellaris
- 7.21 Bursa subtendinea semimembranosi (musculi semimembranosi, semimembranosa tibialis)
- 7.22 Suprapatellar bursa
- 7.23 Bursa suprapatellaris intermuscularis accidentalis
- 8 Further structures
- 9 Pathology
- 10 Tests
- 10.1 Tests of the knee joint
- 10.1.1 Meniscus
- 10.1.2 Medial collateral ligament
- 10.1.3 Lateral collateral ligament
- 10.1.4 Cruciate ligaments
- 10.1.5 ITBS (Runners knee)
- 10.1.6 IT-Band (Tractus iliotibialis) Verkürzung
- 10.1.7 Chondropathia patellae
- 10.1.8 Patella mixed
- 10.1.9 Hoffa-syndrome
- 10.1.10 Joint effusion
- 10.1.11 Q-angle
- 10.1.12 (Posterolateral Instability)
- 10.1.13 Patellaluxation/-subluxation
- 10.1.14 Plica-Syndrom
- 10.1.15 mixed
- 10.2 Tests of the movement directions
- 10.3 Tests of the spanning muscles
- 10.1 Tests of the knee joint
- 11 Images
- 11.1 Knee from dorsal, ligaments
- 11.2 Knee from dorsal
- 11.3 Knee from dorsal, capsule
- 11.4 Knee from ventral
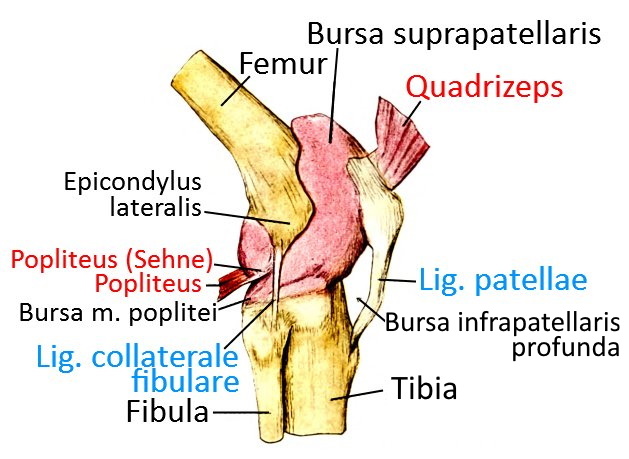
- 11.5 Knee from ventrolateral
- 11.6 Knee from lateral
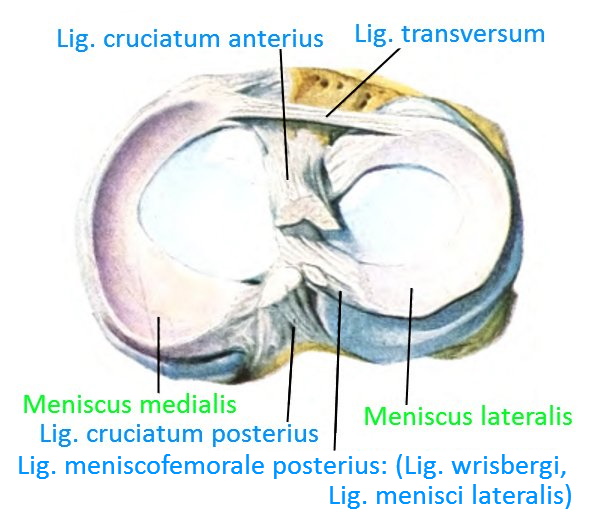
- 11.7 Knee transversal
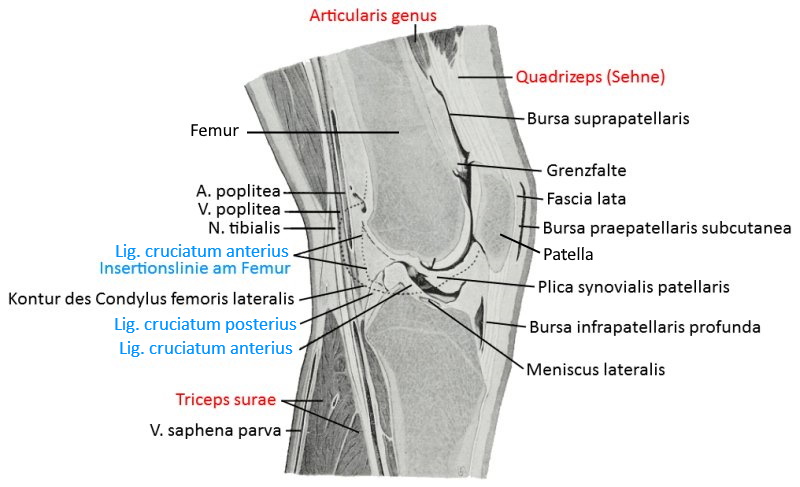
- 11.8 Knee, saggital
- 11.9 ventral view in 90° flexion (image links to linkmap)
- 11.10 Lateral view in 45° flexion with expanded bursae (image links to linkmap)
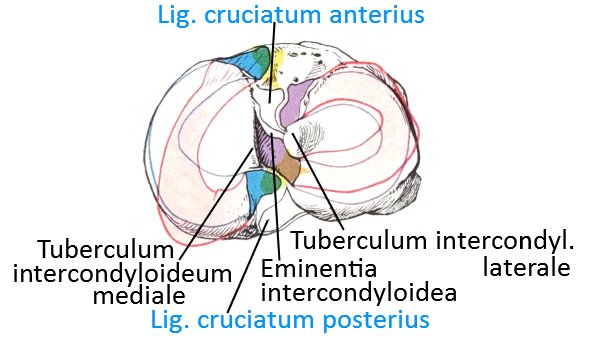
- 11.11 Menisci on tibia from cranial (image links to linkmap)
- 11.12 Menisci with loaded rotation (image links to linkmap)
Image: Knee from the side
Knee joint
The knee joint is usually understood to be the hinge joint in which the lower leg (more precisely the tibia) moves relative to the upper leg (more precisely the femur); this is the femorotibial articulation. As with the elbow joint, the main movement is flexion/extension. In addition, when the knee is flexed, the lower leg can rotate a little in relation to the thigh, but the movement is different from that of the forearm, as there is no overturning(pronation) of two bones and the range of movement is significantly smaller. The axis of rotation of the tibia runs through the medial meniscus, as this is fused with the medial ligament. In principle, translational movements in sagittal and transverse directions are also possible between the two bones, the tibia and femur, as well as compression/distraction movements, all of which are limited by the ligamentous structure of the knee joint. The physiological range of motion of the knee joint in the direction of flexion/extension is given as 5-0-150, whereby the 150° applies to active flexion due to passive insufficiency, while much more can be achieved passively. The degree of hyperextensibility of the knee joint varies from 0° to over 5°, whereby pain can occur from an individually different angle, but does not have to. The range of motion in the direction of rotation is specified as 10° internal rotation and 25° external rotation.
To stabilize the knee joint in movement and posture, the knee joint is well equipped proprioceptively with many sensors in the joint capsule-ligament apparatus. The information from the proprioceptors is processed in a neuronal network in the spinal cord and corresponding muscle actions are initiated. Therefore, the loss of a group of proprioceptors, such as the mechanoreceptors in the anterior cruciate ligament, does not directly result in a complete loss of the increased innervation of the hamstrings in the event of ventral translation of the tibia, but it does result in a reduced response and increased time lag – which causes increased wear and tear during intensive use of the knee joint.
The external angle of the two shafts of the femur and tibia in the frontal plane is physiologically 174° (and not 180°, due to the CCD angle in the femur) – if it falls below 171°, this is referred to as a knock-knee (genu valgum), if it exceeds 180° it is referred to as a bow-leg (genu varum), both of which are pathological and cause damage to the musculoskeletal system, especially the lower extremities. This is a problem that has so far been unsolvable for surgical plasty after tears, which is why postoperative physiotherapy training adapted to the new situation is of great importance.
Biomechanics of the knee joint
The menisci move about half as much as the femoral condyles. During this process, both the posterior and anterior parts of the meniscus absorb pressure, the femur is only in contact with the posterior meniscus when the knee joint is flexed, which is due to the smaller radius of the contact area. These factors mean that the posterior horn of the internal meniscus is the most vulnerable part of the meniscus and is particularly stressed when the knee is flexed further. This is why spontaneous tears of previously damaged menisci often occur in older people when they stand up from a squatting position. Pressure from the femur causes the menisci to be pushed towards the joint capsule, resulting in increased tension in the load-bearing fibre structures at the meniscus base (ring tension). These biomechanical properties favour the development of basket handle tears and explain why the function of the menisci is significantly less impaired in longitudinal tears than in radial tears. This also explains the importance of the meniscus roots and the danger that tearing off a meniscus root entails . In the playing leg phase of the gait cycle, the joint surfaces can be very well lubricated over a large area thanks to low-load contact between the two bones. When the heel touches down, a high contact pressure is quickly generated, but this does not tear the fluid film between the bones, as the ratio of the speed at which the femur moves towards the tibia and the viscosity of the synovia is not sufficient. The speed at flexion and extension is also too high to displace the liquid film in view of the given viscosity. The final critical phase for lubrication is the end of the leg phase with squeezing from the ankle, where a significant amount of fluid can indeed be squeezed out of the joint gap, but some large proteins remain as buffers. In connection with arthrosis, a reduced lubricity, i.e. lower viscosity of the synovia was observed, even more so in rheumatoid arthritis.The assertion that the essential pressures in the knee joint result from the musculature and not from the gravity of the partial body weight can be derived from two observations: when climbing up stairs, the force vector of the centre of gravity along the direction of gravity and the axis of rotation in the knee joint is 4.3 times the body weight due to the bent knee joints and the lever arm, 3 times the body weight, during normal walking about 3.4 times. On the other hand, to stand up from a chair, the pelvis must be shifted forwards with the upper body so that the gravity plumb line lies in the physical support base, resulting in a horizontal lever arm of about 20 cm from the gravity vector to the axis of rotation in the knee joint and a flexion of the knee joint of about 100°. With a lever arm of around 35 mm of the quadriceps in the knee joint, this results in around 2.9 times the body weight with which the quadriceps must contract. The weight force in the
tibiofemoral joint is approximately 3.4 times the body weight when standing up symmetrically on both legs.
The absolute forces and pressures in the tibiofemoral joint as well as in the quadriceps tendon and the contact force in the femoropatellar gliding bearing are linearly dependent on body weight in a static view, from which its significance for wear and tear follows. In the support leg phase of the gait cycle, the body’s centre of gravity is located approximately above the foot, which triggers a varus moment in the knee joint. This is presumably the reason why a valgus angle of 6 degrees has developed in humans, which largely compensates for this. In addition, the iliotibial tract generates a valgus moment not only in the CCD angle of the femur but also in the knee joint. However, these compensations do not prevent the gravity vector from passing the knee joint medially and at that time the medial aspect of the knee joint is loaded more than the lateral aspect. The forces in the knee joint resulting from the weight force are added to the symmetrical medial and lateral aspect of the knee joint, which acts on the quadriceps. Presumably because of this imbalance, the medial tibial condyle is slightly shorter than the lateral and in the medial aspect of the knee joint the congruence is slightly less pronounced. The variable loads on the bones of the tibia and femur are made up of compression forces and shear forces. The femur laterally displaces more than medially due to the greater length of its condyle, which also results in increased flexibility of the lateral meniscus, which is caused by the fact that the lateral meniscus is less firmly attached to the capsule and is not bound to the outer ligament. The much larger second
maximum of the flexion of the knee joint is located approximately in the centre of the gait cycle between the push-off with the toes and the reapplication of the heel. This width flexion of the knee joint of 67° on average serves to prevent the tips of the toes from striking the ground when the foot is pulled forwards. While the inertia of the leg pulls the hip ipsilaterally backwards at the end of the push-off phase due to the forward acceleration of the leg, the inertia inertia also causes the pelvis to move forwards towards the end of this swing phase when the heel touches down, which corresponds to an endorotation of the thigh in the hip joint. With the knee joint more or less extended, the higher tension of the medial gastrocnemius compared to the lateral a certain degree of inversion in the subtalar joint and upper ankle joint, in addition, the strongest foot lifters keep the medial tarsal lifted, as a result of which the longitudinal arch of the foot is lifted and the foot joints between them are fixed in final position. If the knee joint is flexed further in the stance phase, the gastrocnemius is less tensed and the powerful foot lifts acting on the medial tarsal are relieved. This cancels out the pronation in the subtalar joint and causes a certain degree of pronation tilt towards the middle of the stance phase due to the mass inertia, which cancels out the valgus position of the calcaneus. At the same time, the tarsus is loaded ventrally, which helps to reduce the longitudinal arch of the foot. The slight pronation is cancelled out by the supinatory triceps surae at the start of the push-off. This results in the typical rolling curve of the foot. With the extension of the knee joint at the end of the push-off phase and the reduced longitudinal arch of the foot, both the triceps surae in the ankle and the hip extensors in the hip joint provide a stable lever for the propulsion. The special shape of the condyles of the femur and tibia would cause the femur to slip dorsally over the tibia if the femoral condyles were only to roll on the tibial plateau. This is why the ligaments of the knee joint cause an increasing transition from the rolling movement to the sliding movement from an angle of 20 to 30 degrees. This mechanism is primarily caused by the anterior cruciate ligament. The opposite displacement of the femur towards the ventral during extension of the knee joint is limited by the rear cruciate ligament. In addition, the femur abuts the anterior meniscus, which also pushes the femur backwards and relieves the rear cruciate ligament. During flexion, in turn, the femur is limited in its movement not only by the anterior cruciate ligament but also by bumping against the posterior part of the menisci.
Instability or laxity or excess laxity
The laxity can be specified as translation or rotation for a given force or as the force required for a given translation or rotation. Passive stability is ensured by primary restraints with approximately the required direction of traction or rotation, which are supported by secondary restraints with a different direction. Therefore, in the case of partial or complete ligament tears, it cannot be concluded from the absence of instability symptoms that the primary stabilisers are intact. It is possible that the secondary stabilisers are taking over the work, but they are clearly at risk of being overloaded, meaning that the primary damage will result in secondary damage. For clinical testing, it is therefore essential that the tests used exclude coupled movements. The anterior drawer test may serve as an example, in which the anterior translation simultaneously generates an exorotatory moment in the knee joint. For precise clinical testing of the knee joint, all six degrees of freedom would have to be recorded. In connection with the knee joint, it must not be forgotten, that both the quadriceps and dorsally the gastrocnemius and the ischiocoral group generate translatory forces, which, however, are absorbed by healthy cruciate ligaments. This is the most important stabiliser against anterior rotation, which is most effective at around 30°. It is also important to avoid hyperextension. It acts as a secondary stabiliser with regard to end rotation of the lower leg and its valgus movement. It also causes the final rotation of the knee joint in the direction of its extension. The rear cruciate ligament primarily secures against translation in a dorsal direction and does so most intensively at flexion angles of 90°. Its anterior bundle becomes slack in the direction of extension of the knee joint, so that the posterolateral bundle primarily stabilises. The medial collateral ligament is the primary stabiliser against valgus movement and endorotation. As a secondary stabiliser, it supports the prevention of anterior drawer when the tibia is exorotated or in large anterior translation. It contributes significantly to limiting the exorotation of the lower leg. The posterolateral corner of the knee joint helps to prevent hyperextension and limits final rotation when the knee joint is approximately extended. The lateral collateral ligament is the most important stabiliser against variation of the lower leg. It becomes increasingly slack with increasing flexion of the knee joint, so that its stabilisation against dislocation also decreases. It stabilises against both drawers, but only for larger translations. Together with the posterolateral joint corner, it stabilises against wide exorotation.
Q-angle
The Q angle is the angle between the line connecting the SIAS to the patella centre and the line connecting the patella centre to the centre of the tibial tuberosity. Angles of 20° or more are considered abnormal and predispose to ventral knee pain. Similarly, a lateral offset of more than 10 degrees tibial tuberosity predisposes to ventral knee pain. A pathogenic influence of this deviation is primarily suspected in the case of a lack of congruence in the femoropatellar gliding bearing. An excessively tight lateral retinaculum is seen when the patella is pressed medially into the sliding bearing and the right patellar rim is not prominent ventrally. Instabilities of the knee joint are primarily caused by varus stress or valgus stress as well as impact trauma and hyperextension stress. They result intra-articularly from elongation of the cruciate ligaments or changes in the menisci as well as extra-articularly from changes in the collateral ligaments, the capsular ligaments or the muscle-tendon systems that cover the knee joint. Different changes occur depending on the type of trauma:
Damage mechanics to ligaments
Valgus–Exorotation–Flexion: Alteration of the medial collateral ligament, internal capsular ligament, lateral meniscus and anterior cruciate ligament. Hyperextension stress: anterior cruciate ligament, rear cruciate ligament, posterior capsule. Impact trauma: if the knee was sufficiently bent. Varus–Flexion trauma: posterolateral capsule and lateral collateral ligament. Capsule and ligament injuries are categorised into three degrees: first degree, displacement of 3 to 5 mm corresponds to a ligament overextension second degree change in length by 6 to 10 mm usually corresponds to a partial rupture, above 10 mm a rupture must be assumed. The type of impact also says something about the type of injury. In fresh traumatic knee injuries, the intensity of pain correlates negatively with the severity of the injury to the ligamentous apparatus. Varus stress tests and algus stress tests are performed at full knee extension and at 30° flexion. A medial gapping or lateral gapping indicates overstretching of one of the two collateral ligaments, possibly involving the posteromedial or posteolateral capsule and possibly the posterior cruciate ligament. At 30° flexion, the collateral ligaments can be tested in isolation. For a translation to ventral, the Lachman test, the no-touch Lachmann test, the anterior drawer in 90° flexion and the active anterior drawer sign (quadriceps active) can be used as the most important. The end stop is also informative here: if it is hard, there is probably an elongated ligament, if it is soft or missing, the ligament is ruptured and the capsule absorbs the movement. In addition to the pure translation to anterior, the anteromedial stability can also be tested with the rotation drawer. The anterior drawer test is performed with the knee joint flexed at 90° and the lower leg exorotated. If this test is positive, it is likely that not only the anterior cruciate ligament is damaged, but also the medial capsular ligament apparatus. An anterolateral instability is tested with endorotised lower leg accordingly .
Infantile knee
Babies have a varus position, which changes to a valgus position at preschool age, and later goes into a physiological position. Rare disorders of the infantile knee joint include tibia vara adolesentium, which resembles blunt’s disease, which does not develop before the age of five and in many cases is accompanied by obesity, so that a growth disorder in the medial epiphyseal fossa is assumed. Another rare disorder with a prevalence of 1 in 1000 is congenital knee luxation, which is associated with shortening of the quadriceps and sometimes missing cruciate ligaments. A clubfoot or hip dysplasia, possibly with hip dislocation, can accompany this disorder. Another rare condition that often occurs as part of other symptoms is patella aplasia or hypoplasia. Congenital patellar luxation, often with patellar hypoplasia, is also very rare. The displacement can go so far that the quadriceps itself functions as a flexor of the knee joint and the patella is barely palpable in the lateral soft tissues. If the patella forms not just from one bone nucleus but from two or three, this can lead to patella bipatita or tripartita, although this often remains clinically inconspicuous. Rotational deformities of the tibia also occur, particularly in the context of neuroorthopaedic disorders. It is extremely rare for the tibia to form a synostosis with the fibula proximally. In principle, all three bones, femur, tibia and fibula can be affected by malformations, as can their epiphyses, the metaphyses and the epimetaphyses.
The rheumatoid knee
Rheumatic diseases can act through synovitis, on the one hand via a detrimental change in the composition of the synovial fluid, and on the other hand as direct aggression against cartilage, bones and ligaments. In terms of aetiopathology, the knee joint does not differ fundamentally from other joints, but due to its high load, it is often one of the main causes. In addition to rheumatoid arthritis, other diseases also affect the knee joint, for example, ankylosing spondylitis with post-arthritic arthrosis, SLE with bone necrosis and psoriatic arthritis with mutations. In rheumatoid arthritis, a muscle-induced flexion contracture of the knee joint often occurs early on, which is based on atrophy of the quadriceps and shortening of the ischiocrural group. Synovialitis often leads to hypertrophic recesses. This can lead to restricted mobility. Rheumatoid gonitis tends to cause instability of the knee joint, on the one hand due to the resulting laxity of the capsular ligamentous apparatus, and on the other hand due to destruction of bone and bone. The cruciate ligaments can be synovially remodelled, which damages their function and substance and leads to anteroposterior instabilities. Pain avoidance-induced muscle atrophy further contributes to instability of the knee joint. In the frontal plane, there is usually a valgus deviation rather than a varus deviation, which would then usually be accompanied by an excessive endorotation tendency of the lower leg. Further axial deviations can result from loss of bone mass. The event must not be considered in isolation, but must include the joints of the lower extremity kinetic chain. Larsen et al have proposed a radiological classification into six stages. Miehle has classified the synovia according to the criteria of colour and opacity, viscosity, number of cells and other observations in RA and diseases of differential diagnostic importance indicated.
Capsule-tape apparatus
The extensive apparatus of ligaments and joint capsule lined with capsular ligaments, which in the case of the knee joint is extremely important for stability, can be divided into 4 fractions, which have an active and a passive aspect:
Media complex
passive:
- Medialretinaculum
- Lig. collaterale mediale
- Lig. popliteum obliquus (Lig. obliquus posterior, POL)
- Medial capsular ligament
- Medial half of the dorsal joint capsule
- Inner meniscus
- Anterior cru ciate ligament (ACL) and posterior cruciate ligament (PCL)
- Bony specifics of the tibial plateau and the medial femoral condyle
active:
- Vastus medialis
- Vastus medialis obliquus
- M. sartorius (Pes anserinus superficialis)
- M. gracilis (Pes anserinus superficialis)
- M. semitendinosus (Pes anserinus superficialis)
- M. semimembranosus (Pes anserinus profundus)
- M. gastrocnemius, Caput mediale
Lateral complex
passive:
- Joint capsule
- Lateral capsular ligament
- Lateral patellarretinaculum
- Lateral collateral ligament
- Tractus iliotibialis, also as part of the reserve extensor apparatus
- Tractotibial ligament
- Kaplan fibers
active:
Central complex
passive:
- posterior cruciate ligament
- anterior cruciate ligament
- Lig. meniscofemorale anterius
- Lig. meniscofemorale posterius
- Innenmeniskus
- Außenmeniskus
Ventral complex
passive:
- Lig. patellae
- Retinaculum patellae mediale
- Retinaculum patellae laterale
- Corpus adiposum infrapatellare (Hoffa’scher Fettkörper)
active:
Dorsal complex
passive:
- Dorsal capsule
- Lig. popliteum arcuatum
- Lig. popliteum obliquum
active:
Patella
The patella, which is flexibly supported by the femur (femoropatellar sliding bearing), is not directly associated with the knee joint as the femorotibial articulation, but is important for the transmission of force from the quadriceps. The patella and femur form a real joint here, the femoropatellar articulation. The transmission of force via the patella increases the lever arm and thus the possible torque in the knee joint for extension.
Around 50% of the distal tendon fibers of the quadriceps insert at the cranial patellar pole, the remaining fibers of the attachment tendon cover the patella in the direction of the tibial tuberosity or run medial or lateral to the patella as the medial patellarretinaculum or lateral patellarretinaculum.
Articulating bones
Partial joints
- Femorotibial joint Art. femorotibialis
- Femoropatellar joint (femoropatellar articulation, femoropatellar sliding bearing)
Femorotibial joint
The femorotibial joint is the joint that is usually meant when talking about the „knee joint“, i.e. the joint between the femur and tibia. It is a joint that combines the properties of a pivot joint (trochoidea) and a hinge joint (ginglymus), i.e. a combination of rolling and sliding movement of the two joint bodies. This connection is also known as a trochogingly joint or bicondylar joint. Adequate stability of the joint therefore requires good ligament guidance, which is provided here in the form of the cruciate and collateral ligaments.
Femoropatellar sliding bearing Art. femoropatellaris
The femoropatellar sliding bearing is the joint in which the patella rests flexibly on the femur, which transmits the contraction force of the quadriceps. During extension and flexion of the knee joint, the patella moves on the femur, as the patellar ligament is a non-elastic band that keeps the lower patellar pole at an approximately constant distance from the tibial tuberosity when tensed, whereas the quadriceps, as a contractile muscle, changes its length over a large range.
When the knee joint is flexed, this results in considerable contact pressure of the patella against the femur. The wear caused by overuse or uneven movement of the patella, for example when the lower leg rotates during extension or flexion, can lead to damage to the retropatellar cartilage(PFPS).
This joint is often affected by retropatellar cartilage disorders, for example in the form of chondropathia patellae (PFPS) or retropatellar arthrosis. Both phenomena are favored by:
- Incongruence of the joint surfaces
- Anomalies such as lack of height of the ridge (intercondylar sulcus) between the joint surfaces with the femoral condyles
- Relative hypertonus of the vastus lateralis or rectus femoris
- Overuse
A closer look reveals 3 rotational and 3 translational dimensions of movement in the femoropatellar sliding bearing:
- Translation superior-inferior, the most important physiological dimension of movement
- Rotation around the transverse medio-lateral axis of the patella due to the non-constant radii of the femoral condyles; this movement is referred to as flexion
- medio-lateral translation due to the variable, tolerance-dependent guidance of the fin of the patella in the trochlea (sulcus intercondylaris), „ML Shift“
- Rotation around the anterior-posterior transverse line perpendicular to the patella
- Rotation around the superior-inferior axis (tilt)
- anterior-posterior translation
Reserve extensor apparatus
The reserve extensor apparatus refers to the structures that remain after the patella, the lig. patellae or the insertion of the quadriceps at the patella nor force to the extension of the knee joint. The entities that cause this disorder are primarily patellar fracture, rupture of the quadriceps tendon or rupture of the patellar ligament from the tuberosity of the tibia. These include the vastus medialis tendon fibres of the retinaculum patellae (longitudinal) medial and the vastus lateralis and rectus femoris arising from fibres of the retinaculum longitudinale (medialis) laterale. Some authors also include the ilitibial tract, which at less than 30° flexion of the knee joint also supports its extension. Most sources state that the reserve extensor apparatus contains up to 50% of the fibres of the quadriceps tendon.
The movements and the muscles involved
Extension: M. quadriceps femoris (almost exclusively) thereby
M. rectus femoris with stretched hip joint more powerful,
M. tensor fasciae latae (only with less that 30° flexion of the knee)
Flexion: M. semimembranosus, M. semitendinosus, M. biceps femoris, M. gracilis, M. sartorius, M. poplieteus, M. gastrocnemius, M. plantaris. The tensor fasciae latae has a bending effect on the knee joint via the iliotibial band with the knee bend more than 30°.
Internal rotation of the lower leg: M. semimembranosus, M. semitendinosus, M. gracilis, M. sartorius, M. poplieteus
External rotation of the lower leg: M. biceps femoris
Ligaments
- Lig. collaterale mediale
- Lig. collaterale laterale
- Lig. cruciatum anterius
- Lig. cruciatum posterius
- Ligg. meniscofemoralia
- Lig. meniscofemorale anterius (Humphrey)
- Lig. meniscofemorale anterius (Wrisberg)
- Lig. patellae
- Lig. popliteum obliquum (posterior oblique ligament, POL, Bourgery)
- Lig. capitis fibulae anterius
- Lig. capitis fibulae posterius
- Lig. transversum genus
- Retinaculum patellae
- Retinaculum patellae laterale
- Retinaculum patellae mediale
- Retinaculum patellae transversale laterale
- Retinaculum patellae transversale mediale
Patellar ligament
The approx. 5-6 mm thick ligament is a capsular ligament that transmits the contraction force of the quadriceps from the lower edge of the patella(caudal patellar pole) to the tibia, where it inserts at the tibial tuberosity. If the quadriceps are not under tension, the patellar ligament is slack and could become trapped in the joint space when the knee joint is largely extended. This is why the Hoffa’s adipose body (corpus adiposum infrapatellare) lies behind(dorsally or profoundly) the patellar l igament, which prevents this due to its volume. A change in Hoffa’s fat body can lead to Hoffa’s syndrome, which usually only occurs secondarily.
Images:
Linkmap: Knee joint ventrolateral
Linkmap: Lateral knee joint
Linkmap: Knee joint, sagittal section
Linkmap: Tibia
Linkmap: Bones of the lower leg
Linkmap: Trunk ventral head to knee
Linkmap: Trunk lateral, superficial
Linkmap: Knee joint, 90° inflected
Linkmap: Lateral knee joint, bursa
Collateral ligaments Ligg. collateralia
the medial and lateral collateral ligaments that run longitudinally on the medial and lateral side of the knee joint, which tighten when the knee joint is extended due to the shape of the condyles and thus increasingly prevent the endo-and exorotation of the lower leg in the knee joint: the medial collateral ligament and the lateral collateral ligament (fibular). Another important task of the collateral ligaments is to absorb varusand valgus-likemovements and corresponding forces.
Lig. collaterale mediale (inner collateral ligament, lig. collaterale tibiale)
broad, flat ligament, approx. 9-11 cm long, which runs slightly offset dorsally on the medial side of the knee joint and stabilizes it against valgus movement. It runs from the epicondylus medialis femoris to the condylus medialis tibiae. It has an anterior and a posterior part, both of which diverge slightly distally. The more profound parts are fused with the medial meniscus. The proximal part is connected to the medial patellarretinaculum, the distal part merges into the popliteal oblique ligament and the dorsomedial capsule. The distal parts are partly overlaid by the pes anserinus and its attached muscles, which is why abursa (bursa anserina) buffers between them to reduce shear forces. A bursa separates the medial collateral ligament from the more profound structures, namely the joint capsule, which is reinforced with a capsular ligament, and the medial meniscus. The medial collateral ligament not only limits the valgus movement of the tibia and thus prevents medial gapping, but together with the fibular collateral ligament ( lateral collateral ligament) also limits the exorotation of the lower leg in the knee joint, which is why it is at risk in breaststroke athletes. The classic valgus stress test of the knee joint tests the sufficiency of the ligament. Due to the complex anatomy of the medial collateral ligament, the results of reconstructive surgery are often unsatisfactory. In particular, calcifications, which are more likely to occur the longer the knee joint is immobilized, often lead to functional deficits and restricted mobility.
Images:
Linkmap: Knee joint, dorsal, ligaments
Linkmap: Knee joint, dorsal
Linkmap: Knee joint, dorsal, capsule
Linkmap: Knee joint ventrolateral
Linkmap: Knee joint, 90° flexed
Lateral collateral ligament (outer collateral ligament, fibular collateral ligament)
The outer or fibular collateral ligament is a strong round ligament 5-7 cm long and, unlike the inner collateral ligament, has no connection to the meniscus. It is largely covered by the biceps femoris. It runs from the lateral femoral epicondyle, just below the sulcus of the popliteus tendon, to the head of the fibula. It splits the attachment tendon of the biceps femoris into an anterior and a posterior branch. The bursa subtendinea musculi bicipitis femoris inferior lies between the lateral collateral ligament and the biceps femoris. The popliteus tendon runs between the lateral collateral ligament and the lateral capsule. The ligament secures the knee joint against varus movement and limits exorotation.
Images:
Linkmap: Dorsal view of the knee joint, ligaments
Linkmap: Knee joint dorsal
Linkmap: Knee joint dorsal, capsule
Linkmap: Knee joint, 90° inflected
Linkmap: Lateral knee joint
Linkmap: Lateral knee joint, bursa
Cruciate ligaments Ligg. cruciata
The two ligaments that run intra-articularly but retrosynovially in the knee joint and prevent the tibia from shifting ventrally or dorsally in relation to the femur: the anterior cru ciate ligament and the even stronger posterior cruciate ligament. In terms of developmental history, they have migrated into the knee joint from the dorsal side. If they are damaged, unphysiological displacements occur, resulting in instability during movement and increased wear of the knee joint. Damage such as overstretching and tears can be recognized by the anterior or posterior drawer effect. In the English literature, theanterior cruciate ligament is referred to as the ACL(anterior cruciate ligament) and the posterior cruciate l igament as the PCL(posterior cruciate ligament). The name cruciate ligament comes from the fact that the two cruciate ligaments with their different directions of tension cross in the middle of the knee joint and develop complex biomechanics. To a limited extent, the cruciate ligaments also restrict the varus and valgus movements of the knee joint. As they wrap around each other during endorotation of the lower leg in the knee joint, they limit these movements. Tension and release as well as tightening and loosening of the cruciate ligaments are important for their metabolism.
Lig. cruciatum anterius (ACL, LCA, anterior cruciate ligament, anterior cruciate ligament)
The anterior cruciate ligament is probably the most important ligament for stabilizing the knee joint in the sagittal direction and, together with the posterior cruciate ligament, which runs in the opposite direction, secures it against translation of the tibia. Particularly in a slightly flexed position of the knee joint (approx. 20-30°), it strongly secures the tibia against forward displacement. Both cruciate ligaments together limit the final rotation of the lower leg in the knee joint. The anterior cruciate ligament also limits the extension of the knee joint. It runs from the lateral wall of the intercondylar fossa of the lateral femoral condyle to the proximal medial tibia at the anterior intercondylar area in front of the intercondylar eminence, just ventral to the medial intercondylar tubercle between the insertions of the anterior menisci. It therefore runs from posterior-superior-lateral to anterior-inferior-medial. Some fibers insert at the meniscal root of the medial meniscus. A distinction is made between two bundles according to origin and insertion: an anterior (anteromedial) bundle, which runs from the intercondylar line to the anterior tibial plateau, and a posterior (posterolateral) bundle, which runs from the border between the bone and cartilage of the femoral condyle to the posterior area of the tibia, close to the medial meniscus. An intermediate bundle can also be identified. The LCA is supplied with arterial blood from both sides, but the center and the insertion areas are usually not supplied with arterial blood. It has many mechanoreceptors (Golgi type III receptors, Ruffini corpuscles, Pacini type II corpuscles and free nerve endings), which serve the proprioception of the knee joint, but also the activation of knee joint stabilizing muscles, such as the hamstrings, which also pulls the tibia dorsally. In the event of ruptures of the LCA or replacement with a plastic, this function is no longer available, which puts more strain on the plastic than on the native cruciate ligament and leads to increased ventral translation and increased wear. If the ACL is damaged, the rolling-sliding mechanism of the knee joint is disrupted and damage occurs primarily to the posterior horns of the menisci, later also to cartilage damage to the tibia and femur, which can also be detected radiologically.
Images:
Linkmap: Knee joint from the dorsal side, ligaments
Linkmap: Dorsal knee joint, capsule
Linkmap: Knee joint ventral
Linkmap: Knee joint transversal
Linkmap: Knee joint, 90° inflected
Linkmap: Knee joint, menisci
Linkmap: Knee joint, distortion of the menisci during torsion
Posterior cruciate ligament (PCL, posterior cruciate ligament)
The posterior cruciate ligament runs from the inside of the medial femoral condyle diagonally to the lateral distal to the posterior intercondylar area, i.e. from ventral-cranial-medial to dorsal-caudal-lateral and thus runs transversely to the anterior cruciate ligament. A longer, stronger anterolateral and a shorter, less strong dorsomedial fiber bundle can be distinguished.
dorsomedial fiber bundle. The quadriceps, innervated by the proprioceptors of the longitudinal retinaculi of the patella, which radiate from its fibers, work to prevent excessive strain on the posterior cruciate ligament. Good development of the two important quadriceps parts, vastus medialis and vastus lateralis, from which these retinaculi radiate, is therefore important for an athlete.
Images:
Linkmap: Knee joint from dorsal, ligaments
Linkmap: Dorsal knee joint, capsule
Linkmap: Knee joint ventral
Linkmap: Knee joint transversal
Linkmap: Knee joint, 90° inflected
Linkmap: Knee joint, menisci
Linkmap: Knee joint, distortion of the menisci during torsion
Meniscofemoral ligaments Ligg. meniscofemoralia
The meniscofemoral ligaments support the posterior cruciate ligament and occur inconsistently. The Humphrey ligament stretches when the knee joint is flexed and the Wrisberg ligament stretches when the knee joint is extended. If the posterior cruciate ligament is damaged, they can partially take over its function. They stabilize the knee joint with regard to posterior translation of the tibia:
- the Wrisberg ligament (posterior meniscofemoral ligament), which can be differentiated into three types and lies dorsal to the posterior cruciate ligament, accounting for approx. 70%.
- the Humphrey ligament (anterior meniscofemoral ligament) lying ventral to the posterior cruciate ligament in about 50% of cases
Information on the presence of the ligaments varies in the literature. The Wrisberg ligament can be quite pronounced. In 61% of cases, both meniscofemoral ligaments are present. They then wrap around the posterior cruciate ligament. The Humphrey ligament stretches in flexion, the Wrisberg ligament in extension of the knee joint. Both tighten when the lower leg is in endorotation. Their most important task is to prevent the posterior horn of the lateral meniscus from becoming trapped.
Images:
Linkmap: Knee joint from dorsal, ligaments
Linkmap: Knee joint transversal
Linkmap: Knee joint, menisci
Anterior meniscofemoral ligament: „Humphrey ligament„
The anterior meniscofemoral ligament runs from the posterior meniscal root of the lateral meniscus in front of the posterior cruciate ligament to the inner surface of the medial femoral condyle.
Posterior meniscofemoral ligament: „Wrisbergligament„
Like the anterior meniscofemoral ligament, the posterior meniscofemoral ligament runs from the posterior meniscal root of the lateral outer meniscus to the medial femoral condyle, but runs behind the posterior cruciate ligament. An existing Wrisberg ligament must not be misinterpreted radiologically as a tear of the meniscus. The origin of the three types of Wrisberg ligament is identical, but they differ in their attachment:
- Posterior horn of the medial meniscus (most common form)
- fan-shaped from the meniscus to further medial to the tibia
- without attachment to the meniscus, only to the tibia, sometimes considered part of the posterior cruciate ligament as it is not connected to the meniscus
Images:
Linkmap: Knee joint, meniscus
Lig. popliteofibulare (LPF)
The popliteofibular ligament (LPF) radiates from the head of the fibula into the tendon of the popliteus.
Lig. popliteum arcuatum
The popliteus arcuate ligament is an extracapsular dorsal ligament of the knee joint that runs from the posterior edge of the head of the fibula obliquely in a craniomedial direction and crosses the popliteus insertion, which it attaches to the joint capsule. It covers the dorsolateral joint area in a fan shape and runs partly parallel to the lateral collateral ligament.
Images: (still without)
Lig. popliteum obliquum (lig. bourgery)
The oblique popliteofibular ligament, which runs from the posterior edge of the head of the tibia obliquely craniolaterally to the upper edge of the intercondylar fossa and to the posterior surface of the femur, taking up the tendon of the semimembranosus in a lateral split. It reinforces the dorsal capsule of the knee joint. In extension of the knee joint it is taut and prevents medial and lateral gapping, in flexion it is relaxed. Because of its connection to the semimembranosus, it still contributes to the stability of the joint even when relaxed in flexion. This ligament can have connections to the medial collateral ligament, the popliteus tendon and the dorsal capsule.
Images:
Linkmap: Knee joint dorsal
Linkmap: Knee joint, sagittal section
Lig. collaterale mediale posterius (posterior oblique ligament, POL, posterior inner ligament, medial capsular ligament)
The POL moves from the adductor tuberosity in three different lines:
- to the posterior edge of the tibia and medial meniscus (this is the main traction)
- to the tendon of the semimembranosus (medial fiber tract)
- merges with the tendon of the semimembranosus in the lig. popliteum obliquum
It stabilizes against valgus stress and exorotation, both in extension (together with the medial collateral ligament) and in flexion (in conjunction with the tensed semimembranosus). Together with the posterior horn of the medial meniscus, the ACL and the medial collateral l igament, it protects against excessive translation of the tibia in the sagittal direction.
Lig. capitis fibulae anterius
Ventral ligament of the proximal tibiofibular joint that reinforces the capsule. It runs from the ventral caput fibulae and facies articularis fibularis of the lateral tibial condyle. The anterior capitis fibulae ligament is stronger than its posterior equivalent, the posterior capitis fibulae ligament.
Images:
Linkmap: Knee joint from dorsal, ligaments
Linkmap: Knee joint, 90° flexed
Lig. capitis fibulae posterius
Dorsal ligament of the proximal tibiofibular joint that reinforces the capsule dorsally. It is less pronounced than its ventral counterpart, the anterior capitis fibulae ligament.
Images: (still without)
Lig. transversum genus
The variably pronounced transverse genus ligament is an intra-articular ligament that connects the two anterior horns of the menisci(inner meniscus and outer meniscus). No significant function has yet been demonstrated.
Linkmap: Knee joint, 90° flexed
Linkmap: Knee joint, menisci
Linkmap: Knee joint, transverse
Retinaculum patellae
The retinaculum patellae consists of two individual longitudinal ligaments, a lateral retinaculum patellae laterale and a medial retinaculum patellae mediale, which surround the patella from the outside and hold it in position.
lateral trans verse and in 30% also a medial transverse retinaculum. The transverse retinaculi lie deeper than the longitudinal retinaculi. Patelladislocations are therefore generally prevented if the ligamentous apparatus is undamaged. The longitudinal fibers of the patellar retinaculum can transfer a residual contraction force of the quadriceps to the tibia in the event of a tear in the patellar ligament and thus maintain a small residual extensor function, which is why they are referred to as the reserve extensor apparatus.
Medial patellar retinaculum (MPFL)
The medial patellar retinaculum originates from the tendon fibers of the medial vastus, which do not attach to the cranial patellar pole and do not cover the patella. They extend to the medial edge of the patella and the tibial collateral ligament as well as to the medial condyle of the tibia medial to the tibial tuberosity and the patellar ligament.
In addition to the fibres of the vastus medialis, which form the superficial part of this retinaculum, fibres also carry lig. collaterale mediale (intermediate part) and the patellofemoral ligament (deep part) also contribute to the patellar retinaculum mediale.
Images: (still without)
Lateral patellar retinaculum
The lateral patellar retinaculum arises from the tendons of the lateral vastus and the rectus femoris and extends to the lateral edge of the patella and the collateral fibular ligament as well as to the lateral condyle of the tibia lateral to the tibial tuberosity and the patellar ligament.
In addition to tendon fibres from the two muscles mentioned above, fibres from the patellofemoral ligament lateral and the iliotibial tract as well as the biceps femoris also contribute to this retinaculum.
Images:
Linkmap: Knee joint ventrolateral
Retinaculum patellae, transverse parts
In addition to the retinaculum patellae laterale and retinaculum patellae mediale, there is often a lateral transverse part(retinaculum patellae transversale laterale) and in 30% a medial transverse part(retinaculum patellae transversale mediale).
Images: (still without)
Lateral transverse patellar retinaculum (LPTL)
The transverse lateral part originates from tissue of the iliotibial tract and runs on the one hand without connection to the lateral epicondyle as the lateral patellofemoral ligament to the mid-superior lateral edge of the patella and on the other hand runs further caudally (lower lateral edge of the patella) as the lateral patellofemoral ligament. Further cranially there is a connection between the patella and the lateral condyle of the femur via the Kaplan fibers.
Images: (still without)
Lateral patellofemoral ligament
The fiber tract of the transverse lateral patellarretinaculum described above from the mid-superior lateral edge of the patella to the iliotibial tract.
Lateral patellotibial ligament
The fiber tract of the transverse lateralretinaculum patellae from the lower lateral edge of the patella to the iliotibial tract described above.
Kaplan fibers
the cranial connection of the lateral patellarretinaculum to the lateral condyle of the femur.
Retinaculum patellae transversale mediale (patellotibial ligament)
The transverse medial part consisting of fibers of the tendon of the vastus medialis, which extend to the medial edge of the patella and to the femur lateral to the medial collateral ligament.
Images: (still without)
Medial patellofemoral ligament
the cranial (femoral) part of the retinaculum patellae transversale mediale
Medial patellotibial ligament
the caudal (tibial) part of the transverse medial patellarretinaculum
Medial capsular ligament
The medial capsular ligament, which runs from cranial to caudal, represents the fiber-reinforced middle third of the medial capsule. It is firmly fused to the base of the meniscus. The cranial part is referred to as meniscofemoral, the caudal part as meniscotibial. During
extension of the knee joint it is taut and becomes slack even with slight flexion, only to tighten again with further flexion, so that it protects against valgus stress and excessive exorotation during extension and further flexion.
Bursa (bursae)
There are many bursae in the knee area, which is often subject to high mechanical stress. Some of these are constant, others are caused by corresponding stimuli/stress, such as frequent, prolonged kneeling or activities on the knees or in a squatting position. Bursitis can also develop here if overloaded, especially in the:
- Bursa subcutanea praepatellaris „Housemaid’s Knee“
- Bursa subcutanea infrapatellaris due to frequent or prolonged kneeling „clergyman’s knee“, „priest’s knee“
- Bursa subcutanea tuberositatis tibiae
These bursitis often occur in craftsmen, roofers, tilers, carpet layers, fitters and cleaners with kneeling activities as well as clerics whose religion requires kneeling prayers.
Bursa anserina
in the area below the knee joint between the inner collateral ligament and the common insertion tendon of the semitendinosus, sartorius and gracilis on the pes anserinus superficialis. The bursa ensures that the structures can move relative to each other.
(Breast) swimmers and runners are particularly affected by bursitis.
Pictures: (still without)
Bursa bicipitis femoris inferior
Constant, non-communicating bursa between the lateral collateral ligament and the insertion tendon of the biceps femoris.
Images:
Linkmap: Poplitea profunda
Bicipitogastrocnemial bursa
Inconstant bursa located between the insertion of the biceps femoris and the lateral caput of the gastrocnemius.
Images:
Linkmap: Poplitea profunda
Bursa capitis tibialis gastrocnemii
Other name for the bursa subtendinea gastrocnemii medialis
Bursa gastrocnemiosemimembranosa
Bursa between the medial head of the gastrocnemius and the insertion tendon of the biceps femoris, which in 1/3 of cases communicates with the inconstant bursa subtendinea gastrocnemii medialis, whereby the communication channel is only open during flexion of the knee joint. This bursa is considered the main site of popliteal cysts(Baker’s cysts). This bursa is also regarded as the union of the bursa subtendinea gastrocnemii medialis and the bursa subtendinea semimembranosi in the case of the existence of a communication channel.
Bursa infrapatellaris profunda
usually non-communicating bursa between the patellar ligament and the outer layer of the joint capsule or Hoffa’s fat body. Both forms of infrapatellar bursitis (profunda and subcutanea) are often caused by prolonged kneeling in an otherwise upright position, which is why the bursitis is known as „clergyman’s knee“. Sporting activities can also trigger it.
Images:
Linkmap: Lateral view of the knee joint, bursa
Linkmap: Knee joint, 90° flexed
Linkmap: Patella
Linkmap: Knee joint, sagittal view
Bursa infrapatellaris subcutanea
Bursa between the patellar ligament and skin. Both forms of infrapatellar bursitis (profunda and subcutanea) are often caused by prolonged kneeling in an otherwise upright position, which is why the bursitis is called „priest’s knee“. Sporting activities can also be a trigger. The bursa can communicate with the bursa subcutanea praepatellaris and the bursa subcutanea tuberositas tibiae.
Images: (not yet available)
Bursa Lig. cruciatorum
Inconstant bursa in the fatty connective tissue that lies between the collagen fibers of the cruciate ligaments.
Medial patellar bursa
Inconstant bursa between patella and retinaculum patellae mediale.
Lateral patellar bursa
Inconstant bursa between the patella and the lateral patellarretinaculum.
Bursa poplitei
communicating bursa, also known as the subpopliteal recess or popliteal recess, which lies between the tibia, the outer meniscus and the tendon of origin of the popliteus. It is inconstantly connected to the tibiofibular joint and then connects both joint cavities.
Images:
Linkmap: Lateral view of the knee joint, bursa
Linkmap: Poplitea profund
Bursa sartorii proprii
Bursa located between the superficial and deep tendon layers before insertion of the Sartorius.
Bursa subaponeurotica praepatellaris
Inconstant (80%) bursa between the patella, quadriceps tendon and the superficial fascia. It can communicate with the bursa subcutanea praepatellaris and the bursa subfascialis praepatellaris.
Bursa subcutanea epicondyli tibialis
Inconstant subcutaneous bursa on the medial epicondyle of the tibia, occasionally triggered by mechanical stress(pressure), for example in riders.
Bursa subcutanea praepatellaris
Inconstant, often non-communicating bursa located under the skin in front of the kneecap. It is also known as the prepatellar recess. Frequent kneeling can lead to its inflammation(bursitis)(bursitis praepatellaris, Housemaids knee, common in roofers, tilers or carpet layers). Communication may take place with the bursa infrapatellaris subcutanea, bursa subfascialis praepatellaris, bursa subaponeurotica praepatellaris.
Linkmap: Patella
Linkmap: Knee joint, sagittal view
Bursa subcutanea tuberositatis tibiae
Inconstant subcutaneous bursa over the tibial tuberosity that develops as a reaction to repetitive kneeling activities. This bursa is at the top of the list of occupational bursitis of the knee.
Bursa subfascialis praepatellaris
Often non-communicating bursa between the patella and its ventral fascia (fascia superficialis). It may communicate with the subcutaneousbursa praepatellaris and the subaponeuroticbursa praepatellaris
Images: (not yet available)
Bursa subtendinea gastrocnemii medialis
communicating bursa between the medial condyle of the femur and the tendon of the medial origin of the gastrocnemius. In addition to communicating with the knee joint, both bursae of the gastrocnemius can also communicate with each other.
This bursa is also known as the bursa capitis tibialis m. gastrocnemii.
Images:
Linkmap: Poplitea profunda
Bursa subtendinea gastrocnemii lateralis
communicating bursa between the lateral condyle of the femur and the lateral tendon of origin of the gastrocnemius. In addition to communicating with the knee joint, both bursae of the gastrocnemius can also communicate with each other.
This bursa is also known as the bursa capitis fibularis m. gastrocnemii.
Images:
Linkmap: Poplitea profunda
Bursa subtendinea praepatellaris
Usually non-communicating bursa under the tendon fibers of the quadriceps or the patellar ligament directly on the patella
Images: (still without)
Bursa subtendinea semimembranosi (musculi semimembranosi, semimembranosa tibialis)
communicating bursa between the attachment tendon of the semimembranosus and the medial condyle of the tibia or the medial origin of the gracilis.
Images: (still without)
Suprapatellar bursa
Bursa located proximal to the patella between the distal femur and the attachment tendon of the vastus intermedius of the quadriceps. It allows the tendon to glide against the bone. The bursa communicates with the joint cavity from the 5th (fetal) month and is therefore also called the suprapatellar recess. It extends from the cranial patellar pole up to 8 cm cranially.
Images:
Linkmap: Lateral view of the knee joint, bursa
Linkmap: Patella
Linkmap: Knee joint, sagittal view
Bursa suprapatellaris intermuscularis accidentalis
Inconstant, rarely occurring bursa between the rectus femoris ventrally, the vastus intermedius dorsally and the vastus medialis or vastus lateralis medially or laterally. It is located more superficially than the anterior and superior recess of the joint capsule and the suprapatellarbursa.
Further structures
Menisci (inner meniscus, outer meniscus)
The menisci, which consist of fibrocartilage, are named after their curved shape. They are divided into cornu anterius, pars intermedia and cornu posterius. The menisci act as a buffer that absorbs pressure and impact from the bones and distributes it more evenly. They bear around 45% of the load. At the same time, their outwardly thickening shape contributes to the guidance of the joint partners. The functions of the menisci also include proprioception and reinforcement of the medial collateral ligament. During flexion of the knee joint, the menisci slide dorsally, during extension they slide ventrally, partially absorbing or slowing down rotational movements and load peaks.
The far outer zone („red zone„) of the menisci is still well vascularized, in a transition zone („white-red zone„) further inwards the vascularization is already clearly weakening and in the innermost area („white zone„) near the contact surface of the articular cartilage there is no longer any vascularization. The menisci are supplied by different arteries: inner meniscus: R. articularis of the A. genus descendens and A. genus superior medialis, outer meniscus: A. genus inferior lateralis.
Menisci also help to distribute the synovial fluid over a larger area than would be the case if only the cartilage of the femur and tibia were in contact. The menisci are particularly damaged when the lower leg is rotated in the knee joint under load and when the knee joint is rapidly extended or flexed under load. Steinmann1, Steinmann 2, Apley, Böhler, McMurray, Payr(medial meniscus) are common tests for meniscus lesions, but others are available in the tests section of the yoga book.
The meniscus also consists of living tissue, with fibroblasts being present in the outer red zone and cartilage-like cells in the inner white zone. Both produce their typical matrix components, which tend to be ground substance molecules and collagen fibres type 2 on the inside and type 1 fibres and fibrous ground substance on the outside. Anabolic stimuli for matrix production are growth factors such as IGF, PDGF, SGS and above all TGF. Cytokines such as TNF-alpha tend to induce a catabolic process. The cells of the meniscus are embedded in a specially constructed three-dimensional matrix so that compression forces can be converted into shear forces and stretching forces and channelled into the cell via transmembrane proteins (integrins). The meniscotibial ligaments are of particular importance in this process. There are two types of stimuli that inhibit the biological activity of the meniscus tissue: static compression and high impact shocks. On the other hand, cyclical stretching or dynamic compressions stimulate anabolism. The chemical environment is also important for metabolic processes. If it is inflammatory, this weakens the positive effect of the actual anabolic stimuli, even turning them into catabolic stimuli. As the chemical environment and the sensitivity to stimuli can be quite variable, it is difficult to formulate and parameterise a general meniscus anabolic training programme. However, due to the similarity of the inner zone in particular to the hyaline articular cartilage, a first approximation can be made. The absence of sufficient maintenance stimuli, particularly during immobilisation, leads to reduced production of the basic substance and reduced inhibition of catabolism. If the tissue is then overloaded, degenerative processes occur, which in turn lower the threshold for traumatisation, so that a circulus vitiosus can also arise here. Processes such as neovascularisation and sprouting of nerve endings are also found in the meniscus tissue, which are naturally most pronounced in the red zone. Tears occur primarily in the white zone with its weak metabolism. Occasionally, calcification of the meniscus is also seen. To date, there is no evidence that meniscoanabolic training can improve the condition of the menisci. However, the state of degeneration, as assessed by radiology, correlates little with the clinic. Even a clearly degenerated meniscus does not necessarily cause symptoms.
Although the menisci are not ligaments, they are also secondary stabilisers of the knee joint. They are connected to the tibia via their meniscus roots and peripheral ligaments and to the femur via the meniscofemoral ligaments and the profound portion of the deep medial collateral ligament. With increasing flexion of the knee joint, the patella moves further and further inferiorly under the femur. As a result, the tensile forces of the quadriceps tendon and the patellar ligament, which are still equal when the knee joint is extended, increasingly diverge such that the force in the quadriceps tendon becomes greater than that in the patellar ligament. For a 90 degree angle, the forces are in the following ratio patellar ligament to quadriceps tendon to retropatellar contact force: 1 to 1.6 to 1.9. With further flexion, these forces diverge even further. When standing up from a chair with the knee joint flexed at 90°, the patellar ligament is subjected to 2.9 times the body weight in tension, and the retropatellar contact force is 5.5 times and significantly exceeds the load in the tibiofemoral joint of 3.3 times. This deviation means that retropatellar discomfort without active quadriceps contraction is perceived much more intensely when sitting than when standing or in a flat position, which is referred to as a movie sign. Due to the physiological 174 degree angle between the femur and tibia, the knee joint experiences a lateralising effect of the patella and the directions of pull of the quadriceps tendon and the patellar ligament diverge. If the traction of the patella to the lateral is too great, this is referred to as lateral maltracking. In practice, the deviation is measured to be significantly greater than 6 degrees, namely 12 to 15 degrees (male) and 15 to 18 degrees (female). As a result, patellar dislocations are more strongly predisposed in females. The vastus medialis obliquus and, if present, the medial transverse retinaculum must absorb this force. The vastus lateralis consists of a long and an oblique part that lateralise the patella.
The loss of a meniscus does not necessarily lead to an increased possibility of translating the tibia, but the cruciate ligaments are put under more strain as a result. In particular, the loss of the anterior cruciate ligament conversely leads to increased strain on the internal meniscus in particular. If the function of the anterior cruciate ligament and the internal meniscus is lost, this results in even greater translation. The effect of the external meniscus on the translation is subordinate. During flexion of the knee joint, the menisci slide following the femur in a dorsal direction. The displacement of the external meniscus is about 10 mm, that of the internal meniscus about 5 mm. Rotational movements of the tibia lead to a non-uniform movement of the menisci, one towards the ventral, the other towards the dorsal. The inconsistent displacement of the two menisci is mainly due to the fact that the internal meniscus is fused with the internal ligament. In terms of pathology, this results in increased stress on the internal meniscus, particularly due to wide flexion of its posterior horn. Meniscus lesions follow different aetiologies, mainly divided into traumatic and degenerative. Between 10 and 25% of all injuries in sports such as football or handball affect the knee joint, in 25 to 40% of these cases a meniscus injury is included. The most difficult situation for the menisci are rotational movements in inflected, loaded knee joints. Traumatic lesions usually occur at the periphery, i.e. in the base of the meniscus near the meniscosynovial junction as a longitudinal tear or are radial tears. Traumatic meniscus damage usually affects people between the ages of 10 and 30, although dierect trauamta are very rare due to the location of the menisci between the femur and tibia, except for tibial head-fractures. With injuries to the anterior cruciate ligament, the meniscus is sometimes also affected, although in this case the lateral is more common than the medial. The combination of injury to the anterior cruciate ligament, the internal meniscus and the medial collateral ligament is known as the unhappy triad. Weight-bearing knee sports and repetitive squatting activities tend to cause degenerative damage, particularly to the posterior horn of the medial meniscus, through repeated microtrauma. This may be recognised as an occupational disease; originally only miners were recognised here, but today the group also includes tilers, parquet layers, stove masons, shunters, artists, professional football players and a few others. Degenerative damage predisposes to increased body weight. Damage to the anterior cruciate ligament with increased translational capacity also damages the meniscus, particularly the posterior horn of the medial meniscus. Irrespective of trauma and iterated microtrauma, the meniscus can also be damaged purely degeneratively, which is correlated with ageing. The damage is then mainly horizontal tears, flap tears and complex tears, peaking in the 4th and 5th decade of life.
A number of meniscus tests are available for diagnostics and clinical testing. During inspection and palpation, attention must be paid to the presence of a popliteal cyst and swelling in the joint space that causes a meniscus ganglion. Knee joint blockages and extension inhibitions and effusions must also be recorded. The differential diagnosis should include arthrosis, Ahlbäck’s disease, osteochondrosis dissecans, plica syndrome, rheumatic diseases, patellar dislocations and patellar subluxations, femoropatellar pain syndrome (Runners knee), chnodromatosis synovialis, gout and pseudogout, ganglion cysts of the cruciate ligaments, Morbus Sudeck and tumours. Degenerative meniscus lesions generally show no tendency to heal spontaneously but to progress. Stable ruptures close to the base can heal spontaneously. Conservative therapy consists primarily of managing the symptoms and the requirements for healthy functioning of the knee joint as well as moderating the strain. If necessary, a meniscus reduction can be performed in the event of an impingement. Chronic instabilities of the knee joint, particularly due to insufficient anterior cruciate ligaments, significantly worsen the prognosis. At the same time, it can be said that the larger the mass removed, the greater the tendency to osteoarthritis, especially if the meniscal rim has been removed. Pre-existing cartilage damage found during arthroscopic meniscectomy also worsens the prognosis. As a general rule, corpuscle tears, flap tears and longitudinal tears have a better prognosis than degenerative horizontal tears and complex tears, which are often accompanied by cartilage damage. A varus deformity of the lower leg particularly impairs the prognosis for the internal meniscus. The same applies to an valgus lower leg in the case of the external meniscus.
Meniscus lateralis (articulationis) genus / outer meniscus
The outer meniscus extends with its anterior cornu from the front of the eminentia intercondylaris of the tibia, near the insertion of the anterior cruciate ligament, to its posterior side (posterior horn). Shortly before its dorsal end, the posterior meniscofemoral ligament (Wrisberg ligament) often forms from a fiber bundle of the posterior horn. The outer meniscus is subjected to increased stress by endorotation in the knee joint and is relieved by exorotation.
Meniscus medialis (articulationis) genus / medial meniscus
In contrast to the barely connected outer meniscus, the middle part of the inner meniscus is firmly fused with the medial joint capsule, which is reinforced with fibers (buffered against the inner ligament by a bursa ), and the inner collateral ligament. It runs from the area intercondylaris anterior (anterior horn) to the area intercondylaris posterior (posterior horn). The anterior horn is attached to the anterior intercondylar fossa of the tibia by the anterior meniscofemoral ligament (Humphey ligament), while the posterior horn is attached to the posterior intercondylar fossa by the posterior meniscofemoral ligament (Wrisberg ligament). The posterior horn is connected to the bourgery ligament (posterior oblique ligament, POL) and also to the semimembranosus, which makes this part of the meniscus less mobile and therefore more susceptible to injury. .
Hoffa’s fat body / corpus adiposum infrapatellare
the fatty body located behind(dorsal) the patellar ligament, which prevents the patellar ligament from becoming trapped in the joint space when the knee joint is extended. An altered fat body can itself become trapped, causing impingement, which is known as Hoffa’s (Kastert’s) syndrome. The Hoffa’s fat body is partly responsible for the supply of the anterior cruciate ligament. The knee should be mobilized again as soon as possible after an anterior cruciate ligament plastic surgery to avoid adhesions of the Hoffa’s fat body to the cruciate ligament. Various interventions on the knee joint can damage Hoffa’s fat body and lead to pain phenomena, some of which are resistant to treatment, possibly with fibrosis, with the medial and lateral parts proving to be particularly sensitive.
Plicae
The plicae synoviales are folds of synovia that have not regressed after embryonic formation of the knee. The knee joint develops fetally from three compartments separated by synovial septa: one lateral, one medial and one patellar. In 25-30% of cases, these septa regress incompletely, leaving the synovial plicae:
Plica synovialis mediopatellaris
Plica synovialis infrapatellaris
Plica synovialis lateralis
Plica synovialis suprapatellaris
Due to their elastin and fatty tissue content, they do not normally pose a problem. They usually remain asymptomatic and are at most detected as an incidental finding. The plica synovialis mediopatellaris(medial shelf) is the one that most frequently leads to disorders because it is located in an easily irritated area. For more information on the disorders caused by plicae, see plica syndrome.
Pathology
The knee is a region with a very high density of entities. Here are some diseases of the joint:
Important misalignments of the knee are
- genu vargum (bow leg), also unilateral
- genu valgum (X-leg), also unilateral
- genu flexum (non-extensible knee, also: genu procurvatum, extension deficit)
- genu recurvatum (knee hyperextended by more than 5°)
In the case of knee injuries, it is helpful to know the direction, duration and strength of the force applied as well as the position of the knee. In the case of diseases, a careful medical history and corresponding functional tests are important. The following are some of the more common entities or disorders of the knee joint:
- Osgood-Schlatter disease is a typical disease of the knee in adolescents with pain in the area of the tibial tuberosity, especially during jumping sports
- Patellar tendinitis (jumper’s knee) is a typical condition of older adolescents/young adults
- Degenerative meniscopathies/damage to the menisci occur from young adulthood onwards, possibly with incarcerations
- Gonarthrosis, i.e. osteoarthritis of the knee joint. See also the article on cartilage damage in the knee joint
- Chondropathia patellae
- Retropatellar arthrosis, possibly with a feeling of instability, is particularly painful when climbing stairs or walking downhill and is noticeable by rubbing; the knee may be swollen at the same time
- Diffuse knee pain without causative trauma is often the result of meniscus degeneration or osteoarthritis, often with signs of inflammation, swelling, overheating
- Baker’s cysts become noticeable through pain or a popliteal foreign body sensation, the neighboring joints hip joint, SI joint, ankle/foot can be involved or causative, anatomical and functional leg length discrepancies can be the cause
- Knee joint swelling can be synovial (more than the physiological 2 ml, usually after overloading, only slight overheating, self-resolving within days) or bloody (hemarthrosis, usually traumatic, bulging, painful swelling, overheating).
- Infections in the joint show marked overheating and redness, bulging, clearly painful effusion, painfully restricted movement.
- Tearing, tearing or overstretching of one or more ligaments: outer ligament, inner ligament, anterior or posterior cruciate ligament
- Psoriatic arthritis
- Perthes‘ disease and consequential damage to the knee
- Gout
- Baker’s cyst
- Rheumatoid arthritis (RA)/chronic polyarthritis (CP) (also: true „rheumatism“)
- more rarely: impingement
- Mobrus ankylosing spondylitis
- Secondary conditions in pathology of the foot
- Plica syndrome
- Runner’s knee/ITBS (Iliotibial Band Syndrome)
- Hoffa syndrome
Note the other health conditions with regard to secondary genupathies, such as those caused by Lyme disease.
Pathology of the femoropatellar joint
- Patellofemoral knee pain usually increases with strain, especially when descending stairs and sitting for long periods. If the pain continues to worsen under strain, this is indicative of cartilage damage; symptoms that first improve and then worsen later are more likely to indicate a muscle/tendon problem(quadriceps tendon, lig. patellae).
- Patellar luxation can show joint effusions, sometimes the medial retinaculum tears
- Patellar subluxation
- Patella baja (low position), possibly as a result of patella fractures or quadriceps tendon rupture
- Patella alta (high patella ), usually traumatic with rupture
- Patellar lateralization
- Excessive pronation rotates the tibia inwards and stresses the peripatellar soft tissue structures, causing ventral knee pain
When the quadriceps are not tensed, the patella is slightly lateralized. With tension and further flexion, it medializes and enters the trochlear gliding bearing. Unstable kneecaps and patellae altae only enter the gliding bearing with further flexion. All patellar malalignments lead to ventral peripatellar pain with tendinopathy and retropatellar cartilage changes, including an altered leg axis
Tests
Tests of the knee joint
Meniscus
- Joint Line Tenderness Palpation
- Thessaly test
- Apley grinding test
- Steinmann 1 sign
- Steinmann 2 sign
- Payr-sign (medial meniscus)
- McMurray test
- Childress test/Duck-walk test
- Merke sign
- Eges test
- Paessler-rotation-compression test
- Jump-Sign / Finochietto test
- Tschaklin sign
- Turner sign
- Chabot test
Medial collateral ligament
Lateral collateral ligament
Cruciate ligaments
- Lelli-Test (Ruptur des ACL)
- (Lateral) Pivot-Shift-Test (MacIntosh) (hyperextension or rupture of the ACL)
- Lachmann-(-Trillat / Ritchie-)Test (ACL)
- reversed Pivot-Shift-Test (PCL)
- Schubladen (drawer) Test (ACL and PCL)
- Gravity-Sign (posterior sag test, Godfrey-Test) (PCL)
- Marten-Test (Insufficiency of the ACL)
- Quadriceps Active Test / Active Drawer Test (PCL)
- Hyperextensions-Test (PCL)
ITBS (Runners knee)
IT-Band (Tractus iliotibialis) Verkürzung
Chondropathia patellae
Patella mixed
Hoffa-syndrome
Joint effusion
Q-angle
(Posterolateral Instability)
Patellaluxation/-subluxation
- Fairbank apprehension test (Smilie-Test)
- McConnell test
- Tilt test (tension of the lateral retinaculum)
- Subluxation suppression test
Plica-Syndrom
mixed
- Fründ sign (chondropathia patellae, retropatellar arthrosis, patella fracture)
- Böhler sign (menisci, collateral ligament damage)
- Dreyer test (patella fracture, Quadrizepssehnenriß)
Tests of the movement directions
Tests of the spanning muscles
Quadrizeps
Hamstrings
Images
Knee from dorsal, ligaments
Knee from dorsal
Knee from dorsal, capsule
Knee from ventral
Knee from ventrolateral
Knee from lateral
Knee transversal
Knee, saggital
ventral view in 90° flexion (image links to linkmap)

Lateral view in 45° flexion with expanded bursae (image links to linkmap)
Menisci on tibia from cranial (image links to linkmap)
Menisci with loaded rotation (image links to linkmap)